Abstract
Summary
Fractures are associated with increased long-term mortality in patients surviving to undergo baseline DXA. Notably, excess mortality risk does not decline with increasing time since prior hip or humerus fractures, even after accounting for comorbid medical conditions and other risk factors.
Introduction
Mortality risk increases following most types of fracture. In routine clinical practice, patients with prior fractures seen for dual-energy X-ray absorptiometry scan (DXA) are “survivors;” whether they remain at increased mortality risk is unknown. We tested the association between prior fracture and all-cause mortality, stratified by time since fracture, in patients undergoing baseline DXA.
Methods
We conducted a DXA registry-based cohort study and linked to population-based health services data for the Province of Manitoba, Canada. We identified women and men ≥ 40 years with minimum 10 years of prior healthcare coverage undergoing baseline DXA and ascertained prior fracture codes since 1984 and mortality to 2017. Time since prior fracture was calculated between the clinical encounter for the fracture and baseline DXA (index date). Cox proportional hazards models estimated hazard ratios for all-cause mortality in those with compared to those without prior fracture adjusted for (1) age and sex, and (2) age, sex, comorbidities, and other covariates.
Results
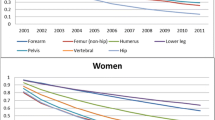
The study cohort consisted of 74,474 individuals (mean age 64.6 years, 89.7% female). During mean follow-up 9.2 years, we ascertained 14,923 (20.0%) deaths. Except for forearm fractures, all fracture sites were associated with increased mortality risk compared to those without prior fracture, even after multivariable adjustment. Excess mortality risk tended to decline slightly with time since fracture and was no longer significant > 10 years after vertebral fracture. However, excess mortality persisted > 10 years following hip or humerus fracture.
Conclusions
Prior fractures are associated with increased long-term mortality in patients surviving to undergo baseline DXA. Excess mortality risk does not decline with time since prior hip or humerus fractures, after accounting for potential confounders. Fracture prevention may have important long-term benefits preserving life expectancy.

Similar content being viewed by others
References
Center JR, Center JR, Nguyen TV et al (1999) Mortality after all major types of osteoporotic fracture in men and women: an observational study. Lancet 353:878–882
Cooper C, Atkinson EJ, Jacobsen SJ et al (1993) Population-based study of survival after osteoporotic fractures. Am J Epidemiol 137:1001–1005
Bliuc D, Nguyen ND, Milch VE et al (2009) Mortality risk associated with low-trauma osteoporotic fracture and subsequent fracture in men and women. JAMA 301:513–521
Abrahamsen B, van Staa T, Ariely R et al (2009) Excess mortality following hip fracture: a systematic epidemiological review. Osteoporos Int 20:1633–1650
Kanis JA, Oden A, Johnell O et al (2004) Excess mortality after hospitalisation for vertebral fracture. Osteoporos Int 15:108–112
Johnell O, Kanis JA (2004) An estimate of the worldwide prevalence, mortality and disability associated with hip fracture. Osteoporos Int 15:897–902
Morin S, Lix LM, Azimaee M et al (2011) Mortality rates after incident non-traumatic fractures in older men and women. Osteoporos Int 22:2439–2448
Harrington JT, Broy SB, Derosa AM et al (2002) Hip fracture patients are not treated for osteoporosis: a call to action. Arthritis Rheum 47:651–654
Barton DW, Behrend CJ, Carmouche JJ (2019) Rates of osteoporosis screening and treatment following vertebral fracture. Spine J 19:411–417
Cui Y, Lix LM, Yang S et al (2019) A population-based study of postfracture care in Manitoba, Canada 2000/2001-2014/2015. Osteoporos Int 30:2119–2127
Morin S, Lix LM, Azimaee M et al (2012) Institutionalization following incident non-traumatic fractures in community-dwelling men and women. Osteoporos Int 23:2381–2386
Bonafede M, Shi N, Barron R et al (2016) Predicting imminent risk for fracture in patients aged 50 or older with osteoporosis using US claims data. Arch Osteoporos 11:26
Banefelt J, Åkesson KE, Spångéus A et al (2019) Risk of imminent fracture following a previous fracture in a Swedish database study. Osteoporos Int 30:601–609
Balasubramanian A, Zhang J, Chen L et al (2019) Risk of subsequent fracture after prior fracture among older women. Osteoporos Int 30:79–92
Johansson H, Siggeirsdóttir K, Harvey NC et al (2017) Imminent risk of fracture after fracture. Osteoporos Int 28:775–780
Leslie WD, MacWilliam L, Lix L et al (2005) A population-based study of osteoporosis testing and treatment following introduction of a new bone densitometry service. Osteoporos Int 16:773–782
Leslie WD, Caetano PA, Macwilliam LR, Finlayson GS (2005) Construction and validation of a population-based bone densitometry database. J Clin Densitom 8:25–30
Lix LM, Azimaee M, Osman BA et al (2012) Osteoporosis-related fracture case definitions for population-based administrative data. BMC Public Health 12:301
Epp R, Alhrbi M, Ward L, Leslie WD (2018) Radiological validation of fracture definitions from administrative data. J Bone Miner Res 33(Supp 1):S275
Looker AC, Wahner HW, Dunn WL et al (1995) Proximal femur bone mineral levels of US adults. Osteoporos Int 5:389–409
(1994) Assessment of fracture risk and its application to screening for postmenopausal osteoporosis. Report of a WHO Study Group. World Health Organ Tech Rep Ser 843:1–129
Lix LM, Yogendran MS, Shaw SY et al (2008) Population-based data sources for chronic disease surveillance. Chronic Dis Can 29:31–38
Blanchard JF, Ludwig S, Wajda A et al (1996) Incidence and prevalence of diabetes in Manitoba, 1986–1991. Diabetes Care 19:807–811
Leslie WD, Lix LM, Johansson H et al (2010) Independent clinical validation of a Canadian FRAX tool: fracture prediction and model calibration. J Bone Miner Res 25:2350–2358
Fraser L-A, CaMos Research Group, Langsetmo L et al (2011) Fracture prediction and calibration of a Canadian FRAX® tool: a population-based report from CaMos. Osteoporos Int 22:829–837
Dagan N, Cohen-Stavi C, Leventer-Roberts M, Balicer RD (2017) External validation and comparison of three prediction tools for risk of osteoporotic fractures using data from population based electronic health records: retrospective cohort study. BMJ 356:i6755
(2005) WHO Collaborating Centre for Drug Statistics Methodology. (eds), Guidelines for ATC classification and DDD assignment. Oslo
The Johns Hopkins Ambulatory Care Groups(R) System, Version 9.0, Reference Manual, Johns Hopkins Bloomberg School of Public Health, 2009
Reid RJ, Roos NP, MacWilliam L et al (2002) Assessing population health care need using a claims-based ACG morbidity measure: a validation analysis in the Province of Manitoba. Health Serv Res 37:1345–1364
Manitoba Centre for Health, Concept: Urban / Rural Definitions, 2002. http://mchp-appserv.cpe.umanitoba.ca/viewConcept.php?conceptID=1253. Accessed 5 Jul 2021
Manitoba Centre for Health Policy, Term: Income Quintiles / Income Quintile, 2013. http://mchp-appserv.cpe.umanitoba.ca/viewDefinition.php?definitionID=102882. Accessed 5 Jul 2021
Tosteson ANA, Gottlieb DJ, Radley DC et al (2007) Excess mortality following hip fracture: the role of underlying health status. Osteoporos Int 18:1463–1472
Walker N, Norton R, Vander Hoorn S et al (1999) Mortality after hip fracture: regional variations in New Zealand. N Z Med J 112:269–271
Wolinsky FD, Fitzgerald JF, Stump TE (1997) The effect of hip fracture on mortality, hospitalization, and functional status: a prospective study. Am J Public Health 87:398–403
Haentjens P, Magaziner J, Colón-Emeric CS et al (2010) Meta-analysis: excess mortality after hip fracture among older women and men. Ann Intern Med 152:380–390
Kannegaard PN, van der Mark S, Eiken P, Abrahamsen B (2010) Excess mortality in men compared with women following a hip fracture. National analysis of comedications, comorbidity and survival. Age Ageing 39:203–209
Endo Y, Aharonoff GB, Zuckerman JD et al (2005) Gender differences in patients with hip fracture: a greater risk of morbidity and mortality in men. J Orthop Trauma 19:29–35
Fransen M, Woodward M, Norton R et al (2002) Excess mortality or institutionalization after hip fracture: men are at greater risk than women. J Am Geriatr Soc 50:685–690
Leslie WD, Schousboe JT, Morin SN et al (2020) Fracture risk following high-trauma versus low-trauma fracture: a registry-based cohort study. Osteoporos Int 31:1059–1067
Mackey DC, Lui L-Y, Cawthon PM et al (2007) High-trauma fractures and low bone mineral density in older women and men. JAMA 298:2381–2388
Sanders KM, Pasco JA, Ugoni AM et al (1998) The exclusion of high trauma fractures may underestimate the prevalence of bone fragility fractures in the community: the Geelong Osteoporosis Study. J Bone Miner Res 13:1337–1342
Acknowledgements
The authors acknowledge the Manitoba Centre for Health Policy for use of data contained in the Population Health Research Data Repository (HIPC 2016/2017-29). The results and conclusions are those of the authors and no official endorsement by the Manitoba Centre for Health Policy, Manitoba Health, Seniors and Active Living, or other data providers is intended or should be inferred. This work has been reviewed and approved by the members of the Manitoba Bone Density Program Committee.
Funding
SNM is chercheur-boursier des Fonds de Recherche du Québec en Santé. LML is supported by a Tier I Canada Research Chair. No funding was received for this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ye, C., Schousboe, J.T., Morin, S.N. et al. Time since prior fracture affects mortality at the time of clinical assessment: a registry-based cohort study. Osteoporos Int 33, 1257–1264 (2022). https://doi.org/10.1007/s00198-021-06236-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-021-06236-3