Abstract
Summary
Decreased cortical bone density and bone strength at peak height velocity (PHV) were noted in girls with adolescent idiopathic scoliosis (AIS). These findings could provide the link to the previously reported observation that low bone mineral density (BMD) could contribute as one of the prognostic factors for curve progression that mostly occurs during PHV in AIS.
Introduction
As part of the studies related to aetiopathogenesis of AIS, we assessed bone qualities, bone mechanical strength and bone turnover markers (BTMs) focusing at the peri-pubertal period and PHV in AIS girls.
Methods
396 AIS girls in two separate cohorts were studied. Skeletal maturity was assessed using the validated thumb ossification composite index (TOCI). Bone qualities and strength were evaluated with high-resolution peripheral quantitative computed tomography (HR-pQCT) and finite element analysis (FEA).
Results
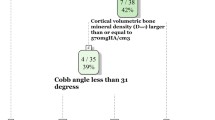
Cohort-A included 179 girls (11.95 ± 0.95 years old). Girls at TOCI-4 had numerically the highest height velocity (0.71 ± 0.24 cm/month) corresponding to the PHV. Subjects at TOCI-4 had lower cortical volumetric BMD (672.36 ± 39.07 mg/mm3), cortical thickness (0.68 ± 0.08 mm) and apparent modulus (1601.54 ± 243.75 N/mm2) than: (a) those at TOCI-1–3 (724.99 ± 32.09 mg/mm3 (p < 0.001), 0.79 ± 0.11 mm (p < 0.001) and 1910.88 ± 374.75 N/mm2 (p < 0.001), respectively) and (b) those at TOCI-8 (732.28 ± 53.75 mg/mm3 (p < 0.001), 0.84 ± 0.14 mm (p < 0.001), 1889.11 ± 419.37 N/mm2 (p < 0.001), respectively). Cohort-B included 217 girls (12.22 ± 0.89 years old). Subjects at TOCI-4 had higher levels of C-terminal telopeptide of type 1 collagen (1524.70 ± 271.10 pg/L) and procollagen type 1 N-terminal propeptide (941.12 ± 161.39 µg/L) than those at TOCI-8 (845.71 ± 478.55 pg/L (p < 0.001) and 370.08 ± 197.04 µg/L (p < 0.001), respectively).
Conclusion
AIS girls had decreased cortical bone density and bone mechanical strength with elevated BTMs at PHV. Coupling of PHV with decreased cortical and FEA parameters could provide the link to the previously reported observation that low BMD could contribute as one of the prognostic factors for curve progression that mostly occurs during PHV in AIS.




Similar content being viewed by others
Availability of data and material
The data that support the findings of this study are available on reasonable request from the corresponding author.
Code availability
Not applicable.
References
Cheng JC, Castelein RM, Chu WC, Danielsson AJ, Dobbs MB, Grivas TB, Gurnett CA, Luk KD, Moreau A, Newton PO, Stokes IA, Weinstein SL, Burwell RG (2015) Adolescent idiopathic scoliosis. Nat Rev Dis Primers 1:15030. https://doi.org/10.1038/nrdp.2015.30
Asher MA, Burton DC (2006) Adolescent idiopathic scoliosis: natural history and long term treatment effects. Scoliosis 1(1):2. https://doi.org/10.1186/1748-7161-1-2
Cobb JR (1960) The problem of the primary curve. J Bone Joint Surg Am 42-A(8):1413–1425
Negrini S, Donzelli S, Aulisa AG, Czaprowski D, Schreiber S, de Mauroy JC, Diers H, Grivas TB, Knott P, Kotwicki T, Lebel A, Marti C, Maruyama T, O’Brien J, Price N, Parent E, Rigo M, Romano M, Stikeleather L, Wynne J, Zaina F (2018) 2016 SOSORT guidelines: orthopaedic and rehabilitation treatment of idiopathic scoliosis during growth. Scoliosis Spinal Disord 13(1):3. https://doi.org/10.1186/s13013-017-0145-8
Moskowitz A, Moe JH, Winter RB, Binner H (1980) Long-term follow-up of scoliosis fusion. J Bone Joint Surg Am 62(3):364–376
Coe JD, Arlet V, Donaldson W, Berven S, Hanson DS, Mudiyam R, Perra JH, Shaffrey CI (2006) Complications in spinal fusion for adolescent idiopathic scoliosis in the new millennium. A report of the Scoliosis Research Society Morbidity and Mortality Committee. Spine (Phila PA 1976) 31(3):345–349. https://doi.org/10.1097/01.brs.0000197188.76369.13
Cheung CS, Lee WT, Tse YK, Lee KM, Guo X, Qin L, Cheng JC (2006) Generalized osteopenia in adolescent idiopathic scoliosis–association with abnormal pubertal growth, bone turnover, and calcium intake? Spine (Phila PA 1976) 31(3):330–338. https://doi.org/10.1097/01.brs.0000197410.92525.10
Yu WS, Chan KY, Yu FW, Ng BK, Lee KM, Qin L, Lam TP, Cheng JC (2014) Bone structural and mechanical indices in adolescent idiopathic scoliosis evaluated by high-resolution peripheral quantitative computed tomography (HR-pQCT). Bone 61:109–115. https://doi.org/10.1016/j.bone.2013.12.033
Li X, Hung VWY, Yu FWP, Hung ALH, Ng BKW, Cheng JCY, Lam TP, Yip BHK (2020) Persistent low-normal bone mineral density in adolescent idiopathic scoliosis with different curve severity: a longitudinal study from presentation to beyond skeletal maturity and peak bone mass. Bone 133:115217. https://doi.org/10.1016/j.bone.2019.115217
Cheng JC, Hung VW, Lee WT, Yeung HY, Lam TP, Ng BK, Guo X, Qin L (2006) Persistent osteopenia in adolescent idiopathic scoliosis–longitudinal monitoring of bone mineral density until skeletal maturity. Stud Health Technol Inform 123:47–51
Yip BHK, Yu FWP, Wang Z, Hung VWY, Lam TP, Ng BKW, Zhu F, Cheng JCY (2016) Prognostic value of bone mineral density on curve progression: a longitudinal cohort study of 513 girls with adolescent idiopathic scoliosis. Sci Rep 6:39220. https://doi.org/10.1038/srep39220
Lam TP, Hung VW, Yeung HY, Chu WC, Ng BK, Lee KM, Qin L, Cheng JC (2013) Quantitative ultrasound for predicting curve progression in adolescent idiopathic scoliosis: a prospective cohort study of 294 cases followed-up beyond skeletal maturity. Ultrasound Med Biol 39(3):381–387. https://doi.org/10.1016/j.ultrasmedbio.2012.09.012
Hung VW, Qin L, Cheung CS, Lam TP, Ng BK, Tse YK, Guo X, Lee KM, Cheng JC (2005) Osteopenia: a new prognostic factor of curve progression in adolescent idiopathic scoliosis. J Bone Joint Surg 87(12):2709–2716
McCormack SE, Cousminer DL, Chesi A, Mitchell JA, Roy SM, Kalkwarf HJ, Lappe JM, Gilsanz V, Oberfield SE, Shepherd JA, Winer KK, Kelly A, Grant SFA, Zemel BS (2017) Association between linear growth and bone accrual in a diverse cohort of children and adolescents. JAMA Pediatr 171(9):e171769. https://doi.org/10.1001/jamapediatrics.2017.1769
Magarey AM, Boulton TJ, Chatterton BE, Schultz C, Nordin BE, Cockington RA (1999) Bone growth from 11 to 17 years: relationship to growth, gender and changes with pubertal status including timing of menarche. Acta Paediatr 88(2):139–146. https://doi.org/10.1080/08035259950170286
Zhu K, Greenfield H, Zhang Q, Du X, Ma G, Foo LH, Cowell CT, Fraser DR (2008) Growth and bone mineral accretion during puberty in Chinese girls: a five-year longitudinal study. J Bone Miner Res 23(2):167–172. https://doi.org/10.1359/jbmr.071006
Faulkner RA, Davison KS, Bailey DA, Mirwald RL, Baxter-Jones AD (2006) Size-corrected BMD decreases during peak linear growth: implications for fracture incidence during adolescence. J Bone Miner Res 21(12):1864–1870. https://doi.org/10.1359/jbmr.060907
Gabel L, Macdonald HM, McKay HA (2017) Sex differences and growth-related adaptations in bone microarchitecture, geometry, density, and strength from childhood to early adulthood: a mixed longitudinal HR-pQCT study. J Bone Miner Res 32(2):250–263. https://doi.org/10.1002/jbmr.2982
Gabel L, Nettlefold L, Brasher PM, Moore SA, Ahamed Y, Macdonald HM, McKay HA (2015) Reexamining the surfaces of bone in boys and girls during adolescent growth: a 12-year mixed longitudinal pQCT study. J Bone Miner Res 30(12):2158–2167. https://doi.org/10.1002/jbmr.2570
Kirmani S, Christen D, van Lenthe GH, Fischer PR, Bouxsein ML, McCready LK, Melton LJ 3rd, Riggs BL, Amin S, Muller R, Khosla S (2009) Bone structure at the distal radius during adolescent growth. J Bone Miner Res 24(6):1033–1042. https://doi.org/10.1359/jbmr.081255
Mitchell DM, Caksa S, Yuan A, Bouxsein ML, Misra M, Burnett-Bowie SM (2018) Trabecular bone morphology correlates with skeletal maturity and body composition in healthy adolescent girls. J Clin Endocrinol Metab 103(1):336–345. https://doi.org/10.1210/jc.2017-01785
Wang Q, Wang XF, Iuliano-Burns S, Ghasem-Zadeh A, Zebaze R, Seeman E (2010) Rapid growth produces transient cortical weakness: a risk factor for metaphyseal fractures during puberty. J Bone Miner Res 25(7):1521–1526. https://doi.org/10.1002/jbmr.46
Cheuk KY, Wang XF, Wang J, Zhang Z, Yu FWP, Tam EMS, Hung VWY, Lee WYW, Ghasem-Zadeh A, Zebaze R, Zhu TY, Guo XE, Cheng JCY, Lam TP, Seeman E (2018) Sexual dimorphism in cortical and trabecular bone microstructure appears during puberty in Chinese children. J Bone Miner Res 33(11):1948–1955. https://doi.org/10.1002/jbmr.3551
Jaworski M, Graff K (2018) Peripheral quantitative computed tomography of the distal and proximal forearm in children and adolescents: bone densities, cross-sectional sizes and soft tissues reference data. J Musculoskelet Neuronal Interact 18(2):237–247
Wang Q, Alen M, Nicholson P, Lyytikainen A, Suuriniemi M, Helkala E, Suominen H, Cheng S (2005) Growth patterns at distal radius and tibial shaft in pubertal girls: a 2-year longitudinal study. J Bone Miner Res 20(6):954–961. https://doi.org/10.1359/JBMR.050110
Zhang J, Wang Y, Cheng KL, Cheuk K, Lam TP, Hung ALH, Cheng JCY, Qiu Y, Muller R, Christen P, Lee WYW (2021) Association of higher bone turnover with risk of curve progression in adolescent idiopathic scoliosis. Bone 143:115655. https://doi.org/10.1016/j.bone.2020.115655
Emmanuel M, Bokor BR (2020) Tanner stages. In: StatPearls. Treasure Island (FL)
Hung ALH, Chau WW, Shi B, Chow SK, Yu FYP, Lam TP, Ng BKW, Qiu Y, Cheng JCY (2017) Thumb ossification composite index (TOCI) for predicting peripubertal skeletal maturity and peak height velocity in idiopathic scoliosis: a validation study of premenarchal girls with adolescent idiopathic scoliosis followed longitudinally until skeletal maturity. J Bone Joint Surg Am 99(17):1438–1446. https://doi.org/10.2106/JBJS.16.01078
Hung AL, Shi B, Chow SK, Chau WW, Hung VW, Wong RM, Liu KL, Lam TP, Ng BK, Cheng JC (2018) Validation study of the thumb ossification composite index (TOCI) in idiopathic scoliosis: a stage-to-stage correlation with classic Tanner-Whitehouse and Sanders simplified skeletal maturity systems. J Bone Joint Surg Am 100(13):88. https://doi.org/10.2106/JBJS.17.01271
Pols MA, Peeters PH, Bueno-De-Mesquita HB, Ocke MC, Wentink CA, Kemper HC, Collette HJ (1995) Validity and repeatability of a modified Baecke questionnaire on physical activity. Int J Epidemiol 24(2):381–388. https://doi.org/10.1093/ije/24.2.381
Woo JLS, Ho SC, Lam TH, Janus ED (1997) A food frequency questionnaire for use in the Chinese population in Hong Kong: description and examination of validity. Nutr Res 17:1633–1641
Whittier DE, Boyd SK, Burghardt AJ, Paccou J, Ghasem-Zadeh A, Chapurlat R, Engelke K, Bouxsein ML (2020) Guidelines for the assessment of bone density and microarchitecture in vivo using high-resolution peripheral quantitative computed tomography. Osteoporos Int 31(9):1607–1627. https://doi.org/10.1007/s00198-020-05438-5
Cheng JC, Tang SP, Guo X, Chan CW, Qin L (2001) Osteopenia in adolescent idiopathic scoliosis: a histomorphometric study. Spine (Phila Pa 1976) 26(3):E19-23. https://doi.org/10.1097/00007632-200102010-00002
Cheung TF, Cheuk KY, Yu FW, Hung VW, Ho CS, Zhu TY, Ng BK, Lee KM, Qin L, Ho SS, Wong GW, Cheng JC, Lam TP (2016) Prevalence of vitamin D insufficiency among adolescents and its correlation with bone parameters using high-resolution peripheral quantitative computed tomography. Osteoporos Int 27(8):2477–2488. https://doi.org/10.1007/s00198-016-3552-4
Yang G, Lee WYW, Hung ALH, Tang MF, Li X, Kong APS, Leung TF, Yung PSH, To KKW, Cheng JCY, Lam TP (2021) Association of serum 25(OH)Vit-D levels with risk of pediatric fractures: a systematic review and meta-analysis. Osteoporos Int. https://doi.org/10.1007/s00198-020-05814-1
Yim AP, Yeung HY, Hung VW, Lee KM, Lam TP, Ng BK, Qiu Y, Cheng JC (2012) Abnormal skeletal growth patterns in adolescent idiopathic scoliosis–a longitudinal study until skeletal maturity. Spine (Phila Pa 1976) 37(18):E1148-1154. https://doi.org/10.1097/BRS.0b013e31825c036d
Nissinen M, Heliovaara M, Seitsamo J, Poussa M (1993) Trunk asymmetry, posture, growth, and risk of scoliosis. A three-year follow-up of Finnish prepubertal school children. Spine (Phila Pa 1976) 18(1):8–13. https://doi.org/10.1097/00007632-199301000-00002
Loncar-Dusek M, Pecina M, Prebeg Z (1991) A longitudinal study of growth velocity and development of secondary gender characteristics versus onset of idiopathic scoliosis. Clin Orthop Relat Res 270:278–282
Frisancho AR, Garn SM, Ascoli W (1970) Subperiosteal and endosteal bone apposition during adolescence. Hum Biol 42(4):639–664
Seeman E (2003) Periosteal bone formation–a neglected determinant of bone strength. N Engl J Med 349(4):320–323. https://doi.org/10.1056/NEJMp038101
Bala Y, Zebaze R, Seeman E (2015) Role of cortical bone in bone fragility. Curr Opin Rheumatol 27(4):406–413. https://doi.org/10.1097/BOR.0000000000000183
Eastell R, Pigott T, Gossiel F, Naylor KE, Walsh JS, Peel NFA (2018) Diagnosis of endocrine disease: bone turnover markers: are they clinically useful? Eur J Endocrinol 178(1):R19–R31. https://doi.org/10.1530/EJE-17-0585
Jurimae J (2010) Interpretation and application of bone turnover markers in children and adolescents. Curr Opin Pediatr 22(4):494–500. https://doi.org/10.1097/MOP.0b013e32833b0b9e
Sanders JO, Browne RH, McConnell SJ, Margraf SA, Cooney TE, Finegold DN (2007) Maturity assessment and curve progression in girls with idiopathic scoliosis. J Bone Joint Surg Am 89(1):64–73. https://doi.org/10.2106/JBJS.F.00067
Campisi SC, Marchand JD, Siddiqui FJ, Islam M, Bhutta ZA, Palmert MR (2020) Can we rely on adolescents to self-assess puberty stage? A systematic review and meta-analysis. J Clin Endocrinol Metab 105(8):2846–2856. https://doi.org/10.1210/clinem/dgaa135
Funding
This study was supported by General Research Fund of Research Grants Council of the Hong Kong SAR, China (Project 14130216, 14174517, 14163517 and 14120818) and the Health and Medical Research Fund (Project 06170546).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethic approval
This study was approved by the joint CUHK-NTEC Clinical Research Ethics Committee (reference number: 2017.038-T and 2009.491-T). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the Helsinki declaration.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent to publication
Not applicable.
Conflict of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Yang, K.G., Lee, W.Y., Hung, A.L. et al. Decreased cortical bone density and mechanical strength with associated elevated bone turnover markers at peri-pubertal peak height velocity: a cross-sectional and longitudinal cohort study of 396 girls with adolescent idiopathic scoliosis. Osteoporos Int 33, 725–735 (2022). https://doi.org/10.1007/s00198-021-06200-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-021-06200-1