Abstract
Summary
Preoperative bone density assessment is necessary to predict screw loosening. The forearm BMD is a useful predictor of BMD-related complications after lumbar operation. Our results show that the forearm BMD is as effective a predictor of screw loosening as the lumbar average HU value. Measurement of the forearm BMD may be a useful adjunct in predicting screw loosening following lumbar fusion.
Purpose
To determine the relationship between forearm bone mineral density (BMD) and the risk of pedicle screw loosening in patients with lumbar spondylolisthesis.
Methods
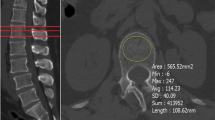
We retrospectively evaluated 270 patients who underwent posterior lumbar interbody fusion for lumbar spondylolisthesis. The patients were divided into two groups on the basis of the with or without loose screws: the loosening group and the non-loosening group. The patient’s gender, age, BMI, smoking and diabetes histories, and the operative segment were recorded as the basic information. The Hounsfield unit (HU) value for the BMD of the L1-4 lumbar was measured using computed tomography. The patient’s distal one-third of the length of the radius and ulna of the non-dominant forearm was chosen as the site for dual-energy X-ray (DXA) bone density testing.
Results
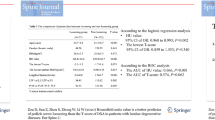
The rate of screw loosening was 13% at a minimum 12 months follow-up. Average forearm BMD (0.461 ± 0.1 vs 0.577 ± 0.1, p < 0.001) and mean HU value (L1-4) (121.1 ± 27.3 vs 155.6 ± 32.2, p < 0.001) were lower in the screw loosening group than those in the non-loosening group. In multivariate logistic regression analysis, the forearm BMD (OR 0.840; 95%CI 0.797–0.886) and HU value (L1-4) (OR 0.952; 95%CI 0.935–0.969) were independent risk factor for screw loosening. The area under the curve (AUC) for the forearm BMD and HU value for prediction of pedicle screw loosening was 0.802 and 0.811. The forearm BMD cut-off for predicting pedicle screw loosening was 0.543 (sensitivity, 0.800; specificity, 0.864).
Conclusions
The forearm BMD was an independent risk factor for loosening of the lumbar pedicle screws. The forearm BMD was a valid predictor of pedicle screw loosening in patients undergoing lumbar fusion, as was the CT HU value.



Similar content being viewed by others
Data availability
Data are available upon reasonable request.
References
Galbusera F, Volkheimer D, Reitmaier S, Berger-Roscher N, Kienle A, Wilke HJ (2015) Pedicle screw loosening: a clinically relevant complication? Eur Spine J 24:1005–1016
Zou D, Sun Z, Zhou S, Zhong W, Li W (2020) Hounsfield units value is a better predictor of pedicle screw loosening than the T-score of DXA in patients with lumbar degenerative diseases. Eur Spine J 29:1105–1111
Yuan L, Zhang X, Zeng Y, Chen Z, Li W (2021) Incidence, risk, and outcome of pedicle screw loosening in degenerative lumbar scoliosis patients undergoing long-segment fusion. Global Spine J 13(4):1064–1071
Bredow J, Boese CK, Werner CM, Siewe J, Lohrer L, Zarghooni K, Eysel P, Scheyerer MJ (2016) Predictive validity of preoperative CT scans and the risk of pedicle screw loosening in spinal surgery. Arch Orthop Trauma Surg 136:1063–1067
Xu F, Zou D, Li W, Sun Z, Jiang S, Zhou S, Li Z (2020) Hounsfield units of the vertebral body and pedicle as predictors of pedicle screw loosening after degenerative lumbar spine surgery. Neurosurg Focus 49:E10
Mehmanparast H, Petit Y, Mac-Thiong JM (2015) Comparison of pedicle screw loosening mechanisms and the effect on fixation strength. J Biomech Eng 137:121003
Zou D, Muheremu A, Sun Z, Zhong W, Jiang S, Li W (2020) Computed tomography Hounsfield unit-based prediction of pedicle screw loosening after surgery for degenerative lumbar spine disease. J Neurosurg Spine 3:1–6
Bokov A, Bulkin A, Aleynik A, Kutlaeva M, Mlyavykh S (2019) Pedicle screws loosening in patients with degenerative diseases of the lumbar spine: potential risk factors and relative contribution. Global Spine J 9:55–61
Weiser L, Huber G, Sellenschloh K, Viezens L, Puschel K, Morlock MM, Lehmann W (2017) Insufficient stability of pedicle screws in osteoporotic vertebrae: biomechanical correlation of bone mineral density and pedicle screw fixation strength. Eur Spine J 26:2891–2897
Chin DK, Park JY, Yoon YS, Kuh SU, Jin BH, Kim KS, Cho YE (2007) Prevalence of osteoporosis in patients requiring spine surgery: incidence and significance of osteoporosis in spine disease. Osteoporos Int 18:1219–1224
Zou D, Jiang S, Zhou S, Sun Z, Zhong W, Du G, Li W (2020) Prevalence of osteoporosis in patients undergoing lumbar fusion for lumbar degenerative diseases: a combination of DXA and Hounsfield units. Spine (Phila Pa 1976) 45:E406–E410
Pennington Z, Ehresman J, Lubelski D, Cottrill E, Schilling A, Ahmed AK, Feghali J, Witham TF, Sciubba DM (2021) Assessing underlying bone quality in spine surgery patients: a narrative review of dual-energy X-ray absorptiometry (DXA) and alternatives. Spine J 21:321–331
Link TM, Kazakia G (2020) Update on imaging-based measurement of bone mineral density and quality. Curr Rheumatol Rep 22:13
Muraki S, Yamamoto S, Ishibashi H, Horiuchi T, Hosoi T, Orimo H, Nakamura K (2004) Impact of degenerative spinal diseases on bone mineral density of the lumbar spine in elderly women. Osteoporos Int 15:724–728
Pye SR, Reid DM, Adams JE, Silman AJ, O’Neill TW (2006) Radiographic features of lumbar disc degeneration and bone mineral density in men and women. Ann Rheum Dis 65:234–238
Choi MK, Kim SM, Lim JK (2016) Diagnostic efficacy of Hounsfield units in spine CT for the assessment of real bone mineral density of degenerative spine: correlation study between T-scores determined by DEXA scan and Hounsfield units from CT. Acta Neurochir (Wien) 158:1421–1427
Pu HY, Chen Q, Huang K, Wei P (2023) Correlation between forearm bone mineral density measured by dual energy x-ray absorptiometry and hounsfield units value measured by CT in lumbar spine. Z Orthop Unfall. https://doi.org/10.1055/a-1984-0466
Ahern DP, McDonnell JM, Riffault M, Evans S, Wagner SC, Vaccaro AR, Hoey DA, Butler JS (2021) A meta-analysis of the diagnostic accuracy of Hounsfield units on computed topography relative to dual-energy X-ray absorptiometry for the diagnosis of osteoporosis in the spine surgery population. Spine J 21:1738–1749
Schreiber JJ, Anderson PA, Rosas HG, Buchholz AL, Au AG (2011) Hounsfield units for assessing bone mineral density and strength: a tool for osteoporosis management. J Bone Joint Surg Am 93:1057–1063
Ran L, Xie T, Zhao L, Huang S, Zeng J (2022) Low Hounsfield units on computed tomography are associated with cage subsidence following oblique lumbar interbody fusion (OLIF). Spine J 22:957–964
Damilakis J, Papadokostakis G, Perisinakis K, Hadjipavlou A, Gourtsoyiannis N (2003) Can radial bone mineral density and quantitative ultrasound measurements reduce the number of women who need axial density skeletal assessment? Osteoporos Int 14:688–693
Jones T, Davie MW (1998) Bone mineral density at distal forearm can identify patients with osteoporosis at spine or femoral neck. Br J Rheumatol 37:539–543
Trivitayaratana W, Trivitayaratana P (2001) The accuracy of bone mineral density at distal radius on non-forearm osteoporosis identification. J Med Assoc Thai 84:566–571
Cheuk KY, Hu Y, Tam EMS et al (2019) Bone measurements at multiple skeletal sites in adolescent idiopathic scoliosis-an in vivo correlation study using DXA, HR-pQCT and QCT. Arch Osteoporos 14:70
Abdelmohsen AM (2017) Comparison of central and peripheral bone mineral density measurements in postmenopausal women. J Chiropr Med 16:199–203
Eftekhar-Sadat B, Ghavami M, Toopchizadeh V, Ghahvechi Akbari M (2016) Wrist bone mineral density utility in diagnosing hip osteoporosis in postmenopausal women. Ther Adv Endocrinol Metab 7:207–211
Pu HY, Chen Q, Huang K, Zeng R, Wei P (2022) Forearm T-score as a predictor of cage subsidence in patients with degenerative lumbar spine disease following posterior single-segment lumbar interbody fusion. BMC Musculoskelet Disord 23:1058
Cheng XG, Yang DZ, Zhou Q et al (2007) Age-related bone mineral density, bone loss rate, prevalence of osteoporosis, and reference database of women at multiple centers in China. J Clin Densitom 10:276–284
Li W, Zhu H, Hua Z, Miao D, Wang F, Tong T, Wang L (2023) Vertebral bone quality score as a predictor of pedicle screw loosening following surgery for degenerative lumbar disease. Spine. https://doi.org/10.1097/BRS.0000000000004577
Shepherd JA, Schousboe JT, Broy SB, Engelke K, Leslie WD (2015) Executive summary of the 2015 ISCD Position Development Conference on Advanced Measures From DXA and QCT: fracture prediction beyond BMD. J Clin Densitom 18:274–286
Ohtori S, Inoue G, Orita S et al (2013) Comparison of teriparatide and bisphosphonate treatment to reduce pedicle screw loosening after lumbar spinal fusion surgery in postmenopausal women with osteoporosis from a bone quality perspective. Spine (Phila Pa 1976) 38:E487-492
Tokuhashi Y, Matsuzaki H, Oda H, Uei H (2008) Clinical course and significance of the clear zone around the pedicle screws in the lumbar degenerative disease. Spine (Phila Pa 1976) 33:903–908
Kim JB, Park SW, Lee YS, Nam TK, Park YS, Kim YB (2015) The effects of spinopelvic parameters and paraspinal muscle degeneration on S1 screw loosening. J Korean Neurosurg Soc 58:357–362
Chen P, Li Z, Hu Y (2016) Prevalence of osteoporosis in China: a meta-analysis and systematic review. BMC Public Health 16:1039
Funding
This study was supported in part by the Research Development Program of North Sichuan Medical College (CBY20-QA-Y24), Research Development Plan of the Affiliated Hospital of North Sichuan Medical College (2022JC020), Projects of the Science & Technology Department of Sichuan Province (2023NSFSC0659), Sichuan Provincial Medical Association Special Research Fund (2021SAT05), and Sichuan Provincial Medical Association Special Research Fund (2019HR18).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Approval is obtained from Biomedical Ethics Review Committee of Affiliated Hospital of North Sichuan Medical College (Approval number: IRB2023ER89-1). The requirement for informed consent was waived to the retrospective analysis.
Conflicts of interest
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chen, Q., Tu, Z., Ai, Y. et al. Forearm bone mineral density predicts screw loosening after lumbar fusion similar to lumbar Hounsfield unit value in patients with lumbar spondylolisthesis. Osteoporos Int 35, 543–549 (2024). https://doi.org/10.1007/s00198-023-06957-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-023-06957-7