Abstract
Summary
Low serum alkaline phosphatase (ALP) was found in 9% of patients attending an osteoporosis clinic, 0.6% of hospital patients, and 2/22 with an atypical femoral fracture. Hypophosphatasia was diagnosed in 3% of osteoporosis clinic patients with low ALP. Low ALP is a screening tool for hypophosphatasia, a condition potentially aggravated by antiresorptive therapy.
Introduction
Hypophosphatasia (HPP) is an inherited disorder associated with impaired primary mineralisation of osteoid (osteomalacia). HPP may be misdiagnosed as osteoporosis, a reduction in the volume of normally mineralized bone. Both illnesses may result in fragility fractures, although stress and atypical fractures are more common in HPP. Antiresorptive therapy, first-line treatment for osteoporosis, is relatively contraindicated in HPP. Misdiagnosis and mistreatment can be avoided by recognising a low serum alkaline phosphatase (ALP). Our aim was to determine the prevalence of a low ALP (< 30 IU/L) in patients attending an osteoporosis clinic, in a hospital-wide setting, and in a group of patients with atypical femoral fractures (AFF).
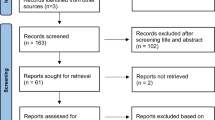
Methods
This was a retrospective study of patients attending an osteoporosis clinic at a tertiary hospital during 8 years (2012–2020). Patients were categorised into those with a transiently low ALP, those with low ALP on ≥ 2 occasions but not the majority of measurements, and those with a persistently low ALP. ALP levels were also assessed in hospital-wide records and a group of patients with AFF.
Results
Of 1839 patients attending an osteoporosis clinic, 168 (9%) had ≥ 1 low ALP, 50 (2.7%) had low ALP for ≥ 2 months, and seven (0.4%) had persistently low ALP levels. HPP was diagnosed in five patients, four of whom had persistently low ALP levels. The prevalence of HPP was 0.3% in the osteoporosis clinic and 3% in patients with ≥ 1 low ALP. Low ALP occurred in 0.6% of all hospital patients and 2/22 with AFF.
Conclusion
Persistently low ALP in osteoporosis clinic attendees is easy to identify and signals the possibility of hypophosphatasia, a condition that may be mistaken for osteoporosis and incorrectly treated with antiresorptive therapy.


Similar content being viewed by others
References
Harvey N, Dennison E, Cooper C (2010) Osteoporosis: impact on health and economics. Nat Rev Rheumatol 6(2):99–105. https://doi.org/10.1038/nrrheum.2009.260
Ebeling PR, Nguyen HH, Aleksova J, Vincent AJ, Wong P, Milat F (2022) Secondary osteoporosis. Endocr Rev 43(2):240–313
Stein E, Shane E (2003) Secondary osteoporosis. Endocrinol Metab Clin North Am 32(1):115–134. https://doi.org/10.1016/S0889-8529(02)00062-2
Mornet E (2007) Hypophosphatasia. Orphanet J Rare Dis 2:40. https://doi.org/10.1186/1750-1172-2-40
Whyte MP (2008) Chapter 73 - Hypophosphatasia: nature’s window on alkaline phosphatase function in humans. In: Bilezikian JP, Raisz LG, Martin TJ (eds) Principles of bone biology, 3rd edn. Academic Press, San Diego, pp 1573–1598
Swallow DM, Povey S, Parkar M, Andrews PW, Harris H, Pym B, Goodfellow P (1986) Mapping of the gene coding for the human liver/bone/kidney isozyme of alkaline phosphatase to chromosome 1. Ann Hum Genet 50(3):229–235. https://doi.org/10.1111/j.1469-1809.1986.tb01043.x
Hofmann C, Girschick HJ, Mentrup B, Graser S, Seefried L, Liese J, Jakob F (2013) Clinical aspects of hypophosphatasia: an update. Clin Rev Bone Miner Metab 11(2):60–70. https://doi.org/10.1007/s12018-013-9139-0
Whyte MP (2016) Hypophosphatasia - aetiology, nosology, pathogenesis, diagnosis and treatment. Nat Rev Endocrinol 12(4):233–246. https://doi.org/10.1038/nrendo.2016.14
Conti F, Ciullini L, Pugliese G (2017) Hypophosphatasia: clinical manifestation and burden of disease in adult patients. Clin Cases Miner Bone Metab 14(2):230 4. https://doi.org/10.11138/ccmbm/2017.14.1.230
Nguyen HH, van de Laarschot DM, Verkerk AJMH, Milat F, Zillikens MC, Ebeling PR (2018) Genetic risk factors for atypical femoral fractures (AFFs): a systematic review. JBMR Plus 2(1):1–11. https://doi.org/10.1002/jbm4.10024
Shane E, Burr D, Abrahamsen B, Adler RA, Brown TD, Cheung AM, Cosman F, Curtis JR, Dell R, Dempster DW, Ebeling PR, Einhorn TA, Genant HK, Geusens P, Klaushofer K, Lane JM, McKiernan F, McKinney R, Ng A, Nieves J, O’Keefe R, Papapoulos S, Howe TS, van der Meulen MC, Weinstein RS, Whyte MP (2014) Atypical subtrochanteric and diaphyseal femoral fractures: second report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res 29(1):1–23. https://doi.org/10.1002/jbmr.1998
Schmidt T, Mussawy H, Rolvien T, Hawellek T, Hubert J, Rüther W, Amling M, Barvencik F (2017) Clinical, radiographic and biochemical characteristics of adult hypophosphatasia. Osteoporos Int 28(9):2653–2662. https://doi.org/10.1007/s00198-017-4087-z
Koerbin G, Sikaris K, Jones GRD, Flatman R, Tate JR (2018) AACB Harmonization Committee for Common Reference Intervals An update report on the harmonization of adult reference intervals in Australasia. Clin Chem Lab Med 57(1):38–41. https://doi.org/10.1515/cclm-2017-0920
Quinn HB, Busch RS, Kane MP (2021) The occurrence and burden of hypophosphatasia in an ambulatory care endocrinology practice. Endocr Pract 27(12):1189–1192. https://doi.org/10.1016/j.eprac.2021.07.005
Alonso N, Larraz-Prieto B, Berg K, Lambert Z, Redmond P, Harris SE, Deary IJ, Pugh C, Prendergast J, Ralston SH (2020) Loss-of-function mutations in the ALPL gene presenting with adult onset osteoporosis and low serum concentrations of total alkaline phosphatase. J Bone Miner Res 35(4):657–661. https://doi.org/10.1002/jbmr.3928
Lum G (1995) Significance of low serum alkaline phosphatase activity in a predominantly adult male population. Clin Chem 41(4):515–518
Vieira LHR, Peixoto KC, Flósi CL, de Farias MLF, Madeira M (2021) Active search of adult patients with persistently low serum alkaline phosphatase levels for the diagnosis of hypophosphatasia. Arch Endocrinol Metab. 65(3):289–294. https://doi.org/10.20945/2359-3997000000347
McKiernan FE, Berg RL, Fuehrer J (2014) Clinical and radiographic findings in adults with persistent hypophosphatasemia. J Bone Miner Res 29(7):1651–1660. https://doi.org/10.1002/jbmr.2178
McKiernan FE, Shrestha LK, Berg RL, Fuehrer J (2014) Acute hypophosphatasemia. Osteoporos Int 25(2):519–523. https://doi.org/10.1007/s00198-013-2447-x
Napal J, Amado JA, Riancho JA, Olmos JM, Gonzàlez-Macìas J (1993) Stress decreases the serum level of osteocalcin. Bone Miner 21(2):113–118. https://doi.org/10.1016/S0169-6009(08)80013-X
Berkseth KE, Tebben PJ, Drake MT, Hefferan TE, Jewison DE, Wermers RA (2013) Clinical spectrum of hypophosphatasia diagnosed in adults. Bone 54(1):21–27. https://doi.org/10.1016/j.bone.2013.01.024
Maman E, Borderie D, Roux C, Briot K (2016) Absence of recognition of low alkaline phosphatase level in a tertiary care hospital. Osteoporos Int 27:1251–1254. https://doi.org/10.1007/s00198-015-3346-0
Deeb A, Elfatih A (2018) Could alerting physicians for low alkaline phosphatase levels be helpful in early diagnosis of hypophosphatasia? J Clin Res Pediatr Endocrinol 10(1):19–24. https://doi.org/10.4274/jcrpe.4426
Saraff V, Narayanan VK, Lawson AJ, Shaw NJ, Preece MA, Högler W (2016) A diagnostic algorithm for children with low alkaline phosphatase activities: lessons learned from laboratory screening for hypophosphatasia. J Pediatr 172:181–186. https://doi.org/10.1016/j.jpeds.2016.01.045
Hepp N, Frederiksen AL, Duno M, Præst Holm J, Rye Jørgensen N, Beck Jensen JE (2021) Biochemical, clinical and genetic characteristics in adults with persistent hypophosphatasaemia; data from an endocrinological outpatient clinic in Denmark. Bone Rep 15:101101. https://doi.org/10.1016/j.bonr.2021.101101
Riancho-Zarrabeitia L, García-Unzueta M, Tenorio JA, Gómez-Gerique JA, Ruiz Pérez VL, Heath KE, Lapunzina P, Riancho JA (2016) Clinical, biochemical and genetic spectrum of low alkaline phosphatase levels in adults. Eur J Intern Med 29:40–45. https://doi.org/10.1016/j.ejim.2015.12.019
McKiernan FE, Dong J, Berg RL, Scotty E, Mundt P, Larson L, Rai I (2017) Mutational and biochemical findings in adults with persistent hypophosphatasemia. Osteoporos Int 28(8):2343–2348. https://doi.org/10.1007/s00198-017-4035-y
Cundy T, Michigami T, Tachikawa K, Dray M, Collins JF, Paschalis EP, Gamsjaeger S, Roschger A, Fratzl-Zelman N, Roschger P, Klaushofer K (2015) Reversible deterioration in hypophosphatasia caused by renal failure with bisphosphonate treatment. J Bone Miner Res 30(9):1726–1737. https://doi.org/10.1002/jbmr.2495
Gagnon C, Sims NA, Mumm S, McAuley SA, Jung C, Poulton IJ, Ng KW, Ebeling PR (2010) Lack of sustained response to teriparatide in a patient with adult hypophosphatasia. J Clin Endocrinol Metab 95(3):1007–1012. https://doi.org/10.1210/jc.2009-1965
Lawrence JE, Saeed D, Bartlett J, Carrothers AD (2017) Adult-onset hypophosphatasia diagnosed following bilateral atypical femoral fractures in a 55-year-old woman. Clin Cases Miner Bone Metab. 14(3):347–53. https://doi.org/10.11138/ccmbm/2017.14.3.347
Rassie K, Dray M, Michigami T, Cundy T (2019) Bisphosphonate use and fractures in adults with hypophosphatasia. JBMR Plus 3(10):e10223. https://doi.org/10.1002/jbm4.10223
Desborough R, Nicklin P, Gossiel F, Balasubramanian M, Walsh JS, Petryk A, Teynor M, Eastell R (2021) Clinical and biochemical characteristics of adults with hypophosphatasia attending a metabolic bone clinic. Bone 144:115795. https://doi.org/10.1016/j.bone.2020.115795
Genest F, Seefried L (2018) Subtrochanteric and diaphyseal femoral fractures in hypophosphatasia - not atypical at all. Osteoporos Int 29(8):1815–1825. https://doi.org/10.1007/s00198-018-4552-3
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
PRE has received research funding from Alexion. All other authors declare no conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ng, E., Ashkar, C., Seeman, E. et al. A low serum alkaline phosphatase may signal hypophosphatasia in osteoporosis clinic patients. Osteoporos Int 34, 327–337 (2023). https://doi.org/10.1007/s00198-022-06597-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-022-06597-3