Abstract
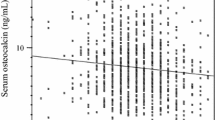
Osteocalcin acts as an endocrine hormone to regulate energy homeostasis. Although several in vivo and in vitro studies suggest that osteocalcin is involved in chronic inflammation, the association between osteocalcin and chronic inflammation in humans is unknown. In this cross-sectional study, 246 patients with type 2 diabetes mellitus (T2DM) were recruited to investigate the association of bone turnover markers with chronic inflammation parameters such as high-sensitive C-reactive protein (hsCRP), ferritin, and leukocyte subtype counts. Bone-specific alkaline phosphatase (BAP), total osteocalcin (OC), undercarboxylated OC (ucOC), and urinary N-terminal cross-linked telopeptide of type-I collagen (uNTX) were measured. Multiple regression analysis adjusted for age, duration of diabetes, body mass index, estimated glomerular filtration rate, and hemoglobin A1c showed that serum OC levels were significantly and negatively associated with hsCRP, ferritin, basophil count, and monocyte count (β = − 0.18, p = 0.013; β = − 0.22, p = 0.031; β = − 0.14, p = 0.038; and β = − 0.17, p = 0.012, respectively). Moreover, serum ucOC levels were significantly and negatively associated with hsCRP, ferritin, total leukocyte count, neutrophil count, and monocyte count (β = − 0.24, p = 0.007; β =− 0.37, p = 0.003; β = − 0.21, p = 0.007; β = − 0.24, p = 0.002; and β = − 0.20, p = 0.011, respectively). The ratio of ucOC to OC was significantly and negatively associated with ferritin (β = − 0.31, p = 0.014). However, neither BAP nor uNTX was associated with any chronic inflammation parameters. This is the first study to show that serum OC and ucOC levels were negatively associated with chronic inflammation parameters such as hsCRP, ferritin, and leukocyte subtypes in patients with T2DM. Therefore, OC could be a therapeutic target for protecting against chronic inflammation.
Similar content being viewed by others
References
Wei J, Karsenty G (2015) An overview of the metabolic functions of osteocalcin. Curr Osteoporos Rep 13:180–185
Kanazawa I (2017) Interaction between bone and glucose metabolism. Endocr J 64:1043–1053
Lee NK, Sowa H, Hinoi E, Ferron M, Ahn JD, Confavreux C, Dacquin R, Mee PJ, McKee MD, Jung DY, Zhang Z, Kim JK, Mauvais-Jarvis F, Ducy P, Karsenty G (2007) Endocrine regulation of energy metabolism by the skeleton. Cell 130:456–469
Mizokami A, Yasutake Y, Higashi S, Kawakubo-Yasukochi T, Chishaki S, Takahashi I, Takeuchi H, Hirata M (2014) Oral administration of osteocalcin improves glucose utilization by stimulating glucagon-like pepride-1 secretion. Bone 69:68–79
Tsuka S, Aonuma F, Higashi S, Ohsumi T, Nagano K, Mizokami A, Kawakubo-Yasukochi T, Masaki C, Hosokawa R, Hirata M, Takeuchi H (2015) Promotion of insulin-induced glucose uptake in C2C12 myotubes by osteocalcin. Biochem Biophys Res Commun 459:437–442
Otani T, Mizokami A, Hayashi Y, Gao J, Mori Y, Nakamura S, Takeuchi H, Hirata M (2015) Signaling pathway for adiponectin expression in adipocytes by osteocalcin. Cell Signal 27:532–544
Kanazawa I, Yamaguchi T, Yamamoto M, Yamauchi M, Kurioka S, Yano S, Sugimoto T (2009) Serum osteocalcin level is associated with glucose metabolism and atherosclerosis parameters in type 2 diabetes mellitus. J Clin Endocrinol Metab 94:45–49
Kanazawa I, Yamaguchi T, Tada Y, Yamauchi M, Yano S, Sugimoto T (2011) Serum osteocalcin level is positively associated with insulin sensitivity and secretion in patients with type 2 diabetes. Bone 48:720–725
Kanazawa I, Yamaguchi T, Yamauchi M, Yamamoto M, Kurioka S, Yano S, Sugimoto T (2011) Serum undercarboxylated osteocalcin was inversely associated with plasma glucose level and fat mass in type 2 diabetes mellitus. Osteoporos Int 22:187–194
Iki M, Tamaki J, Fujita Y, Kouda K, Yura A, Kadowaki E, Sato Y, Moon JS, Tomioka K, Okamoto N, Kurumatani N (2012) Serum undercarboxylated osteocalcin levels are inversely associated with glycemic status and insulin resistance in an elderly Japanese male population: Fujiwara-kyo osteoporosis Risk in Men (FORMEN) Study. Osteoporos Int 23:761–770
Kannel WB, McGee DL (1979) Diabetes and cardiovascular disease. The Framingham study. JAMA 241:2035–2038
Vestergaard P (2007) Discrepancies in bone mineral density and fracture risk in patients with type 1 and type 2 diabetes—a meta-analysis. Osteoporos Int 18:427–444
Wang J, You W, Jing Z, Wang R, Fu Z, Wang Y (2016) Increased risk of vertebral fracture in patients with diabetes: a meta-analysis of cohort studies. Int Orthop 40:1299–1307
Hygum K, Starup-Linde J, Harslof T, Vestergaard P, Langdahl BL (2017) Diabetes mellitus, a state of low bone turnover –a systematic review and meta-analysis. Eur J Endocrinol 176:R137–R157
Kanazawa I, Sugimoto T. Diabetes mellitus-induced bone fragility. Intern Med (in press)
Kunutsor SK, Apekey TA, Laukkanen JA (2015) Association of serum total osteocalcin with type 2 diabetes and intermediate metabolic phenotypes: systematic review and meta-analysis of observational evidence. Eur J Epidemiol 30:599–614
Lerchbaum E, Schwetz V, Pilz S, Grammer TB, Look M, Boehm BO, Obermayer-Pietsch B, Marz W (2013) Association of bone turnover markers with mortality in men referred to coronary angiography. Osteoporos Int 24:1321–1332
Lerchbaum E, Schwetz V, Pilz S, Boehm BO, Marz W (2014) Association of bone turnover markers with mortality referred to coronary angiography: the Ludwigshafen Risk and Cardiovascular Health (LURIC) study. Osteoporos Int 25:455–465
Miyake H, Kanazawa I, Sugimoto T (2018) Association of bone mineral density, bone turnover markers, and vertebral fractures with all-cause mortality in type 2 diabetes mellitus. Calcif Tissue Int 102:1–13
Zhou B, Li H, Liu J, Xu L, Zang W, Wu S, Sun H (2013) Intermittent injections of osteocalcin reverse autophagic dysfunction and endoplasmic reticulum stress resulting from diet-induced obesity in the vascular tissue via the NFκB-p65-dependent mechanism. Cell Cycle 12:1901–1913
Jung CH, Lee WJ, Hwang JY, Lee MJ, Seol SM, Kim YM, Lee YL, Park JY (2013) The preventive effect of uncarboxylated osteocalcin against free fatty acid-induced endothelial apoptosis through the activation of phosphatidylinositol 3-kinase/Akt signaling pathway. Metabolism 62:1250–1257
Dou J, Li H, Ma X, Zhang M, Fang Q, Nie M, Bao Y, Jia W (2014) Osteocalcin attenuates high fat diet-induced impairment of endothelium-dependent relaxation through Akt/eNOS-dependent pathway. Cardiovasc Diabetol 13:74
Kolb H, Mandrup-Poulsen T (2010) The global diabetes epidemic as a consequence of lifestyle-induced low-grade inflammation. Diabetologia 53:10–20
Pollack RM, Donath MY, LeRoith D, Leibowitz G (2016) Anti-inflammatory agents in the treatment of diabetes and its vascular complications. Diabetes Care 39:S244–S252
Patel PS, Buras ED, Balasubramanyam A (2013) The role of the immune system in obesity and insulin resistance. J Obes 2013:616193
Pickering RJ, Rosado CJ, Sharma A, Buksh S, Tate M, de Haan JB (2018) Recent novel approaches to limit oxidative stress and inflammation in diabetic complications. Clin Transl Immunology 7:e1016
Hill HS, Gram J, Walton RG, Liu J, Moellering DR, Garvey WT (2014) Carboxylated and undercarboxylated forms of osteocalcin directly modulate the glucose transport system and inflammation in adipocytes. Horm Metab Res 46:341–347
Guedes JAC, Esteves JV, Morais MR, Zorn TM, Furuya DT. Osteocalcin improves insulin resistance and inflammation in obese mice: participation of white adipose tissue and bone. Bone. https://doi.org/10.1016/j.bone.2017.11.020
Polonskaya YV, Kashtanove EV, Murashov IS, Volkov AM, Kurguzov AV, Chernyavsky AM, Ragino YI (2017) Associations of osteocalcin, osteoprotegerin, and calcitonin with inflammation biomarkers in atherosclerotic plaques of coronary arteries. Bull Exp Biol Med 162:726–729
Imai E, Horibe M (2008) Evaluation of kidney function. Nippon Naika Gakkai Zasshi 97:921–928 (in Japanese)
Pittas AG, Harris SS, Eliades M, Stark P, Dawson-Hughes B (2009) Association between serum osteocalcin and markers of metabolic phenotype. J Clin Endocrinol Metab 94:827–832
Chen L, Li Q, Yang Z, Ye Z, Huang Y, He M, Wen J, Wang X, Lu B, Hu J, Liu C, Ling C, Qu S, Hu R (2013) osteocalcin, glucose metabolism, lipid profile and chronic low-grade inflammation in middle-aged and elderly Chinese. Diabet Med 30:309–317
Sarkar PD, Choudhury AB (2013) Relationships between serum osteocalcin levels versus blood glucose, insulin resistance and markers of systemic inflammation in central Indian type 2 diabetic patients. Eur Rev Med Pharmacol Sci 17:1631–1635
Bonneau J, Ferland G, Karelis AD, Doucet E, Faraj M, Rabasa-Lhoret R, Ferron M (2017) Association between osteocalcin gamma-carboxylation and insulin resistance in overweight and obese postmenopausal women. J Diabetes Complicat 31:1027–1034
Razny U, Fedak D, Kiec-Wilk B, Goralska J, Gruca A, Zdzienicka A, Kiec-Klimczak M, Solnica B, Hubalewska-Dydejczyk A, Malczewska-Malec M (2017) Carboxylated and undercarboxylated osteocalcin in metabolic complications of human obesity and prediabetes. Diabetes Metab Res Rev 33:2862
Garielsen JS, Gao Y, Simcox JA, Huang J, Thorup D, Jones D, Cooksey RC, Gabrielsen D, Adams TD, Hunt SC, Hopkins PN, Cefalu WT, McClain DA (2012) Adipocyte iron regulated adiponectin and insulin sensitivity. J Clin Invest 122:3529–3540
Wlazlo N, van Greevenbroek MM, Ferreira I, Jansen EH, Feskens EJ, vander Kallen CJ, Schalkwijk CG, Bravenboer B, Stehouwer CD (2013) Iron metabolism is associated with adipocyte insulin resistance and plasma adiponectin: the Cohort on Diabetes and Atherosclerosis Maastricht (CODAM) study. Diabetes Care 36:309–315
Torti FM, Torti SV (2002) Regulation of ferritin genes and protein. Blood 99:3505–3516
Sharif K, Vieira Borba V, Zandman-Goddard G, Shoenfeld Y (2018) Ferritin is essential in modulating inflammation. Clin Exp Immunol 191:149–150
Ruddell RG, Hoang-Le D, Barwood JM, Ruthrford PS, Piva TJ, Watters DJ, Santambrogio P, Arosio P, Ramm GA (2009) Ferritin functions as a proinflammatory cytokine via iron-independent protein kinase C zeta/nuclear factor kappaB-regulated signaling in rat hepatic stellate cells. Hepatology 49:887–900
Friedman GD, Klatsky AL, Siegelaub AB (1974) The leukocyte count as a predictor of myocardial infarction. N Engl J Med 290:1275–1278
Kavousi M, Elias-Smale S, Rutten JH, Leening MJ, Vliegenthart R, Verwoert GC, Krestin GP, Oudkerk M, de Maat MP, Leebeek FW, Mattace-Raso FU, Lindemans J, Hofman A, Steyerberg EW, van der Lugt A, van den Meiracker AH, Witteman JC (2012) Evaluation of newer risk markers for coronary heart disease risk classification: a cohort study. Ann Intern Med 156:438–444
Olivares R, Ducimetiere P, Claude JR (1993) Monocyte count: a risk factor for coronary heart disease? Am J Epidemiol 137:49–53
Nagareddy PR, Murphy AJ, Stirzaker RA, Hu Y, Yu S, Miller RG, Ramkhelawan B, Distel E, Westerterp M, Huang LS, Schmidt AM, Orchard TJ, Fishwe EA, Tall AR, Goldberg IJ (2013) Hyperglycemia promotes myelopoiesis and impairs the resolution of atherosclerosis. Cell Metab 17:695–708
Rossol M, Pierer M, Raulien N, Quandt D, Meusch U, Rothe K, Schubert K, Schoneberg T, Schaefer M, Krugel U, Smajilovic S, Brauner-Osborne H, Baerwald C, Wagner U (2012) Extracellular Ca2 + is a danger signal activating the NLRP3 inflammasome through G protein-coupled calcium sensing receptors. Nat Commun 3:1329
Adamopoulos IE (2018) Inflammation in bone physiology and pathology. Curr Opin Rheumatol 30:59–64
Calvi LM, Adams GB, Weibrecht KW, Weber JM, Olson DP, Knight MC, Martin RP, Schipani E, Divieti P, Bringhurst FR, Milner LA, Kronenberg HM, Scadden DT (2003) Osteoblastic cells regulate the haematopoietic stem cell niche. Nature 425:841–846
Zhang J, Niu C, Ye L, Huang H, He X, Tong WG, Ross J, Haug J, Johnson T, Feng JQ, Harris S, Wiedemann LM, Mishina Y, Li L (2003) Identification of the haematopoietic stem cell niche and control of the niche size. Nature 425:836–841
Torrens JI, Skurnick J, Davidow AL, Korenman SG, Santoro N, Soto-Greene M, Lasser N, Weiss G, Study of Women’s Health Across the Nation (SWAN) (2004) Ethnic differences in insulin sensitivity and beta-cell function in premenopaulsa or early perimenopausal women without diabetes: the Study of Women’s Health Across the Nation (SWAN). Diabetes Care 27: 354–361
Acknowledgements
This study was partly supported by research grant from Eli Lilly Japan.
Author information
Authors and Affiliations
Contributions
Study design and conduct: IK. Collected and analyzed the data: IK and ST. wrote the paper: IK and TS. Approving final version: All authors. IK takes responsibility for the integrity of the data analysis.
Corresponding author
Ethics declarations
Conflict of interest
Ippei Kanazawa, Sayuri Tanaka, and Toshitsugu Sugimoto declare that they have no conflicts of interest.
Human and Animal Rights and Informed Consent
This study was approved by IRB of our university and informed consent was waived because no intervention and further examinations were performed.
Rights and permissions
About this article
Cite this article
Kanazawa, I., Tanaka, S. & Sugimoto, T. The Association Between Osteocalcin and Chronic Inflammation in Patients with Type 2 Diabetes Mellitus. Calcif Tissue Int 103, 599–605 (2018). https://doi.org/10.1007/s00223-018-0460-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-018-0460-y