Abstract
Rationale
Attention deficit with hyperactivity disorder is a neurodevelopmental disorder associated with alterations in the prefrontal cortex via dopaminergic and noradrenergic neurotransmission. Neurosteroids (e.g. allopregnanolone and dehydroepiandrosterone) modulate the release of multiple neurotransmitters.
Objective
This study aims to determine the baseline concentrations and daily variations in allopregnanolone and dehydroepiandrosterone in children with attention deficit hyperactivity disorder (ADHD) and to determine the effect of chronic administration of methylphenidate on clinical symptoms and on the concentrations of these two neurosteroids.
Methods
We included 148 children aged 5 to 14 years, subdivided into two groups: ADHD group (n = 107, with a diagnosis of ADHD (DSM-IV-TR criteria), further classified in subtypes by an “attention deficit and hyperactivity scale” and subgroups by the “Children’s Depression Inventory”) and a control group (n = 41). The clinical workup included blood samples that were drawn at 20:00 and 09:00 hours, at inclusion in both groups, and after 4.61 ± 2.29 months of treatment only in the ADHD group, for measurements for allopregnanolone and dehydroepiandrosterone. Factorial analysis, adjusted for age and gender, was performed by using Stata 12.0.
Results
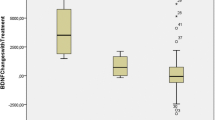
Methylphenidate induced the doubling of allopregnanolone levels in the predominantly inattentive ADHD patients without depressive symptoms (27.26 ± 12.90 vs. 12.67 ± 6.22 ng/ml, morning values). Although without statistical differences, baseline dehydroepiandrosterone levels were higher and slightly increased after methylphenidate in the ADHD subtype with depressive symptoms (7.74 ± 11.46 vs. 6.18 ± 5.99 ng/ml, in the morning), opposite to the lower baseline levels, and further decrease after methylphenidate in the inattentive subtype with depressive symptoms.
Conclusions
Different neurosteroids may have different baseline concentrations and differential responses to methylphenidate treatment as a function of ADHD subtype and subgroup. These differential responses may be a clinical marker of ADHD subtype and/or co-morbidities.


Similar content being viewed by others
References
American Psychiatric Association (2002) Manual diagnóstico y estadístico de los trastornos mentales (DSM-IV-TR). Masson, Barcelona
Amin Z, Mason GF, Cavus I, Krystal JH, Rothman DL, Epperson CN (2006) The interaction of neuroactive steroids and GABA in the development of neuropsychiatric disorders in women. Pharmacol Biochem Behav 84:635–643
Andreen L, Nyberg S, Turkmen S, van Wingen G, Fernandez G, Backstrom T (2009) Sex steroid induced negative mood may be explained by the paradoxical effect mediated by GABAA modulators. Psychoneuroendocrinology 34:1121–1132
Barkley RA (1997) Behavioral inhibition, sustained attention, and executive functions: constructing a unifying theory of ADHD. Psychol Bull 121:65–94
Bessa JM, Ferreira D, Melo I, Marques F, Cerqueira JJ, Palha JA, Almeida OF, Sousa N (2009) The mood-improving actions of antidepressants do not depend on neurogenesis but are associated with neuronal remodeling. Mol Psychiatry 14(764–73):739
Biederman J, Faraone SV, Petty C, Martelon M, Woodworth KY, Wozniak J (2013) Further evidence that pediatric-onset bipolar disorder comorbid with ADHD represents a distinct subtype: results from a large controlled family study. J Psychiat Res 47:15–22
Brickenkamp R (1997) D2, Test de Atención. Adaptación Española. TEA ediciones, Madrid
Brookes KJ, Hawi Z, Kirley A, Barry E, Gill M, Kent L (2008) Association of the steroid sulfatase (STS) gene with attention deficit hyperactivity disorder. Am J Med Genet B Neuropsychiatr Genet 147B:1531–1535
Charalampopoulos I, Dermitzaki E, Vardouli L, Tsatsanis C, Stournaras C, Margioris AN, Gravanis A (2005) Dehydroepiandrosterone sulfate and allopregnanolone directly stimulate catecholamine production via induction of tyrosine hydroxylase and secretion by affecting actin polymerization. Endocrinology 146:3309–3318
Charalampopoulos I, Remboutsika E, Margioris AN, Gravanis A (2008) Neurosteroids as modulators of neurogenesis and neuronal survival. Trends Endocrinol Metab 19:300–307
Compagnone NA, Mellon SH (2000) Neurosteroids: biosynthesis and function of these novel neuromodulators. Front Neuroendocrinol 21:1–56
Connor DF, Ford JD (2012) Comorbid symptom severity in attention-deficit/hyperactivity disorder: a clinical study. J Clin Psychiatry 73:711–717
Davies W, Humby T, Kong W, Otter T, Burgoyne PS, Wilkinson LS (2009) Converging pharmacological and genetic evidence indicates a role for steroid sulfatase in attention. Biol Psychiatry 66:360–367
Evans J, Sun Y, McGregor A, Connor B (2012) Allopregnanolone regulates neurogenesis and depressive/anxiety-like behaviour in a social isolation rodent model of chronic stress. Neuropharmacology 63:1315–1326
Fadalti M, Petraglia F, Luisi S, Bernardi F, Casarosa E, Ferrari E, Luisi M, Saggese G, Genazzani AR, Bernasconi S (1999) Changes of serum allopregnanolone levels in the first 2 years of life and during pubertal development. Pediatr Res 46:323–327
Farré-Riba A, Narbona J (1997) Escalas de Conners en la evaluación del trastorno por déficit de atención con hiperactividad: nuevo estudio factorial en niños españoles. Rev Neurol 25:200–204
Galderisi S, Mucci A, Monteleone P, Sorrentino D, Piegari G, Maj M (2003) Neurocognitive functioning in subjects with eating disorders: the influence of neuroactive steroids. Biol Psychiatry 53:921–927
George O, Vallee M, Vitiello S, Le MM, Piazza PV, Mayo W (2010) Low brain allopregnanolone levels mediate flattened circadian activity associated with memory impairments in aged rats. Biol Psychiatry 68:956–963
Girdler SS, Klatzkin R (2007) Neurosteroids in the context of stress: implications for depressive disorders. Pharmacol Ther 116:125–139
Grosso S, Luisi S, Mostardini R, Matera M, Barlocco EG, Casarosa E, Balestri P, Petraglia F (2011) Circulating levels of allopregnanolone, a neuroactive steroid, and leptin during treatment with valproic acid in children with epilepsy. Neuroendocrinology 93:159–164
Gupta R, Kar BR (2009) Development of attentional processes in ADHD and normal children. Prog Brain Res 176:259–276
Hart H, Radua J, Nakao T, Mataix-Cols D, Rubia K (2013) Meta-analysis of functional magnetic resonance imaging studies of inhibition and attention in attention-deficit/hyperactivity disorder: exploring task-specific, stimulant medication, and age effects. JAMA Psychiatry 70:185–198
Jagasia R, Steib K, Englberger E, Herold S, Faus-Kessler T, Saxe M, Gage FH, Song H, Lie DC (2009) GABA-cAMP response element-binding protein signaling regulates maturation and survival of newly generated neurons in the adult hippocampus. J Neurosci 29:7966–7977
Johansson AG, Nikamo P, Schalling M, Landen M (2011) AKR1C4 gene variant associated with low euthymic serum progesterone and a history of mood irritability in males with bipolar disorder. J Affect Disord 133:346–351
Kaufman AS, Kaufman ND (1996) KBIT. Test breve de inteligencia de Kaufmann. TEA ediciones, Madrid
Kovacs M (1992) Manual for the children’s depression inventory. Multi-Health Systems, North Tonawanda, NJ
Kowatch RA, Youngstrom EA, Danielyan A, Findling RL (2005) Review and meta-analysis of the phenomenology and clinical characteristics of mania in children and adolescents. Bipolar Disord 7:483–496
Kretschmer BD (1999) Modulation of the mesolimbic dopamine system by glutamate: role of NMDA receptors. J Neurochem 73:839–848
Maayan R, Yoran-Hegesh R, Strous R, Nechmad A, Averbuch E, Weizman A, Spivak B (2003) Three-month treatment course of methylphenidate increases plasma levels of dehydroepiandrosterone (DHEA) and dehydroepiandrosterone-sulfate (DHEA-S) in attention deficit hyperactivity disorder. Neuropsychobiology 48:111–115
Matthews M, Nigg JT, Fair DA (2013) Attention deficit hyperactivity disorder. Curr Top Behav Neurosci 1–32. doi:10.1007/7854_2013_249
Miller MN, Miller BE (2001) Premenstrual exacerbations of mood disorders. Psychopharmacol Bull 35:135–149
Moghaddam B, Roth RH, Bunney BS (1990) Characterization of dopamine release in the rat medial prefrontal cortex as assessed by in vivo microdialysis: comparison to the striatum. Neuroscience 36:669–676
Molina-Carballo A, Muñoz-Hoyos A, Sánchez-Forte M, Uberos-Fernández J, Moreno-Madrid F, Acuña-Castroviejo D (2007) Melatonin increases following convulsive seizures may be related to its anticonvulsant properties at physiological concentrations. Neuropediatrics 38:122–125
Molina-Carballo A, Naranjo-Gómez A, Uberos J, Justicia-Martínez F, Ruiz-Ramos MJ, Cubero-Millán MI, Contreras-Chova F, Augustin-Morales MC, Khaldy-Belkadi H, Muñoz-Hoyos A (2013) Methylphenidate effects on blood serotonin and melatonin levels may help to synchronise biological rhythms in children with ADHD. J Psychiat Res 47:377–383
Muñoz-Hoyos A, Molina-Carballo A, Augustin-Morales MC, Contreras-Chova F, Naranjo-Gómez A, Justicia-Martínez F, Uberos-Fernández J (2011) Psychological dwarfism: psychopathological and putative neuroendocrine markers. Psychiat Res 188:96–101
Naert G, Maurice T, Tapia-Arancibia L, Givalois L (2007) Neuroactive steroids modulate HPA axis activity and cerebral brain-derived neurotrophic factor (BDNF) protein levels in adult male rats. Psychoneuroendocrinology 32:1062–1078
Nakao T, Radua J, Rubia K, Mataix-Cols D (2011) Gray matter volume abnormalities in ADHD: voxel-based meta-analysis exploring the effects of age and stimulant medication. Am J Psychiatry 168:1154–1163
Nigg JT (2005) Neuropsychologic theory and findings in attention-deficit/hyperactivity disorder: the state of the field and salient challenges for the coming decade. Biol Psychiatry 57:1424–1435
Nigg JT, Casey BJ (2005) An integrative theory of attention-deficit/hyperactivity disorder based on the cognitive and affective neurosciences. Dev Psychopathol 17:785–806
Pinna G, Costa E, Guidotti A (2005) Changes in brain testosterone and allopregnanolone biosynthesis elicit aggressive behavior. Proc Natl Acad Sci U S A 102:2135–2140
Pluchino N, Cubeddu A, Giannini A, Merlini S, Cela V, Angioni S, Genazzani AR (2009) Progestogens and brain: an update. Maturitas 62:349–355
Predieri B, Luisi S, Casarosa E, De SM, Balli F, Bernasconi S, Rossi M, Petraglia F, Iughetti L (2007) High basal serum allopregnanolone levels in overweight girls. Int J Obes (Lond) 31:543–549
Puia G, Gullo F, Dossi E, Lecchi M, Wanke E (2012) Novel modulatory effects of neurosteroids and benzodiazepines on excitatory and inhibitory neurons excitability: a multi-electrode array recording study. Front Neural Circuits 6:94
Sánchez CR, Ramos C, Díaz F, Simón M (2010) Validación de la escala de evaluación del trastorno por déficit de atención/hiperactividad (EDAH) en población adolescente. Rev Neurol 50:283–290
Strous RD, Spivak B, Yoran-Hegesh R, Maayan R, Averbuch E, Kotler M, Mester R, Weizman A (2001) Analysis of neurosteroid levels in attention deficit hyperactivity disorder. Int J Neuropsychopharmacol 4:259–264
Traish AM, Kang HP, Saad F, Guay AT (2011) Dehydroepiandrosterone (DHEA)—a precursor steroid or an active hormone in human physiology. J Sex Med 8:2960–2982
Trent S, Dean R, Veit B, Cassano T, Bedse G, Ojarikre OA, Humby T, Davies W (2013) Biological mechanisms associated with increased perseveration and hyperactivity in a genetic mouse model of neurodevelopmental disorder. Psychoneuroendocrinology 38:1370–1380
van Ewijk H, Heslenfeld DJ, Zwiers MP, Buitelaar JK, Oosterlaan J (2012) Diffusion tensor imaging in attention deficit/hyperactivity disorder: a systematic review and meta-analysis. Neurosci Biobehav Rev 36:1093–1106
van Goozen SH, van den Ban E, Matthys W, Cohen-Kettenis PT, Thijssen JH, van Engeland H (2000) Increased adrenal androgen functioning in children with oppositional defiant disorder: a comparison with psychiatric and normal controls. J Am Acad Child Adolesc Psychiatry 39:1446–1451
Wang LJ, Hsiao CC, Huang YS, Chiang YL, Ree SC, Chen YC, Wu YW, Wu CC, Shang ZY, Chen CK (2011) Association of salivary dehydroepiandrosterone levels and symptoms in patients with attention deficit hyperactivity disorder during six months of treatment with methylphenidate. Psychoneuroendocrinology 36:1209–1216
Wiltschko AB, Pettibone JR, Berke JD (2010) Opposite effects of stimulant and antipsychotic drugs on striatal fast-spiking interneurons. Neuropsychopharmacology 35:1261–1270
Wolkowitz OM, Reus VI, Mellon SH (2011) Of sound mind and body: depression, disease, and accelerated aging. Dialogues Clin Neurosci 13:25–39
Yang SY, He XY, Olpin SE, Sutton VR, McMenamin J, Philipp M, Denman RB, Malik M (2009) Mental retardation linked to mutations in the HSD17B10 gene interfering with neurosteroid and isoleucine metabolism. Proc Natl Acad Sci U S A 106:14820–14824
Zambrano-Sánchez E, Martínez-Cortés JA, Del Río-Carlos Y, Martinez-Wbaldo MD, Poblano A (2011) Identification of attention-deficit-hyperactivity disorder and conduct disorder in Mexican children by the scale of evaluation of deficit of attention and hyperactivity scale. Psychiatry Res 187:437–440
Zheng P (2009) Neuroactive steroid regulation of neurotransmitter release in the CNS: action, mechanism and possible significance. Prog Neurobiol 89:134–152
Acknowledgments
Funding for this study was provided by the Health Research Fund (FIS; Spanish Ministry of Science and Innovation), FIS-PI07-0603; the FIS had no further role in study design; in the collection, analysis and interpretation of data; in the writing of the report; and in the decision to submit the paper for publication. We wish to thank to Ms. Puri Ubago-Corpas for her entire supervision and support.
Conflict of interest
All of the researchers declare that they have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Molina-Carballo, A., Justicia-Martínez, F., Moreno-Madrid, F. et al. Differential responses of two related neurosteroids to methylphenidate based on ADHD subtype and the presence of depressive symptomatology. Psychopharmacology 231, 3635–3645 (2014). https://doi.org/10.1007/s00213-014-3514-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-014-3514-5