Abstract
Summary
A comprehensive review of studies shows that patients with wrist fracture, aged over 50 years, experience pain and functional limitation long after fracture. This is associated with increased healthcare costs, and reduced quality of life. Understanding factors that predict poor outcomes is important for future healthcare policy and planning.
Purpose
To summarise and appraise evidence on the prognosis and long-term clinical and socio-economic outcomes following wrist fracture among adults aged 50 years and over.
Methods
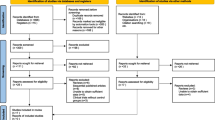
Five databases (MEDLINE, EMBASE, AMED, CINAHL-P and PsycINFO) were comprehensively searched (supplemented by a grey-literature search) from inception till June 2021 for prospective/retrospective cohort studies of patients (≥ 50 years) with a history of wrist fracture and reporting long-term (≥ 6 months) outcomes. Peer study selection, data extraction and risk of bias assessment were conducted. A random effects meta-analysis was used to summarise estimates of pain and function outcomes.
Results
78 studies (n = 688,041 patients) were included. Patients report persistent moderate to severe pain (range: 7.5%-62%) and functional limitations (range: 5.5–78%) up to 12-months or later after wrist fracture. Mean Patient-Rated Wrist Evaluation (PRWE) score for pain and function (9 studies, n = 1759 patients) was 15.23 (95%CI 12.77, 17.69) at 6-months to 13-years follow-up. Mean disabilities of the arm, shoulder and hand (DASH) score (9 studies, n = 1346 patients) was 13.82 (95%CI 12.71, 14.93)( at 6- to 17-months follow-up. A 10–20% increase in healthcare encounters in the first 12-months after fracture was observed. Twelve prognostic factors were associated with poor long-term outcomes.
Conclusion
Evidence shows that a high proportion of people aged over 50 years with wrist fracture experience pain and functional limitation > 6 months after fracture. This is associated with increased healthcare costs, and reduced quality of life. Exploratory evidence was found for several candidate prognostic factors. Their predictive performance needs to be investigated further.
PROSPERO: CRD42018116478




Similar content being viewed by others
References
Scholes S, Panesar S, Shelton NJ, Francis RM, Mirza S, Mindell JS, Donaldson LJ (2014) Epidemiology of lifetime fracture prevalence in England: a population study of adults aged 55 years and over. Age Ageing 43(2):234–240. https://doi.org/10.1093/ageing/aft167
Curtis EM, van der Velde R, Moon RJ, van den Bergh JP, Geusens P, de Vries F, van Staa TP, Cooper C, Harvey NC (2016) Epidemiology of fractures in the United Kingdom 1988–2012: variation with age, sex, geography, ethnicity and socioeconomic status. Bone 87:19–26. https://doi.org/10.1016/j.bone.2016.03.006
O’Neill TW, Cooper C, Finn JD, Lunt M, Purdie D, Reid DM, Rowe R, Woolf AD, Wallace WA, UK Colles’ Fracture Study Group (2001) Incidence of distal forearm fracture in British men and women. Osteoporos Int 12(7):555–558. https://doi.org/10.1007/s001980170076
Ong T, Sahota O, Marshall L (2015) Epidemiology of appendicular skeletal fractures: a cross-sectional analysis of data from the Nottingham Fracture Liaison Service. J Orthop Sci 20(3):517–521. https://doi.org/10.1007/s00776-015-0700-1
van Staa TP et al (2001) Epidemiology of fractures in England and Wales. Bone 29(6):517–22. https://doi.org/10.1016/s8756-3282(01)00614-7
Hernlund E, Svedbom A, Ivergård M, Compston J, Cooper C, Stenmark J, McCloskey EV, Jönsson B, Kanis JA (2013) Osteoporosis in the European Union: medical management, epidemiology and economic burden. A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos 8(1):136. https://doi.org/10.1007/s11657-013-0136-1
Svedbom A, Hernlund E, Ivergård M, Compston J, Cooper C, Stenmark J, McCloskey EV, Jönsson B, Kanis JA, EU Review Panel of IOF (2013) Osteoporosis in the European Union: a compendium of country-specific reports. Arch Osteoporos 8(1):137. https://doi.org/10.1007/s11657-013-0137-0
Ioannidis G, Flahive J, Pickard L, Papaioannou A, Chapurlat RD, Saag KG, Silverman S, Anderson FA Jr, Gehlbach SH, Hooven FH, Boonen S, Compston JE, Cooper C, Díez-Perez A, Greenspan SL, Lacroix AZ, Lindsay R, Netelenbos JC, Pfeilschifter J, Rossini M, Roux C, Sambrook PN, Siris ES, Watts NB, Adachi JD, Investigators GLOW (2013) Non-hip, non-spine fractures drive healthcare utilization following a fracture: the Global Longitudinal Study of Osteoporosis in Women (GLOW). Osteoporos Int 24(1):59–67. https://doi.org/10.1007/s00198-012-1968-z
Edwards BJ, Song J, Dunlop DD, Fink HA, Cauley JA (2010) Functional decline after incident wrist fractures—study of osteoporotic fractures: prospective cohort study. BMJ 341:c3324. https://doi.org/10.1136/bmj.c3324
González N, Antón-Ladislao A, Orive M, Zabala J, García-Gutiérrez S, Las Hayas C, Quintana JM, OFF (Older Falls Fracture)-IRYSS Group (2016) Factors related to a decline in upper extremity function among patients with a wrist fracture due to a fall. Int J Clin Pract 70(11):930–939. https://doi.org/10.1111/ijcp.12880
Vergara I, Vrotsou K, Orive M, Garcia-Gutierrez S, Gonzalez N, Las Hayas C, Quintana JM (2016) Wrist fractures and their impact in daily living functionality on elderly people: a prospective cohort study. BMC Geriatr 16:11. https://doi.org/10.1186/s12877-015-0176-z
Vogt MT, Cauley JA, Tomaino MM, Stone K, Williams JR, Herndon JH (2002) Distal radius fractures in older women: a 10-year follow-up study of descriptive characteristics and risk factors. The study of osteoporotic fractures. J Am Geriatr Soc 50(1):97–103. https://doi.org/10.1046/j.1532-5415.2002.50014.x
MacIntyre NJ, Dewan N (2016) Epidemiology of distal radius fractures and factors predicting risk and prognosis. J Hand Ther 29(2):136–145. https://doi.org/10.1016/j.jht.2016.03.003
Földhazy Z, Törnkvist H, Elmstedt E, Andersson G, Hagsten B, Ahrengart L (2007) Long-term outcome of non-surgically treated distal radius fractures. J Hand Surg 32(9):1374–1384. https://doi.org/10.1016/j.jhsa.2007.08.019
Nordell E, Kristinsdottir EK, Jarnlo GB, Magnusson M, Thorngren KG (2005) Older patients with distal forearm fracture. A challenge to future fall and fracture prevention. Aging Clin Exp Res 17(2):90–95. https://doi.org/10.1007/BF03324579
Noredll E, Jarnlo GB, Thorngren KG (2003) Decrease in physical function after fall-related distal forearm fracture in elderly women. Adv Physiother 5(4):146–154. https://doi.org/10.1080/14038190310016788
Borgström F, Lekander I, Ivergård M, Ström O, Svedbom A, Alekna V, Bianchi ML, Clark P, Curiel MD, Dimai HP, Jürisson M, Kallikorm R, Lesnyak O, McCloskey E, Nassonov E, Sanders KM, Silverman S, Tamulaitiene M, Thomas T, Tosteson AN, Jönsson B, Kanis JA (2013) The International Costs and Utilities Related to Osteoporotic Fractures Study (ICUROS)—quality of life during the first 4 months after fracture. Osteoporos Int 24(3):811–823. https://doi.org/10.1007/s00198-012-2240-2
Kasapinova K, Kamiloski V (2009) Pain and disability during six months in patients with a distal radius fracture. Prilozi 30(2):185–196
Friesgaard KD, Gromov K, Knudsen LF, Brix M, Troelsen A, Nikolajsen L (2016) Persistent pain is common 1 year after ankle and wrist fracture surgery: a register-based questionnaire study. Br J Anaesth 116(5):655–661. https://doi.org/10.1093/bja/aew069
Mehta SP, MacDermid JC, Richardson J, MacIntyre NJ, Grewal R (2015) Baseline pain intensity is a predictor of chronic pain in individuals with distal radius fracture. J Orthop Sports Phys Ther 45(2):119–127. https://doi.org/10.2519/jospt.2015.5129
Moore CM, Leonardi-Bee J (2008) The prevalence of pain and disability one year post fracture of the distal radius in a UK population: a cross sectional survey. BMC Musculoskelet Disord 9:129. https://doi.org/10.1186/1471-2474-9-129
MacDermid JC, Donner A, Richards RS, Roth JH (2002) Patient versus injury factors as predictors of pain and disability six months after a distal radius fracture. J Clin Epidemiol 55(9):849–854. https://doi.org/10.1016/s0895-4356(02)00445-6
Li Z, Smith BP, Tuohy C, Smith TL, Koman LA (2010) Complex regional pain syndrome after hand surgery. Hand Clin 26(2):281–289. https://doi.org/10.1016/j.hcl.2009.11.001
Bienek T, Kusz D, Cielinski L (2006) Peripheral nerve compression neuropathy after fractures of the distal radius. J Hand Surg Br 31(3):256–260. https://doi.org/10.1016/j.jhsb.2005.09.021
Kamath J, Jayasheelan N, Mathews R (2016) Compressive neuropathy of the palmar cutaneous branch of the median nerve after a malunited fracture of the distal radius. J Hand Surg Eur 41(2):231–232. https://doi.org/10.1177/1753193415572800
Megerle K, Baumgarten A, Schmitt R, van Schoonhoven J, Prommersberger KJ (2013) Median neuropathy in malunited fractures of the distal radius. Arch Orthop Trauma Surg 133(9):1321–1327. https://doi.org/10.1007/s00402-013-1803-9
Vance RM, Gelberman RH (1978) Acute ulnar neuropathy with fractures at the wrist. J Bone Joint Surg Am 60(7):962–965
Ahmed LA, Schirmer H, Bjørnerem A, Emaus N, Jørgensen L, Størmer J, Joakimsen RM (2009) The gender- and age-specific 10-year and lifetime absolute fracture risk in Tromsø, Norway. Eur J Epidemiol 24(8):441–448. https://doi.org/10.1007/s10654-009-9353-8
Singer BR, McLauchlan GJ, Robinson CM, Christie J (1998) Epidemiology of fractures in 15,000 adults: the influence of age and gender. J Bone Joint Surg Br 80(2):243–248. https://doi.org/10.1302/0301-620x.80b2.7762
Cummings SR, Black DM, Rubin SM (1989) Lifetime risks of hip, Colles’, or vertebral fracture and coronary heart disease among white postmenopausal women. Arch Intern Med 149(11):2445–2448
Amorosa LF, Vitale MA, Brown S, Kaufmann RA (2011) A functional outcomes survey of elderly patients who sustained distal radius fractures. Hand (N Y) 6(3):260–267. https://doi.org/10.1007/s11552-011-9327-7
Cooper C (2009) The Global Longitudinal Registry of Osteoporosis in Women (GLOW): regional differences in risk factors and fragility fractures. Osteoporos Int 20:183–184
Cowie J, Anakwe R, McQueen M (2015) Factors associated with one-year outcome after distal radial fracture treatment. J Orthop Surg (Hong Kong) 23(1):24–28. https://doi.org/10.1177/230949901502300106
Crandall CJ, Hovey KM, Cauley JA, Andrews CA, Curtis JR, Wactawski-Wende J, Wright NC, Li W, LeBoff MS (2015) Wrist fracture and risk of subsequent fracture: findings from the women’s health initiative study. J Bone Miner Res 30(11):2086–2095. https://doi.org/10.1002/jbmr.2559
Mehta SP (2012) Predicting risk for adverse outcomes following distal radius fracture. Dissertation, McMaster University
Hayden JA, van der Windt DA, Cartwright JL, Côté P, Bombardier C (2013) Assessing bias in studies of prognostic factors. Ann Intern Med 158(4):280–286. https://doi.org/10.7326/0003-4819-158-4-201302190-00009
Grooten WJA, Tseli E, Äng BO, Boersma K, Stålnacke BM, Gerdle B, Enthoven P (2019) Elaborating on the assessment of the risk of bias in prognostic studies in pain rehabilitation using QUIPS-aspects of interrater agreement. Diagn Progn Res 3:5. https://doi.org/10.1186/s41512-019-0050-0
Hozo SP, Djulbegovic B, Hozo I (2005) Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol 5:13. https://doi.org/10.1186/1471-2288-5-13
Higgins JPT, Green S (2008) Cochrane handbook for systematic reviews of interventions. Wiley, Chichester
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7:177e88. https://doi.org/10.1016/0197-2456(86)90046-2
Iorio A, Spencer FA, Falavigna M, Alba C, Lang E, Burnand B, McGinn T, Hayden J, Williams K, Shea B, Wolff R, Kujpers T, Perel P, Vandvik PO, Glasziou P, Schunemann H, Guyatt G (2015) Use of GRADE for assessment of evidence about prognosis: rating confidence in estimates of event rates in broad categories of patients. BMJ 350:h870. https://doi.org/10.1136/bmj.h870
Huguet A, Hayden JA, Stinson J, McGrath PJ, Chambers CT, Tougas ME, Wozney L (2013) Judging the quality of evidence in reviews of prognostic factor research: adapting the GRADE framework. Syst Rev 2:71. https://doi.org/10.1186/2046-4053-2-71
Foroutan F, Guyatt G, Zuk V, Vandvik PO, Alba AC, Mustafa R, Vernooij R, Arevalo-Rodriguez I, Munn Z, Roshanov P, Riley R, Schandelmaier S, Kuijpers T, Siemieniuk R, Canelo-Aybar C, Schunemann H, Iorio A (2020) GRADE guidelines 28: use of GRADE for the assessment of evidence about prognostic factors: rating certainty in identification of groups of patients with different absolute risks. J Clin Epidemiol 121:62–70. https://doi.org/10.1016/j.jclinepi.2019.12.023
Bhattacharyya R, Morgan BS, Mukherjee P, Royston S (2014) Distal radial fractures: the significance of the number of instability markers in management and outcome. Iowa Orthop J 34:118–122
Bickerstaff DR, Kanis JA (1994) Algodystrophy: an under-recognized complication of minor trauma. Br J Rheumatol 33(3):240–248. https://doi.org/10.1093/rheumatology/33.3.240
Field J, Gardner FV (1997) Psychological distress associated with algodystrophy. J Hand Surg Br 22(1):100–101. https://doi.org/10.1016/s0266-7681(97)80030-7
McQueen M, Caspers J (1988) Colles fracture: does the anatomical result affect the final function? J Bone Joint Surg Br 70(4):649–651. https://doi.org/10.1302/0301-620X.70B4.3403617
Roysam GS (1993) The distal radio-ulnar joint in Colles’ fractures. J Bone Joint Surg Br 75(1):58–60. https://doi.org/10.1302/0301-620X.75B1.8421035
Cantlon MB, Marcano AI, Lee J, Egol KA (2016) Does malunion in multiple planes predict worse functional outcomes in distal radial fractures? Curr Orthop Pract 27(4):371–374. https://doi.org/10.1097/BCO.0000000000000398
Lübbeke A, Stern R, Grab B, Herrmann F, Michel JP, Hoffmeyer P (2005) Upper extremity fractures in the elderly: consequences on utilization of rehabilitation care. Aging Clin Exp Res 17(4):276–280. https://doi.org/10.1007/BF03324610
Hollevoet N, Goemaere S, Mortier F, Van Bouchaute P, Kaufman JM, Verdonk R (2000) The role of osteoporosis in distal radius fractures. Acta Orthop Belg 66(2):163–168
Crandall CJ, Hunt RP, LaCroix AZ, Robbins JA, Wactawski-Wende J, Johnson KC, Sattari M, Stone KL, Weitlauf JC, Gure TR, Cauley JA (2021) After the initial fracture in postmenopausal women, where do subsequent fractures occur? EClinicalMedicine 35:100826. https://doi.org/10.1016/j.eclinm.2021.100826
Alsubheen SA, MacDermid JC, Walton DM, Grewal R (2019) The effect of diabetes on functional outcomes among individuals with distal radial fractures. J Hand Ther 32(4):476–482. https://doi.org/10.1016/j.jht.2018.02.008
Brogren E, Hofer M, Petranek M, Dahlin LB, Atroshi I (2011) Fractures of the distal radius in women aged 50 to 75 years: natural course of patient-reported outcome, wrist motion and grip strength between 1 year and 2–4 years after fracture. J Hand Surg Eur 36(7):568–576. https://doi.org/10.1177/1753193411409317
Crockett K, Kontulainen SA, Farthing JP, Chilibeck PD, Bath B, Baxter-Jones ADG, Arnold CM (2018) Differences in function and fracture risk in postmenopausal women with and without a recent distal radius fracture. J Aging Phys Act 26(1):136–145. https://doi.org/10.1123/japa.2016-0132
Dewan N, MacDermid JC, Grewal R, Beattie K (2018) Risk factors predicting subsequent falls and osteoporotic fractures at 4 years after distal radius fracture-a prospective cohort study. Arch Osteoporos 13(1):32. https://doi.org/10.1007/s11657-018-0445-5
Dewan N, MacDermid JC, Grewal R, Beattie K (2018) Recovery patterns over 4 years after distal radius fracture: descriptive changes in fracture-specific pain/disability, fall risk factors, bone mineral density, and general health status. J Hand Ther 31(4):451–464. https://doi.org/10.1016/j.jht.2017.06.009
Langenberg R (1991) Die differenzierte Behandlung von distalen Radiusfrakturen. Ergebnisse einer prospektiven Studie [Variable treatment of distal radius fractures. Results of a prospective study]. Unfallchirurg 94(9):482–485
Larouche J, Pike J, Slobogean GP, Guy P, Broekhuyse H, O’Brien P, Lefaivre KA (2016) Determinants of functional outcome in distal radius fractures in high-functioning patients older than 55 years. J Orthop Trauma 30(8):445–449. https://doi.org/10.1097/BOT.0000000000000566
Lutz K, Yeoh KM, MacDermid JC, Symonette C, Grewal R (2014) Complications associated with operative versus nonsurgical treatment of distal radius fractures in patients aged 65 years and older. J Hand Surg Am 39(7):1280–1286. https://doi.org/10.1016/j.jhsa.2014.04.018
MacDermid JC, Richards RS, Roth JH (2001) Distal radius fracture: a prospective outcome study of 275 patients. J Hand Ther 14(2):154–169. https://doi.org/10.1016/s0894-1130(01)80046-6
Modarresi S, Suh N, Walton DM, MacDermid JC (2019) Depression affects the recovery trajectories of patients with distal radius fractures: a latent growth curve analysis. Musculoskelet Sci Pract 43:96–102. https://doi.org/10.1016/j.msksp.2019.07.012
Nielsen TL, Dekkers MK (2013) Progress and prediction of occupational performance in women with distal radius fractures: a one-year follow-up. Scand J Occup Ther 20(2):143–151. https://doi.org/10.3109/11038128.2012.748823
Solgaard S (1988) Function after distal radius fracture. Acta Orthop Scand 59(1):39–42. https://doi.org/10.3109/17453678809149341
Synn AJ, Makhni EC, Makhni MC, Rozental TD, Day CS (2009) Distal radius fractures in older patients: is anatomic reduction necessary? Clin Orthop Relat Res 467(6):1612–1620. https://doi.org/10.1007/s11999-008-0660-2
Symonette CJ, MacDermid JC, Grewal R (2019) Radiographic thresholds with increased odds of a poor outcome following distal radius fractures in patients over 65 years old. J Hand Surg Glob Online 1(2):65–69. https://doi.org/10.1016/j.jhsg.2019.02.002
van Leerdam RH, Huizing F, Termaat F, Kleinveld S, Rhemrev SJ, Krijnen P, Schipper IB (2019) Patient-reported outcomes after a distal radius fracture in adults: a 3–4 years follow-up. Acta Orthop 90(2):129–134. https://doi.org/10.1080/17453674.2019.1568098
Ziebart C, Macdermid JC, Suh N (2020) Effects of gender, age, and time on wrist pain up to two years following distal radius fracture. Crit Rev Phys Rehabil Med 32(2):85–96. https://doi.org/10.1615/CritRevPhysRehabilMed.2020034189
Abramo A, Kopylov P, Tagil M (2008) Evaluation of a treatment protocol in distal radius fractures: a prospective study in 581 patients using DASH as outcome. Acta Orthop 79(3):376–385. https://doi.org/10.1080/17453670710015283
Egund L, McGuigan FE, Egund N, Besjakov J, Akesson KE (2020) Patient-related outcome, fracture displacement and bone mineral density following distal radius fracture in young and older men. BMC Musculoskelet Disord 21(1):816. https://doi.org/10.1186/s12891-020-03843-9
Hung LP, Leung YF, Ip WY, Lee YL (2015) Is locking plate fixation a better option than casting for distal radius fracture in elderly people? Hong Kong Med J 21(5):407–410. https://doi.org/10.12809/hkmj144440
Jakob M, Mielke S, Keller H, Metzger U (1999) Therapieergebnisse nach primär konservativer Versorgung distaler Radiusfrakturen bei Patienten im Alter von über 65 Jahren [Results of therapy after primary conservative management of distal radius fractures in patients over 65 years of age]. Handchir Mikrochir Plast Chir 31(4):241–245. https://doi.org/10.1055/s-1999-13532
Jansky W, Laminger K, Iqbal M, Seeger T (1994) Klinische und radiologische Ergebnisse von handgelenknahen Speichenbrüchen [Clinical and radiological results of distal radius fractures]. Unfallchirurgie 20(4):197–202. https://doi.org/10.1007/BF02588712
Yeoh JC, Pike JM, Slobogean GP, O’Brien PJ, Broekhuyse HM, Lefaivre KA (2016) Role of depression in outcomes of low-energy distal radius fractures in patients older than 55 years. J Orthop Trauma 30(5):228–233. https://doi.org/10.1097/BOT.0000000000000514
Abimanyi-Ochom J, Watts JJ, Borgström F, Nicholson GC, Shore-Lorenti C, Stuart AL, Zhang Y, Iuliano S, Seeman E, Prince R, March L, Cross M, Winzenberg T, Laslett LL, Duque G, Ebeling PR, Sanders KM (2015) Changes in quality of life associated with fragility fractures: Australian arm of the International Cost and Utility Related to Osteoporotic Fractures Study (AusICUROS). Osteoporos Int 26(6):1781–1790. https://doi.org/10.1007/s00198-015-3088-z
Brenneman SK, Barrett-Connor E, Sajjan S, Markson LE, Siris ES (2006) Impact of recent fracture on health-related quality of life in postmenopausal women. J Bone Miner Res 21(6):809–816. https://doi.org/10.1359/jbmr.060301
Hagino H, Nakamura T, Fujiwara S, Oeki M, Okano T, Teshima R (2009) Sequential change in quality of life for patients with incident clinical fractures: a prospective study. Osteoporos Int 20(5):695–702. https://doi.org/10.1007/s00198-008-0761-5
Lee JW, Lee YB, Kwon BC, Yoo JH, Choi HG (2019) Mortality and cause of death in distal radius fracture patients: a longitudinal follow-up study using a national sample cohort. Medicine 98(52):e18604. https://doi.org/10.1097/MD.0000000000018604
Tsukutani Y, Hagino H, Ito Y, Nagashima H (2015) Epidemiology of fragility fractures in Sakaiminato, Japan: incidence, secular trends, and prognosis. Osteoporos Int 26(9):2249–2255. https://doi.org/10.1007/s00198-015-3124-z
González N, Aguirre U, Orive M, Zabala J, García-Gutiérrez S, Las Hayas C, Navarro G, Quintana JM (2014) Health-related quality of life and functionality in elderly men and women before and after a fall-related wrist fracture. Int J Clin Pract 68(7), 919–928. DOI: 10.1111/ijcp.12410. & González Y, Sicras A, Larraínzar R, Sorio F, Canals L, Lizán L, Calvo E (2015) Estimación de los costes sanitarios relacionados con las fracturas osteoporóticas en pacientes posmenopáusicas en España [Estimation of healthcare costs associated with osteoporotic fractures in postmenopausal patients in Spain]. PharmacoEcon Span Res Artic 12:1–9. https://doi.org/10.1007/s40277-014-0029-8
Borgström F, Zethraeus N, Johnell O, Lidgren L, Ponzer S, Svensson O, Abdon P, Ornstein E, Lunsjö K, Thorngren KG, Sernbo I, Rehnberg C, Jönsson B (2006) Costs and quality of life associated with osteoporosis-related fractures in Sweden. Osteoporos Int 17(5):637–650. https://doi.org/10.1007/s00198-005-0015-8
Shauver MJ, Zhong L, Chung KC (2015) Mortality after distal radial fractures in the Medicare population. J Hand Surg Eur 40(8):805–181. https://doi.org/10.1177/1753193415589735
Bynum JPW, Bell JE, Cantu RV, Wang Q, McDonough CM, Carmichael D, Tosteson TD, Tosteson ANA (2016) Second fractures among older adults in the year following hip, shoulder, or wrist fracture. Osteoporos Int 27(7):2207–2215. https://doi.org/10.1007/s00198-016-3542-6
Chen CW, Huang TL, Su LT, Kuo YC, Wu SC, Li CY, Chen KB, Sung FC (2013) Incidence of subsequent hip fractures is significantly increased within the first month after distal radius fracture in patients older than 60 years. J Trauma Acute Care Surg 74(1):317–321. https://doi.org/10.1097/ta.0b013e31824bb325
Clement ND, Aitken S, Duckworth AD, McQueen MM, Court-Brown CM (2012) Multiple fractures in the elderly. J Bone Joint Surg Br 94(2):231–236. https://doi.org/10.1097/10.1302/0301-620X.94B2.27381
Endres HG, Dasch B, Lungenhausen M, Maier C, Smektala R, Trampisch HJ, Pientka L (2006) Patients with femoral or distal forearm fracture in Germany: a prospective observational study on health care situation and outcome. BMC Public Health 6:87. https://doi.org/10.1186/1471-2458-6-87
Johnell O, Kanis JA, Odén A, Sernbo I, Redlund-Johnell I, Petterson C, De Laet C, Jönsson B (2004) Mortality after osteoporotic fractures. Osteoporos Int 15(1):38–42. https://doi.org/10.1007/s00198-003-1490-4
Morin S, Lix LM, Azimaee M, Metge C, Caetano P, Leslie WD (2011) Mortality rates after incident non-traumatic fractures in older men and women. Osteoporos Int 22(9):2439–2448. https://doi.org/10.1007/s00198-010-1480-2
Øyen J, Diamantopoulos AP, Haugeberg G (2014) Mortality after distal radius fracture in men and women aged 50 years and older in southern Norway. PLoS ONE 9(11):e112098. https://doi.org/10.1371/journal.pone.0112098
Jung HS, Jang S, Chung HY, Park SY, Kim HY, Ha YC, Lee YK, Nho JH (2021) Incidence of subsequent osteoporotic fractures after distal radius fractures and mortality of the subsequent distal radius fractures: a retrospective analysis of claims data of the Korea National Health Insurance Service. Osteoporos Int 32(2):293–299. https://doi.org/10.1007/s00198-020-05609-4
Luthje P, Nurmi-Luthje I, Tavast N, Villikka A, Kataja M (2021) Evaluation of minimal fracture liaison service resource: costs and survival in secondary fracture prevention-a prospective one-year study in South-Finland. Aging Clin Exp Res. https://doi.org/10.1007/s40520-021-01826-x. Online ahead of print
Marchewka J, Glodzik J, Marchewka W, Golec E (2019) Higher mortality in men compared with women following distal radius fracture in population aged 50 years or above: are common distal radius fracture classifications useful in predicting mortality? Biomed Res Int 2019:5359204. https://doi.org/10.1155/2019/5359204
Montoya-Garcia MJ, Giner M, Marcos R, Garcia-Romero D, Olmo-Montes FJ, Miranda MJ, Hernandez-Cruz B, Colmenero MA, Vazquez-Gamez MA (2021) Fragility fractures and imminent fracture risk in the Spanish population: a retrospective observational cohort study. J Clin Med 10(5):1–11. https://doi.org/10.3390/jcm10051082
Parikh K, Reinhardt D, Templeton K, Toby B, Brubacher J (2021) Rate of bone mineral density testing and subsequent fracture-free interval after distal forearm fracture in the Medicare population. J Hand Surg 46(4):267–277. https://doi.org/10.1016/j.jhsa.2020.11.020
Sujic R, Beaton DE, Mamdani M, Cadarette SM, Luo J, Jaglal S, Sale JEM, Jain R, Bogoch E, Ontario Osteoporosis Strategy Fracture Screening and Prevention Program Evaluation (2019) Five-year refracture rates of a province-wide fracture liaison service. Osteoporos Int 30(8):1671–1677. https://doi.org/10.1007/s00198-019-05017-3
Sujic R, Luo J, Beaton DE, Bogoch ER, Sale JEM, Jaglal S, Jain R, Mamdani M, Ontario Osteoporosis Strategy Fracture Screening and Prevention Program Evaluation (2020) Multiple simultaneous fractures are associated with higher all-cause mortality: results from a province-wide fracture liaison service. Osteoporos Int 31(2):291–296. https://doi.org/10.1007/s00198-019-05207-z
Toth E, Banefelt J, Akesson K, Spangeus A, Ortsater G, Libanati C (2020) History of previous fracture and imminent fracture risk in Swedish women aged 55 to 90 years presenting with a fragility fracture. J Bone Miner Res 35(5):861–868. https://doi.org/10.1002/jbmr.3953
Yoo JI, Ha YC, Park KS, Kim RB, Seo SH, Koo KH (2019) Incidence and mortality of osteoporotic refractures in Korea according to nationwide claims data. Yonsei Med J 60(10):969–975. https://doi.org/10.3349/ymj.2019.60.10.969
Becker DJ, Yun H, Kilgore ML, Curtis JR, Delzell E, Gary LC, Saag KG, Morrisey MA (2010) Health services utilization after fractures: evidence from Medicare. J Gerontol A Biol Sci Med Sci 65(9):1012–1020. https://doi.org/10.1093/gerona/glq093
Freedman BA, Potter BK, Nesti LJ, Cho T, Kuklo TR (2007) Missed opportunities in patients with osteoporosis and distal radius fractures. Clin Orthop Relat Res 454(202–206):1020. https://doi.org/10.1097/01.blo.0000238866
Leslie WD, Metge CJ, Azimaee M, Lix LM, Finlayson GS, Morin SN, Caetano P (2011) Direct costs of fractures in Canada and trends 1996–2006: a population-based cost-of-illness analysis. J Bone Miner Res 26(10):2419–2429. https://doi.org/10.1002/jbmr.457
Ohsfeldt RL, Borisov NN, Sheer RL (2006) Fragility fracture-related direct medical costs in the first year following a nonvertebral fracture in a managed care setting. Osteoporos Int 17(2):252–258. https://doi.org/10.1007/s00198-005-1993-2
Eekman DA, ter Wee MM, Coupé VM, Erisek-Demirtas S, Kramer MH, Lems WF (2014) Indirect costs account for half of the total costs of an osteoporotic fracture: a prospective evaluation. Osteoporos Int 25(1):195–204. https://doi.org/10.1007/s00198-013-2505-4
Gong HS, Oh WS, Chung MS, Oh JH, Lee YH, Baek GH (2009) Patients with wrist fractures are less likely to be evaluated and managed for osteoporosis. J Bone Joint Surg Am 91(10):2376–2380. https://doi.org/10.2106/JBJS.H.01871
Khan SA, de Geus C, Holroyd B, Russell AS (2001) Osteoporosis follow-up after wrist fractures following minor trauma. Arch Intern Med 161(10):1309–1312. https://doi.org/10.1001/archinte.161.10.1309
Mallmin H, Ljunghall S, Persson I, Naessén T, Krusemo UB, Bergström R (1993) Fracture of the distal forearm as a forecaster of subsequent hip fracture: a population-based cohort study with 24 years of follow-up. Calcif Tissue Int 52(4):269–272. https://doi.org/10.1007/BF00296650
Owen RA, Melton LJ 3rd, Ilstrup DM, Johnson KA, Riggs BL (1982) Colles’ fracture and subsequent hip fracture risk. Clin Orthop Relat Res 171:37–43
Rozental TD, Branas CC, Bozentka DJ, Beredjiklian PK (2002) Survival among elderly patients after fractures of the distal radius. J Hand Surg Am 27(6):948–952. https://doi.org/10.1053/jhsu.2002.36995
Svedbom A, Borgstöm F, Hernlund E, Ström O, Alekna V, Bianchi ML, Clark P, Curiel MD, Dimai HP, Jürisson M, Kallikorm R, Lember M, Lesnyak O, McCloskey E, Sanders KM, Silverman S, Solodovnikov A, Tamulaitiene M, Thomas T, Toroptsova N, Uusküla A, Tosteson ANA, Jönsson B, Kanis JA (2018) Quality of life for up to 18 months after low-energy hip, vertebral, and distal forearm fractures-results from the ICUROS. Osteoporos Int 29(3):557–566. https://doi.org/10.1007/s00198-017-4317-4
Shortt NL, Robinson CM (2005) Mortality after low-energy fractures in patients aged at least 45 years old. J Orthop Trauma 19(6):396–400. https://doi.org/10.1097/01.bot.0000155311.04886.7e
Lipman MD, Hess DE, Werner BC, Deal DN (2019) Fibromyalgia as a predictor of complex regional pain syndrome after distal radius fracture. Hand 14(4):516–522. https://doi.org/10.1177/1558944717735949
Mosenthal WP, Boyajian HH, Ham SA, Conti Mica MA (2019) Treatment trends, complications, and effects of comorbidities on distal radius fractures. Hand 14(4):534–539. https://doi.org/10.1177/1558944717751194
Torchia MT, Munson J, Tosteson TD, Tosteson ANA, Wang Q, McDonough CM, Morgan TS, Bynum JPW, Bell JE (2019) Patterns of opioid use in the 12 months following geriatric fragility fractures: a population-based cohort study. J Am Med Dir Assoc 20(3):298–304. https://doi.org/10.1016/j.jamda.2018.09.024
Johnson NA, Stirling ER, Divall P, Thompson JR, Ullah AS, Dias JJ (2017) Risk of hip fracture following a wrist fracture-a meta-analysis. Injury 48(2):399–405. https://doi.org/10.1016/j.injury.2016.11.002
Bentohami A, de Burlet K, de Korte N, van den Bekerom MP, Goslings JC, Schep NW (2014) Complications following volar locking plate fixation for distal radial fractures: a systematic review. J Hand Surg Eur 39(7):745–754. https://doi.org/10.1177/1753193413511936
Jayakumar P, Teunis T, Vranceanu AM, Lamb S, Ring D, Gwilym S (2020) Early psychological and social factors explain the recovery trajectory after distal radial fracture. J Bone Joint Surg Am 102(9):788–795. https://doi.org/10.2106/JBJS.19.00100
Riley RD, Hayden JA, Steyerberg EW, Moons KG, Abrams K, Kyzas PA, Malats N, Briggs A, Schroter S, Altman DG, Hemingway H, PROGRESS Group (2013) Prognosis Research Strategy (PROGRESS) 2: prognostic factor research. PLoS Med 10(2):e1001380. https://doi.org/10.1371/journal.pmed.1001380
British Orthopaedic Association, British Society for Surgery of the Hand (2018) Best practice for management of distal radial fractures (DRFs). https://www.bssh.ac.uk/_userfiles/pages/files/professionals/Radius/Blue%20Book%20DRF%20Final%20Document.pdf. Accessed 20 Apr 2021
Handoll HH, Elliott J (2015) Rehabilitation for distal radial fractures in adults. Cochrane Database Syst Rev 9:CD003324. https://doi.org/10.1002/14651858.CD003324.pub3
Acknowledgements
Authors acknowledge and are grateful for the contributions of Dr Linda Chesterton, Dr John Edwards and Mrs Victoria Jansen (Senior Hand and Research Physiotherapist, Pulvertaft Hand Centre, Royal Derby Hospital) who contributed to the development and design of this study. We also acknowledge contributions of Mrs Ruth Haines (Patient and Public Involvement and Engagement) in the study design and interpretation of results as part of this study.
Funding
This study is funded by the National Institute for Health Research (NIHR) (PB-PG-0317–10033)/Research for Patient Benefit. ZP is funded by the NIHR, Clinician Scientist Award (ZP—CS-2018–18-ST2-010)/NIHR Academy. CB is funded by an NIHR Clinical Lectureship. The views expressed are those of the author(s) and not necessarily those of the National Health Service, the NIHR or the Department of Health and Social Care.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Babatunde, O.O., Bucknall, M., Burton, C. et al. Long-term clinical and socio-economic outcomes following wrist fracture: a systematic review and meta-analysis. Osteoporos Int 33, 753–782 (2022). https://doi.org/10.1007/s00198-021-06214-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-021-06214-9