Abstract
Summary
Osteoporosis was suggested to be associated with higher odds of age-related macular degeneration. However, the temporal relationship between osteoporosis and age-related macular degeneration has not been explored. This population-based longitudinal follow-up study showed an increased risk of age-related macular degeneration in both men and women with osteoporosis.
Purpose
To investigate the long-term risk of age-related macular degeneration (AMD) in patients with osteoporosis.
Methods
This is a retrospective cohort study using the Longitudinal Health Insurance Database 2005, a subset of Taiwan’s National Health Insurance research database. A total of 23,611 individuals aged 50 to 79 who were diagnosed with osteoporosis between January 1, 2002 and December 31, 2006, were enrolled in the osteoporosis group. An exactly equal number of propensity score-matched individuals without osteoporosis comprised the comparison group. The variables used in propensity score matching included age, sex, comorbidities, and socioeconomic status. Cox proportional hazard regression analysis was used to evaluate the association between osteoporosis and AMD. The main outcome measure is the occurrence of newly diagnosed AMD.
Results
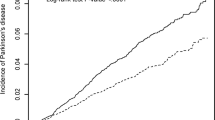
The hazard ratio (HR) of AMD in the osteoporosis group was 1.34 times higher than in the comparison group (95% confidence interval [CI] 1.22–1.47, p < 0.05). The AMD-free survival rate of the osteoporosis group was significantly lower than that of the comparison group (p < 0.0001). Sex-stratified analysis revealed a significantly increased risk of AMD in both osteoporotic men (HR 1.45; 95% CI 1.20–1.76, p = 0.0002) and women (HR 1.31; 95% CI 1.17–1.46, p < 0.0001) compared with their non-osteoporotic counterparts.
Conclusion
This longitudinal follow-up study revealed an increased risk of developing AMD in both men and women with osteoporosis.


Similar content being viewed by others
References
Hernlund E, Svedbom A, Ivergård M, Compston J, Cooper C, Stenmark J, McCloskey EV, Jönsson B, Kanis JA (2013) Osteoporosis in the European Union: medical management, epidemiology and economic burden. A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos 8:136. https://doi.org/10.1007/s11657-013-0136-1
Jager RD, Mieler WF, Miller JW (2008) Age-related macular degeneration. N Engl J Med 358:2606–2617. https://doi.org/10.1056/NEJMra0801537
Apte RS (2021) Age-related macular degeneration. N Engl J Med 385:539–547. https://doi.org/10.1056/NEJMcp2102061
Yoo TK, Kim SH, Kwak J, Kim HK, Rim TH (2018) Association between osteoporosis and age-related macular degeneration: the Korea National Health and Nutrition Examination Survey. Invest Ophthalmol Vis Sci 59:Amd132–amd142. https://doi.org/10.1167/iovs.18-24059
Huang HK, Lin SM, Loh CH, Wang JH, Liang CC (2019) Association between cataract and risks of osteoporosis and fracture: a nationwide cohort study. J Am Geriatr Soc 67:254–260. https://doi.org/10.1111/jgs.15626
Velilla S, García-Medina JJ, García-Layana A, Dolz-Marco R, Pons-Vázquez S, Pinazo-Durán MD, Gómez-Ulla F, Arévalo JF, Díaz-Llopis M, Gallego-Pinazo R (2013) Smoking and age-related macular degeneration: review and update. J Ophthalmol 2013:895147–895147. https://doi.org/10.1155/2013/895147
Al-Bashaireh AM, Haddad LG, Weaver M, Chengguo X, Kelly DL, Yoon S (2018) The effect of tobacco smoking on bone mass: an overview of pathophysiologic mechanisms. J Osteoporos 2018:1206235. https://doi.org/10.1155/2018/1206235
Stang P, Lydick E, Silberman C, Kempel A, Keating ET (2000) The prevalence of COPD: using smoking rates to estimate disease frequency in the general population. Chest 117:354s–359s. https://doi.org/10.1378/chest.117.5_suppl_2.354s
Cackett P, Tay WT, Aung T, Wang JJ, Shankar A, Saw SM, Mitchell P, Wong TY (2008) Education, socio-economic status and age-related macular degeneration in Asians: the Singapore Malay Eye Study. Br J Ophthalmol 92:1312–1315. https://doi.org/10.1136/bjo.2007.136077
Liu CYHY, Chuang YL, Chen YJ, Weng WS, Liu JS, Liang K (2006) Incorporating development stratification of Taiwan townships into sampling design of large scale health interview survey. J Health Manag 4:1–22. https://doi.org/10.29805/jhm.200606.0001
Parsons LS (2004) Performing a 1: N case-control match on propensity score. Proceedings of the 29th annual SAS users group international conference. SAS Institute, p e11
Austin PC (2009) Using the standardized difference to compare the prevalence of a binary variable between two groups in observational research. Commun Stat Simul Comput 38:1228–1234. https://doi.org/10.1080/03610910902859574
Mammo Z, Guo M, Maberley D, Matsubara J, Etminan M (2016) Oral bisphosphonates and risk of wet age-related macular degeneration. Am J Ophthalmol 168:62–67. https://doi.org/10.1016/j.ajo.2016.04.022
Garriga C, Pazianas M, Hawley S, Delmestri A, Prieto-Alhambra D, Cooper C, Judge A (2018) Oral bisphosphonate use and age-related macular degeneration: retrospective cohort and nested case-control study. Ann N Y Acad Sci 1415:34–46. https://doi.org/10.1111/nyas.13589
Gage BF, Birman-Deych E, Radford MJ, Nilasena DS, Binder EF (2006) Risk of osteoporotic fracture in elderly patients taking warfarin: results from the National Registry of Atrial Fibrillation 2. Arch Intern Med 166:241–246. https://doi.org/10.1001/archinte.166.2.241
Ginaldi L, Di Benedetto MC, De Martinis M (2005) Osteoporosis, inflammation and ageing. Immun Ageing 2:14. https://doi.org/10.1186/1742-4933-2-14
Yun AJ, Lee PY (2004) Maldaptation of the link between inflammation and bone turnover may be a key determinant of osteoporosis. Med Hypotheses 63:532–537. https://doi.org/10.1016/S0306-9877(03)00326-8
Lencel P, Magne D (2011) Inflammaging: the driving force in osteoporosis? Med Hypotheses 76:317–321. https://doi.org/10.1016/j.mehy.2010.09.023
Srivastava RK, Dar HY, Mishra PK (2018) Immunoporosis: immunology of osteoporosis—role of T cells. Front Immunol 9. https://doi.org/10.3389/fimmu.2018.00657
Klein R, Myers CE, Cruickshanks KJ, Gangnon RE, Danforth LG, Sivakumaran TA, Iyengar SK, Tsai MY, Klein BE (2014) Markers of inflammation, oxidative stress, and endothelial dysfunction and the 20-year cumulative incidence of early age-related macular degeneration: the Beaver Dam Eye Study. JAMA Ophthalmol 132:446–455. https://doi.org/10.1001/jamaophthalmol.2013.7671
Seddon JM, George S, Rosner B, Rifai N (2005) Progression of age-related macular degeneration: prospective assessment of C-reactive protein, interleukin 6, and other cardiovascular biomarkers. Arch Ophthalmol 123:774–782. https://doi.org/10.1001/archopht.123.6.774
Bolton C, Stone M, Edwards P, Duckers J, Evans W, Shale D (2009) Circulating matrix metalloproteinase-9 and osteoporosis in patients with chronic obstructive pulmonary disease. Chron Respir Dise 6:81–87. https://doi.org/10.1177/1479972309103131
Malemud CJ (2006) Matrix metalloproteinases (MMPs) in health and disease: an overview. Front Biosci 11:1696–1701. https://doi.org/10.2741/1915
García-Onrubia L, Valentín-Bravo FJ, Coco-Martin RM, González-Sarmiento R, Pastor JC, Usategui-Martín R, Pastor-Idoate S (2020) Matrix metalloproteinases in age-related macular degeneration (AMD). Int J Mol Sci 21:5934. https://doi.org/10.3390/ijms21165934
Lambert V, Munaut C, Jost M, Noël A, Werb Z, Foidart J-M, Rakic J-M (2002) Matrix metalloproteinase-9 contributes to choroidal neovascularization. Am J Pathol 161:1247–1253. https://doi.org/10.1016/S0002-9440(10)64401-X
Chau KY, Sivaprasad S, Patel N, Donaldson TA, Luthert PJ, Chong NV (2008) Plasma levels of matrix metalloproteinase-2 and -9 (MMP-2 and MMP-9) in age-related macular degeneration. Eye (Lond) 22:855–859
Mendoza E-PN, Marín J-WT, Carrillo DC, Guzmán GE, Arango LG (2016) Prevalence of vitamin D deficiency in patients with osteoporosis. Rev Colomb de Reumatol (English Edition) 23:17–23. https://doi.org/10.1016/j.rcreue.2016.04.003
Lips P, Hosking D, Lippuner K, Norquist JM, Wehren L, Maalouf G, Ragi-Eis S, Chandler J (2006) The prevalence of vitamin D inadequacy amongst women with osteoporosis: an international epidemiological investigation. J Intern Med 260:245–254. https://doi.org/10.1111/j.1365-2796.2006.01685.x
Annweiler C, Drouet M, Duval GT, Paré PY, Leruez S, Dinomais M, Milea D (2016) Circulating vitamin D concentration and age-related macular degeneration: systematic review and meta-analysis. Maturitas 88:101–112. https://doi.org/10.1016/j.maturitas.2016.04.002
Parekh N, Chappell RJ, Millen AE, Albert DM, Mares JA (2007) Association between vitamin D and age-related macular degeneration in the Third National Health and Nutrition Examination Survey, 1988 through 1994. Arch Ophthalmol 125:661–669. https://doi.org/10.1001/archopht.125.5.661
Merle BMJ, Silver RE, Rosner B, Seddon JM (2017) Associations between vitamin D intake and progression to incident advanced age-related macular degeneration. Invest Ophthalmol Vis Sci 58:4569–4578. https://doi.org/10.1167/iovs.17-21673
Layana AG, Minnella AM, Garhöfer G, Aslam T, Holz FG, Leys A, Silva R, Delcourt C, Souied E, Seddon JM (2017) Vitamin D and age-related macular degeneration. Nutrients 9:1120. https://doi.org/10.3390/nu9101120
Khandhadia S, Lotery A (2010) Oxidation and age-related macular degeneration: insights from molecular biology. Expert Rev Mol Med 12:e34. https://doi.org/10.1017/s146239941000164x
Radak Z, Taylor AW, Ohno H, Goto S (2001) Adaptation to exercise-induced oxidative stress: from muscle to brain. Exerc Immunol Rev 7:90–107
McGuinness MB, Le J, Mitchell P, Gopinath B, Cerin E, Saksens NTM, Schick T, Hoyng CB, Guymer RH, Finger RP (2017) Physical activity and age-related macular degeneration: a systematic literature review and meta-analysis. Am J Ophthalmol 180:29–38. https://doi.org/10.1016/j.ajo.2017.05.016
Pagnotti GM, Styner M, Uzer G, Patel VS, Wright LE, Ness KK, Guise TA, Rubin J, Rubin CT (2019) Combating osteoporosis and obesity with exercise: leveraging cell mechanosensitivity. Nat Rev Endocrinol 15:339–355. https://doi.org/10.1038/s41574-019-0170-1
Lewczuk E, Białoszewski D (2006) The level of physical activity in patients with osteoporosis in relation to the risk and prevention of falls. Ortop Traumatol Rehabil 8:412–421
Kaarniranta K, Machalińska A, Veréb Z, Salminen A, Petrovski G, Kauppinen A (2015) Estrogen signalling in the pathogenesis of age-related macular degeneration. Curr Eye Res 40:226–233. https://doi.org/10.3109/02713683.2014.925933
Ahlborg HG, Johnell O, Turner CH, Rannevik G, Karlsson MK (2003) Bone loss and bone size after menopause. N Engl J Med 349:327–334. https://doi.org/10.1056/NEJMoa022464
Kang MJ, Rim TH, Kim SS (2016) Visual acuity and falls in South Korea: Korean National Health and Nutrition Examination Survey 2008-2012. J Korean Ophthalmol Soc 57:1451–1459. https://doi.org/10.3341/jkos.2016.57.9.1451
Sun CC, Huang TS, Fu TS, Lee CY, Chen BY, Chen FP (2020) Association of age-related macular degeneration on fracture risks among osteoporosis population: a nationwide population-based cohort study. BMJ Open 10:e037028. https://doi.org/10.1136/bmjopen-2020-037028
Hong T, Mitchell P, Burlutsky G, Samarawickrama C, Wang JJ (2014) Visual impairment and the incidence of falls and fractures among older people: longitudinal findings from the Blue Mountains Eye Study. Invest Ophthalmol Vis Sci 55:7589–7593. https://doi.org/10.1167/iovs.14-14262
Resnick B, Nahm ES, Zhu S, Brown C, An M, Park B, Brown J (2014) The impact of osteoporosis, falls, fear of falling, and efficacy expectations on exercise among community-dwelling older adults. Orthop Nurs 33:277. https://doi.org/10.1097/nor.0000000000000084
Tonelli M, Wiebe N, Fortin M et al (2015) Methods for identifying 30 chronic conditions: application to administrative data. BMC Med Inform Decis Mak 15:31. https://doi.org/10.1186/s12911-015-0155-5
Lin SY, Hsu WH, Lin CL, Lin CC, Lin JM, Chang YL, Hsu CY, Kao CH (2018) Evidence for an association between macular degeneration and thyroid cancer in the aged population. Int J Environ Res Public Health 15(5):902. https://doi.org/10.3390/ijerph15050902
Zhang J, Mitsuhashi T, Matsuo T, Yorifuji T, Hamada J, Liu Y (2021) Alcohol consumption and age-related macular degeneration: a systematic review and dose–response meta-analysis. Curr Eye Res 46:1900–1907. https://doi.org/10.1080/02713683.2021.1942070
Godos J, Giampieri F, Chisari E et al (2022) Alcohol consumption, bone mineral density, and risk of osteoporotic fractures: a dose–response meta-analysis. Int J Environ Res Public Health 19:1515
Funding
This research was supported by grants NTU-JP-110L7246 and NTU-JP-111L7221 from National Taiwan University, Taipei, Taiwan.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
This study was approved by the Research Ethics Committee of National Taiwan University Hospital (NTUH-REC No.: 202012192RINA).
Informed consent
Not applicable.
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hsu, SC., Feng, SH. & Pan, SL. Risk of developing age-related macular degeneration in patients with osteoporosis: a population-based, longitudinal follow-up study. Osteoporos Int 34, 793–801 (2023). https://doi.org/10.1007/s00198-023-06711-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-023-06711-z