Abstract
Rationale
Aberrations in the stress response are associated with posttraumatic stress disorder (PTSD) symptom development, maintenance, and severity. Gamma-aminobutyric acid (GABA), the brain’s primary inhibitory neurotransmitter, may play a key role in stress recovery.
Objectives
In this preliminary study, we examined whether plasma GABA levels differed between women with PTSD and trauma-exposed healthy controls.
Methods
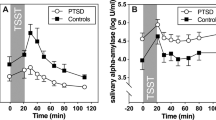
Thirty participants provided plasma samples during two phases of the menstrual cycle: the early follicular phase and the mid-luteal phase. During each phase, blood was drawn after 45 min of rest, and after mild and moderately stressful psychophysiological tasks. Plasma GABA levels were measured using HPLC-mass spectrometry (LC-MS/MS).
Results
In analyses using PTSD diagnosis as a categorical group variable, women with and without a diagnosis of PTSD did not differ in plasma GABA levels (ps > .18). However, in analyses examining PTSD symptom severity as a continuous variable, there was a trend-level positive association between more severe PTSD symptoms and higher plasma GABA levels across the four blood draws (p = .06). In analyses examining DSM-IV PTSD symptom clusters separately, dysphoria symptoms were positively and significantly associated with plasma GABA levels (p = .03). Similarly, there was a trend-level positive association between avoidance cluster symptoms and plasma GABA levels (p = .06). Plasma GABA levels were not modulated by experimentally induced stress or menstrual cycle phase.
Conclusions
Dysregulation in GABA may be a neurobiological marker and/or potential treatment target for women with PTSD symptom profiles characterized by prominent dysphoria and avoidance cluster symptoms.

Similar content being viewed by others
Notes
To explore the potential contribution of depression to study results, we examined differences in baseline GABA levels between individuals with and without a comorbid depressive disorder diagnosis. In the full sample (n = 30) of PTSD and TC participants, individuals with and without a depressive disorder did not differ significantly in their baseline GABA levels during either the eFP, t (5.18) = 1.11, p = .31, or the mLP, t (27) = .66, p = .52, menstrual cycle phase. Similarly, when PTSD participants with depression (n = 6) were compared to PTSD participants without depression (n = 9), no differences in baseline GABA levels were observed (eFP: t (13) = .70, p = .50; mLP: t (11) = 1.04, p = .32).
References
Al-Sarraf H (2002) Transport of 14C-γ-aminobutyric acid into brain, cerebrospinal fluid and choroid plexus in neonatal and adult rats. Dev Brain Res. https://doi.org/10.1016/S0165-3806(02)00537-0
American Psychiatric Association (2000) Diagnostic and statistical manual of mental disorders, 4th edn. Author, Washington, DC
Berrettini WH, Nurnberger JI, Hare T, Gershon ES, Post RM (1982) Plasma and CSF GABA in affective illness. Br J Psychiatry 141:483–487
Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, Keane TM (1995) The development of a Clinician-Administered PTSD Scale. J Trauma Stress 8:75–90
Boonstra E, de Kleijn R, Colzato LS, Alkemade A, Forstmann BU, Nieuwenhuis S (2015) Neurotransmitters as food supplements: the effects of GABA on brain and behavior. Front Psychol 6:1520
Crowley SK, Girdler SS (2014) Neurosteroid, GABAergic and hypothalamic pituitary adrenal (HPA) axis regulation: what is the current state of knowledge in humans? Psychopharmacology 231:3619–3634
de Groote L, Linthorst AC (2007) Exposure to novelty and forced swimming evoke stressor-dependent changes in extracellular GABA in the rat hippocampus. Neuroscience 148:794–805. https://doi.org/10.1016/j.neuroscience.2007.06.030
Epperson CN et al (2002) Cortical γ-aminobutyric acid levels across the menstrual cycle in healthy women and those with premenstrual dysphoric disorder: a proton magnetic resonance spectroscopy study. Arch Gen Psychiatry 59:851–858
Erdö SL, Wolff JR (1990) γ-Aminobutyric acid outside the mammalian brain. J Neurochem 54:363–372
Frey HH, Löscher W (1980) Cetyl GABA: effect on convulsant thresholds in mice and acute toxicity. Neuropharmacology 19:217–220. https://doi.org/10.1016/0028-3908(80)90141-0
Grillon C, Morgan CA, Southwick SM, Davis M, Charney DS (1996) Baseline startle amplitude and prepulse inhibition in Vietnam veterans with posttraumatic stress disorder. Psychiatry Res 64:169–178
Halbreich U, Petty F, Yonkers K, Kramer GL, Rush AJ, Bibi KW (1996) Low plasma gamma-aminobutyric acid levels during the late luteal phase of women with premenstrual dysphoric disorder. Am J Psychiatry 153:718–720
Heim C, Nemeroff CB (2016) Neurobiological pathways involved in fear, stress, and PTSD.
Kakee A, Takanaga H, Terasaki T, Naito M, Tsuruo T, Sugiyama Y (2001) Efflux of a suppressive neurotransmitter, GABA, across the blood-brain barrier. J Neurochem 79:110–118. https://doi.org/10.1046/j.1471-4159.2001.00540.x
Kazi AI, Oommen A (2014) Chronic noise stress-induced alterations of glutamate and gamma-aminobutyric acid and their metabolism in the rat brain. Noise Health 16:343
Kelmendi B, Adams TG, Yarnell S, Southwick S, Abdallah CG, Krystal JH (2016) PTSD: from neurobiology to pharmacological treatments. Eur J Psychotraumatol 7:31858
Kim BK, Fonda JR, Hauger RL, Pinna G, Anderson GM, Valovski IT, Rasmusson AM (2020) Composite contributions of cerebrospinal fluid GABAergic neurosteroids, neuropeptide Y and interleukin-6 to PTSD symptom severity in men with PTSD. Neurobiology of Stress:100220
Lambert JJ, Belelli D, Peden DR, Vardy AW, Peters JA (2003) Neurosteroid modulation of GABAA receptors. Prog Neurobiol 71:67–80
Meyerhoff DJ, Mon A, Metzler T, Neylan TC (2014) Cortical gamma-aminobutyric acid and glutamate in posttraumatic stress disorder and their relationships to self-reported sleep quality. Sleep 37:893–900. https://doi.org/10.5665/sleep.3654
Michels L, Schulte-Vels T, Schick M, O’Gorman RL, Zeffiro T, Hasler G, Mueller-Pfeiffer C (2014) Prefrontal GABA and glutathione imbalance in posttraumatic stress disorder: preliminary findings. Psychiatry Res 224:288–295. https://doi.org/10.1016/j.pscychresns.2014.09.007
Orr SP, Lasko NB, Shalev AY, Pitman RK (1995) Physiologic responses to loud tones in Vietnam veterans with posttraumatic stress disorder. J Abnorm Psychol 104:75–82. https://doi.org/10.1037/0021-843X.104.1.75
Orr SP, Metzger LJ, Lasko NB, Macklin ML, Peri T, Pitman RK (2000) De novo conditioning in trauma-exposed individuals with and without posttraumatic stress disorder. J Abnorm Psychol 109:290–298
Petroff OA (2002) Book review: GABA and glutamate in the human brain. Neuroscientist 8:562–573
Petty F, Kramer GL, Gullion CM, Rush AJ (1992) Low plasma γ-aminobutyric acid levels in male patients with depression. Biol Psychiatry 32:354–363
Pietrzak RH, Fredrickson A, Snyder PJ, Maruff P (2010) A comparison of statistical approaches used to evaluate change in cognitive function following pharmacologic challenge: an example with lorazepam. Hum Psychpharmacol Clin Exp 25:335–341. https://doi.org/10.1002/hup.1121
Pineles SL et al (2016a) Prepulse inhibition deficits in women with PTSD. Psychophysiol 53:1377–1385. https://doi.org/10.1111/psyp.12679
Pineles SL et al (2016b) Extinction retention and the menstrual cycle: different associations for women with posttraumatic stress disorder. J Abnorm Psychol 125:349–355. https://doi.org/10.1037/abn0000138
Pineles SL et al (2018) PTSD in women is associated with a block in conversion of progesterone to the GABAergic neurosteroids allopregnanolone and pregnanolone measured in plasma. Psychoneuroendocrinology 93:133–141
Pineles SL et al (2020) Associations between PTSD-Related extinction retention deficits in women and plasma steroids that modulate brain GABAA and NMDA receptor activity. Neurobiol Stress 13:100225
Pitman RK et al (2012) Biological studies of post-traumatic stress disorder. Nat Rev Neurosci 13:769
Puia G et al (1990) Neurosteroids act on recombinant human GABA A receptors. Neuron 4:759–765
Rasmusson AM, Pineles SL (2018) Neurotransmitter, peptide, and steroid hormone abnormalities in PTSD: biological endophenotypes relevant to treatment. Curr Psychiatry Rep 20:52
Rasmusson AM et al (2006) Decreased cerebrospinal fluid allopregnanolone levels in women with PTSD. Biol Psychiatry 60:704–713. https://doi.org/10.1016/j.biopsych.2006.03.026
Rasmusson AM et al (2019) Relationships between cerebrospinal fluid GABAergic neurosteroid levels and symptom severity in men with PTSD. Psychoneuroendocrinology 102:95–104
Rosso IM, Weiner MR, Crowley DJ, Silveri MM, Rauch SL, Jensen JE (2014) Insula and anterior cingulate GABA levels in posttraumatic stress disorder: preliminary findings using magnetic resonance spectroscopy. Depress Anxiety 31:115–123. https://doi.org/10.1002/da.22155
Schmidt D, Löscher W (1982) Plasma and cerebrospinal fluid gamma-aminobutyric acid in neurological disorders. J Neurol Neurosurg Psychiatry 45(10):931–935
Schüle C, Nothdurfter C, Rupprecht R (2014) The role of allopregnanolone in depression and anxiety. Prog Neurobiol 113:79–87
Schür RR et al (2016) Development of psychopathology in deployed armed forces in relation to plasma GABA levels. Psychoneuroendocrinology 73:263–270. https://doi.org/10.1016/j.psyneuen.2016.08.014
Simms LJ, Watson D, Doebbeling BN (2002) Confirmatory factor analyses of posttraumatic stress symptoms in deployed and nondeployed veterans of the Gulf War. J Abnorm Psychol 111:637–647. https://doi.org/10.1037/0021-843X.111.4.637
Smith SS, Gong QH, Hsu F-C, Markowitz RS, Li X (1998) GABAA receptor α4 subunit suppression prevents withdrawal properties of an endogenous steroid. Nat 392:926–929
Trousselard M, Lefebvre B, Caillet L, Andruetan Y, de Montleau F, Denis J, Canini F (2016) Is plasma GABA level a biomarker of post-traumatic stress disorder (PTSD) severity? A preliminary study. Psychiatry Res 241:273–279. https://doi.org/10.1016/j.psychres.2016.05.013
Uhlhaas S, Lange H, Wappenschmidt J, Olek K (1986) Free and conjugated CSF and plasma GABA in Huntington’s chorea. Acta Neurol Scand 74(4):261–265
Vaiva G et al (2004) Low posttrauma GABA plasma levels as a predictive factor in the development of acute posttraumatic stress disorder. Biol Psychiatry 55:250–254
Vaiva G et al (2006) Relationship between posttrauma GABA plasma levels and PTSD at 1-year follow-up. Am J Psychiatry 163:1446–1448
Funding
Support for this work was provided by a VA Career Development Award (PI: Pineles) from the Clinical Sciences R&D Service, Department of Veterans Affairs.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Rasmusson reports receiving in-kind travel compensation during the past 3 years as a scientific consultant to Cohen Veterans Bioscience, a non-profit organization. Other authors report no conflicts of interest related to this study.
Disclaimer
The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs or the United States Government.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Arditte Hall, K.A., DeLane, S.E., Anderson, G.M. et al. Plasma gamma-aminobutyric acid (GABA) levels and posttraumatic stress disorder symptoms in trauma-exposed women: a preliminary report. Psychopharmacology 238, 1541–1552 (2021). https://doi.org/10.1007/s00213-021-05785-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-021-05785-z