Abstract
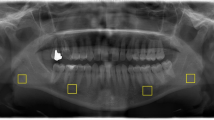
Patients with Osteogenesis Imperfecta (OI) present extra-skeletal manifestations, including important orodental and craniofacial features as dentinogenesis imperfecta, dental agenesis, failure of maxilla growth and hypotonia of masticatory muscles. These features may compromise vital functions speech and mastication. Studies have demonstrated that cyclic pamidronate infusion, the standard therapy for patients with moderate to severe OI, influences the histomorphometric pattern of different body bones. The present study aimed to investigate the condyle trabecular bone pattern in OI patients. We used fractal dimension (FD) analysis on dental panoramic radiographic images to characterize the mandibular condyle trabecular bone in adolescents diagnosed with OI and treated with pamidronate. Imaging exam of 33 adolescents of both sexes, aged between 12 and 17 years, were analyzed and compared with 99 age- and sex-matched healthy adolescents. FD in patients was significantly lower (1.23 ± 0.15) than in healthy controls (1.29 ± 0.11; p < 0.01). Type of OI, age at treatment onset, and the duration of therapy were variables that showed a statistically significant effect on the FD results. This study demonstrated that the bone architecture of mandibular condyles may be altered in pediatric patients with moderate and severe forms of OI. Also, pamidronate treatment seems to have a positive effect on condyle trabecular bone in these patients. This is supported by our finding that FD values were positively influenced by the length of cyclic pamidronate treatment at the time of imaging, as well as by the age of the individual at treatment onset.


Similar content being viewed by others
Data Availability
The authors declare that all data and materials support their published information and comply with filed standards.
Code Availability
Not applicable.
References
Rauch F, Glorieux FH (2004) Osteogenesis imperfecta. Lancet 24:1377–1385. https://doi.org/10.1016/S0140-6736(04)16051-0
Trejo P, Rauch F (2016) Osteogenesis imperfecta in children and adolescents—new developments in diagnosis and treatment. Osteoporos Int 27:3427–3437. https://doi.org/10.1007/s00198-016-3723-3
Marini JC, Dang Do AN. Osteogenesis Imperfecta. [Updated 2020 Jul 26]. In: Feingold KR, Anawalt B, Boyce A, et al., editors. Endotext [Internet]. South Dartmouth (MA): MDText.com I. 2000. A from: https://www.ncbi.nlm.nih.gov/books/NBK279109. (2020) Osteogenesis Imperfecta. MDText.com
Marini JC, Forlino A, Bächinger HP et al (2017) Osteogenesis imperfecta. Nat Rev Dis Prim. https://doi.org/10.1038/nrdp.2017.52
Forlino A, Marini JC (2016) Osteogenesis imperfecta. Lancet 387:1657–1671. https://doi.org/10.1016/S0140-6736(15)00728-X
Sillence DO, Rimoin DL (1978) Classification of osteogenesis imperfecta. Lancet 311:1041–1042. https://doi.org/10.1016/S0140-6736(78)90763-8
Bonafe L, Cormier-Daire V, Hall C et al (2015) Nosology and classification of genetic skeletal disorders: 2015 revision. Am J Med Genet Part A 167:2869–2892. https://doi.org/10.1002/ajmg.a.37365
Mortier GR, Cohn DH, Cormier-Daire V et al (2019) Nosology and classification of genetic skeletal disorders: 2019 revision. Am J Med Genet Part A 179:2393–2419. https://doi.org/10.1002/ajmg.a.61366
Van Dijk FS, Sillence DO (2014) Osteogenesis imperfecta: clinical diagnosis, nomenclature and severity assessment. Am J Med Genet Part A 164:1470–1481. https://doi.org/10.1002/ajmg.a.36545
Schwartz S, Tsipouras P (1984) Oral findings in osteogenesis imperfecta. Oral Surg Oral Med Oral Pathol 57:161–167. https://doi.org/10.1016/0030-4220(84)90206-8
Waltimo J (1994) Hyperfibers and vesicles in dentin matrix in dentinogenesis imperfecta (Dl) associated with osteogenesis imperfecta (01). J Oral Pathol Med 23:389–389. https://doi.org/10.1111/j.1600-0714.1994.tb00082.x
Foster BL, Ramnitz MS, Gafni RI et al (2014) Rare bone diseases and their dental, oral, and craniofacial manifestations. J Dent Res 93:7S-19S. https://doi.org/10.1177/0022034514529150
Malmgren B, Tsilingaridis G, Monsef-Johansson N et al (2020) Bisphosphonate therapy and tooth development in children and adolescents with osteogenesis imperfecta. Calcif Tissue Int 107:143–150. https://doi.org/10.1007/s00223-020-00707-1
Chetty M, Roberts TS, Stephen L, Beighton P (2017) Craniofacial manifestations in osteogenesis imperfecta type III in South Africa. BDJ Open 3:1–5. https://doi.org/10.1038/bdjopen.2017.21
Bendixen KH, Gjørup H, Baad-Hansen L et al (2018) Temporomandibular disorders and psychosocial status in osteogenesis imperfect—a cross-sectional study. BMC Oral Health 18:6–13. https://doi.org/10.1186/s12903-018-0497-3
Ortega ADOL, Rosa VLM, Figueiredo Zwir LML et al (2007) Anatomic and dynamic aspects of stomatognathic structures in osteogenesis imperfecta: a case report. Cranio J Craniomandib Pract 25:144–149. https://doi.org/10.1179/crn.2007.022
Rauch F, Travers R, Parfitt AM, Glorieux FH (2000) Static and dynamic bone histomorphometry in children with osteogenesis imperfecta. Bone 26:581–589. https://doi.org/10.1016/S8756-3282(00)00269-6
Rauch F, Travers R, Plotkin H, Glorieux FH (2002) The effects of intravenous pamidronate on the bone tissue of children and adolescents with osteogenesis imperfecta. J Clin Invest 110:1293–1299. https://doi.org/10.1172/JCI0215952
Land C, Rauch F, Travers R, Glorieux FH (2007) Osteogenesis imperfecta type VI in childhood and adolescence: effects of cyclical intravenous pamidronate treatment. Bone 40:638–644. https://doi.org/10.1016/j.bone.2006.10.010
Palomo T, Fassier F, Ouellet J et al (2015) Intravenous bisphosphonate therapy of young children with osteogenesis imperfecta: skeletal findings during follow up throughout the growing years. J Bone Miner Res 30:2150–2157. https://doi.org/10.1002/jbmr.2567
Pinheiro B, Zambrano MB, Vanz AP et al (2019) Cyclic pamidronate treatment for osteogenesis imperfecta: report from a brazilian reference center. Genet Mol Biol 42:252–260. https://doi.org/10.1590/1678-4685-gmb-2018-0097
Apolinário AC, Figueiredo PT, Guimarães AT et al (2015) Pamidronate affects the mandibular cortex of children with osteogenesis imperfecta. J Dent Res 94:95S-102S. https://doi.org/10.1177/0022034514567334
Apolinario AC, Sindeaux R, De Souza Figueiredo PT et al (2016) Dental panoramic indices and fractal dimension measurements in osteogenesis imperfecta children under pamidronate treatment. Dentomaxillofacial Radiol 45:1–9. https://doi.org/10.1259/dmfr.20150400
Marçal FF, Ribeiro EM, Costa FWG et al (2019) Dental alterations on panoramic radiographs of patients with osteogenesis imperfecta in relation to clinical diagnosis, severity, and bisphosphonate regimen aspects: a STROBE-compliant case-control study. Oral Surg Oral Med Oral Pathol Oral Radiol 128:621–630. https://doi.org/10.1016/j.oooo.2019.07.001
Marginean O, Tamasanu C, Mang N et al (2017) Therapy with pamidronate in children with osteogenesis imperfecta. Drug Des Dev Ther 11:2507
Pachêco-Pereira C, Almeida FT, Chavda S et al (2019) Dental imaging of trabecular bone structure for systemic disorder screening: a systematic review. Oral Dis 25:1009–1026. https://doi.org/10.1111/odi.12950
Aktuna Belgin C, Serindere G (2020) Fractal and radiomorphometric analysis of mandibular bone changes in patients undergoing intravenous corticosteroid therapy. Oral Surg Oral Med Oral Pathol Oral Radiol 130:110–115. https://doi.org/10.1016/j.oooo.2019.12.009
Şahin O, Odabaşı O, Demiralp KÖ et al (2019) Comparison of findings of radiographic and fractal dimension analyses on panoramic radiographs of patients with early-stage and advanced-stage medication-related osteonecrosis of the jaw. Oral Surg Oral Med Oral Pathol Oral Radiol 128:78–86. https://doi.org/10.1016/j.oooo.2019.03.002
Neves FS, Barros AS, Cerqueira GA et al (2020) Assessment of fractal dimension and panoramic radiomorphometric indices in women with celiac disease. Oral Radiol 36:141–147. https://doi.org/10.1007/s11282-019-00388-z
Baksi BG, Fidler A (2011) Fractal analysis of periapical bone from lossy compressed radiographs: a comparison of two lossy compression methods. J Digit Imaging 24:993–998. https://doi.org/10.1007/s10278-011-9383-0
Toghyani S, Nasseh I, Aoun G, Noujeim M (2019) Effect of image resolution and compression on fractal analysis of the periapical bone. Acta Inform Medica 27:167–170. https://doi.org/10.5455/aim.2019.27.167-170
Bollen AM, Taguchi A, Hujoel PP, Hollender LG (2001) Fractal dimension on dental radiographs. Dentomaxillofacial Radiol 30:270–275. https://doi.org/10.1038/sj.dmfr.4600630
Law AN, Bollen AM, Chen SK (1996) Detecting osteoporosis using dental radiographs: a comparison of four methods. J Am Dent Assoc 127:1734–1742. https://doi.org/10.14219/jada.archive.1996.0134
Arsan B, Köse TE, Çene E, Özcan İ (2017) Assessment of the trabecular structure of mandibular condyles in patients with temporomandibular disorders using fractal analysis. Oral Surg Oral Med Oral Pathol Oral Radiol 123:382–391. https://doi.org/10.1016/j.oooo.2016.11.005
Rasband WS (2018) ImageJ. U. S. National Institutes of Health, Bethesda, Maryland, USA. https://imagej.nih.gov/ij/.
Sindeaux R, Figueiredo PTDS, De Melo NS et al (2014) Fractal dimension and mandibular cortical width in normal and osteoporotic men and women. Maturitas 77:142–148. https://doi.org/10.1016/j.maturitas.2013.10.011
White SC, Rudolph DJ (1999) Alterations of the trabecular pattern of the jaws in patients with osteoporosis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 88:628–635. https://doi.org/10.1016/S1079-2104(99)70097-1
Smartt JM, Low DW, Bartlett SP (2005) The pediatric mandible: I. A primer on growth and development. Plast Reconstr Surg 116:258. https://doi.org/10.1097/01.prs.0000169940.69315.9c
Karlo CA, Stolzmann P, Habernig S et al (2010) Size, shape and age-related changes of the mandibular condyle during childhood. Eur Radiol 20:2512–2517. https://doi.org/10.1007/s00330-010-1828-1
Bender ME, Lipin RB, Goudy SL (2018) Development of the pediatric temporomandibular joint. Oral Maxillofac Surg Clin North Am 30:1–9. https://doi.org/10.1016/j.coms.2017.09.002
Malmgren B, Thesleff I, Dahllöf G et al (2021) Abnormalities in tooth formation after early bisphosphonate treatment in children with osteogenesis imperfecta. Calcif Tissue Int. https://doi.org/10.1007/s00223-021-00835-2
Oliveira ML, Pedrosa EFNC, Cruz AD et al (2013) Relationship between bone mineral density and trabecular bone pattern in postmenopausal osteoporotic Brazilian women. Clin Oral Investig 17:1847–1853. https://doi.org/10.1007/s00784-012-0882-2
Parfitt AM, Travers R, Rauch F, Glorieux FH (2000) Structural and cellular changes during bone growth in healthy children. Bone 27:487–494. https://doi.org/10.1016/S8756-3282(00)00353-7
Hegde S, Praveen B, Shetty SR (2013) Morphological and radiological variations of mandibular condyles in health and diseases: a systematic review. Dentistry 03:1–5. https://doi.org/10.4172/2161-1122.1000154
Dwan K, Ca P, Rd S, Basel D (2016) Bisphosphonate therapy for osteogenesis imperfecta (review). Cochrane Libr. https://doi.org/10.1002/14651858.CD005088.pub4
Chagas CEA, Roque JP, Santarosa Emo Peters B et al (2012) Do patients with osteogenesis imperfecta need individualized nutritional support? Nutrition 28:138–142. https://doi.org/10.1016/j.nut.2011.04.003
Funding
The author Pantoja, LLQ was supported by Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES), Ministry of Education, Brazil. This study was supported by a CAPES/COFECUB grant (#918/2018). The authors thank the Department of Research and Innovation, University of Brasilia, Brazil. The funding agencies have no role in the submitted work.
Author information
Authors and Affiliations
Contributions
LLQP: Contributed to conception, design, data acquisition and interpretation, performed statistical analyses, drafted and critically revised the manuscript. ML: Contributed to data acquisition and interpretation, performed statistical analyses, drafted, and critically revised the manuscript. PMY: Contributed to design, and critically revised the manuscript. LSR: Contributed to design, and critically revised the manuscript. AFL: Contributed to conception, design, data interpretation, revised statistical analyses, and critically revised the manuscript. PTSF: Contributed to design, data interpretation, and critically revised the manuscript. LCC: Contributed to conception, design, data analysis and interpretation, and critically revised the manuscript. ACA: Contributed to conception, design, data analysis and interpretation, drafted and critically revised the manuscript. All authors gave their final approval and agreed to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of Interest
Leticia L. Quirino Pantoja, Mariana Lustosa, Paulo Márcio Yamaguti, Lídia S. Rosa, André Ferreira Leite, Paulo Tadeu S. Figueiredo, Luiz Claudio Castro and Ana Carolina Acevedo declare no potential conflicts of interest with respect to the authorship and/or publication of this article.
Human and Animal Rights and Informed Consent statements
This study was developed at the University Hospital of Brasília (HUB) and approved by the Human Research Ethics Committee of the University of Brasília School of Health Sciences (registration number 15367519.8.0000.0030). Parents or legal guardians of all subjects participating in the study signed an Informed Consent Form, in which they agreed to participate in the research. Parents or legal guardians of all subjects participating in the study signed an Informed Consent Form, in which they allowed publication of data and images.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pantoja, L.L.Q., Lustosa, M., Yamaguti, P.M. et al. Pamidronate Therapy Increases Trabecular Bone Complexity of Mandibular Condyles in Individuals with Osteogenesis Imperfecta. Calcif Tissue Int 110, 303–312 (2022). https://doi.org/10.1007/s00223-021-00915-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-021-00915-3