Abstract
Summary
Methodological limitations preclude determination of the association between sleep duration and bone mineral density (BMD) from existing literature. This was the first study to use objective sleep duration to determine its association with BMD. Nocturnal sleep duration, assessed objectively (actigraphy) or subjectively (questionnaire), was not independently associated with BMD in postmenopausal women.
Introduction
Both long and short self-reported sleep durations are associated with low bone mineral density (BMD) in men and women. The association between sleep duration measured by actigraphy and BMD in postmenopausal women is unknown.
Methods
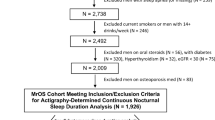
The Study of Osteoporotic Fractures (SOF) ancillary sleep study was used to determine the association between sleep duration and BMD at the total hip and femoral neck in postmenopausal women ≥ 75 years old. Sleep duration was assessed by wrist actigraphy (average 4 nights) and questionnaire. BMD was compared between postmenopausal women with short (< 6 h/night) vs. NIH-recommended (7–8 h/night) sleep durations. Data were analyzed using a 2-sample t test (unadjusted) and multivariate regression model (adjusted). Simple linear regression was used to estimate the difference in BMD per additional hour of sleep when sleep duration was considered as a continuous, rather than dichotomized, variable.
Results
Total hip BMD was higher in women with actigraphically assessed shorter sleep duration in unadjusted models only. No clinically or statistically significant differences in total hip or femoral neck BMD were observed according to nocturnal sleep duration after adjusting for body mass index (BMI) in dichotomized (N = 874) or continuous (N = 1624) sleep duration models or when subjective sleep duration was used. When sleep duration included daytime naps, longer sleep duration was associated with lower total hip BMD (β = − 0.005, p = 0.04).
Conclusions
Nocturnal sleep duration, whether assessed objectively (actigraphy) or subjectively (questionnaire), was not independently associated with BMD in older postmenopausal women.

Similar content being viewed by others
Abbreviations
- BMD:
-
Bone mineral density
- P1NP:
-
Propeptide of type 1 procollagen N-terminal
- CTX:
-
C-telopeptide of type I collagen
- AASM:
-
American Academy of Sleep Medicine
- SRS:
-
Sleep Research Society
- SOF:
-
Study of Osteoporotic Fractures
- QUS:
-
Quantitative ultrasound
- DXA:
-
Dual-energy X-ray absorptiometry
- BMI:
-
Body mass index
- PIM:
-
Proportional integration mode
- h:
-
hour
References
(NOF) NOF About NOF. https://www.nof.org/about-us/about-nof/ Accessed July 9 2018
Hudec SM, Camacho PM (2013) Secondary causes of osteoporosis. Endocr Pract 19:120–128
Diab DL, Watts NB (2013) Secondary osteoporosis: differential diagnosis and workup. Clin Obstet Gynecol 56:686–693
Painter SE, Kleerekoper M, Camacho PM (2006) Secondary osteoporosis: a review of the recent evidence. Endocr Pract 12:436–445
Swanson CM, Shea SA, Stone KL, Cauley JA, Rosen CJ, Redline S, Karsenty G, Orwoll ES (2015) Obstructive sleep apnea and metabolic bone disease: insights into the relationship between bone and sleep. J Bone Miner Res 30:199–211
Swanson CM, Kohrt WM, Buxton OM, Everson CA, Wright KP Jr, Orwoll ES, Shea SA (2018) The importance of the circadian system & sleep for bone health. Metabolism 84:28–43
Feskanich D, Hankinson SE, Schernhammer ES (2009) Nightshift work and fracture risk: the Nurses’ Health Study. Osteoporos Int 20:537–542
Cauley JA, Hovey KM, Stone KL, et al. (2018) Characteristics of self-reported sleep and the risk of falls and fractures: the Women’s Health Initiative (WHI). J Bone Miner Res 34:464–474. https://doi.org/10.1002/jbmr.3619
Everson CA, Folley AE, Toth JM (2012) Chronically inadequate sleep results in abnormal bone formation and abnormal bone marrow in rats. Exp Biol Med 237:1101–1109
Xu X, Wang L, Chen L, Su T, Zhang Y, Wang T, Ma W, Yang F, Zhai W, Xie Y, Li D, Chen Q, Fu X, Ma Y, Zhang Y (2016) Effects of chronic sleep deprivation on bone mass and bone metabolism in rats. J Orthop Surg Res 11:87
Swanson C, Shea SA, Wolfe P, Cain SW, Munch M, Vujovic N, Czeisler CA, Buxton OM, Orwoll ES (2017) Bone turnover markers after sleep restriction and circadian disruption: a mechanism for sleep-related bone loss in humans. J Clin Endocrinol Metab 102:3722–3730
Niu J, Sahni S, Liao S, Tucker KL, Dawson-Hughes B, Gao X (2015) Association between sleep duration, insomnia symptoms and bone mineral density in older Boston Puerto Rican adults. PLoS One 10:e0132342
Tian Y, Shen L, Wu J, Xu G, Yang S, Song L, Zhang Y, Mandiwa C, Yang H, Liang Y, Wang Y (2015) Sleep duration and timing in relation to osteoporosis in an elderly Chinese population: a cross-sectional analysis in the Dongfeng-Tongji cohort study. Osteoporos Int 26:2641–2648
Chen G, Chen L, Wen J, Yao J, Li L, Lin L, Tang K, Huang H, Liang J, Lin W, Chen H, Li M, Gong X, Peng S, Lu J, Bi Y, Ning G (2014) Associations between sleep duration, daytime nap duration, and osteoporosis vary by sex, menopause, and sleep quality. J Clin Endocrinol Metab 99:2869–2877
Wang K, Wu Y, Yang Y, Chen J, Zhang D, Hu Y, Liu Z, Xu J, Shen Q, Zhang N, Mao X, Liu C (2015) The associations of bedtime, nocturnal, and daytime sleep duration with bone mineral density in pre- and post-menopausal women. Endocrine 49:538–548
Cunningham TD, Di Pace BS (2015) Is self-reported sleep duration associated with osteoporosis? Data from a 4-year aggregated analysis from the National Health and Nutrition Examination Survey. J Am Geriatr Soc 63:1401–1406
Moradi S, Shab-Bidar S, Alizadeh S, Djafarian K (2017) Association between sleep duration and osteoporosis risk in middle-aged and elderly women: a systematic review and meta-analysis of observational studies. Metabolism 69:199–206
Kim N, Choi HR, Kim SW, Kim BS, Won CW, Kim SY (2014) Association between bone mineral density and sleep duration in the Korean elderly population. Korean J Fam Med 35:90–97
Saint Martin M, Labeix P, Garet M, Thomas T, Barthelemy JC, Collet P, Roche F, Sforza E (2016) Does subjective sleep affect bone mineral density in older people with minimal health disorders? The PROOF cohort. J Clin Sleep Med 12:1461–1469
Wang D, Ruan W, Peng Y, Li W (2018) Sleep duration and the risk of osteoporosis among middle-aged and elderly adults: a dose-response meta-analysis. Osteoporos Int 29:1689–1695
Specker BL, Binkley T, Vukovich M, Beare T (2007) Volumetric bone mineral density and bone size in sleep-deprived individuals. Osteoporos Int 18:93–99
Fu X, Zhao X, Lu H, Jiang F, Ma X, Zhu S (2011) Association between sleep duration and bone mineral density in Chinese women. Bone 49:1062–1066
Kuriyama N, Inaba M, Ozaki E, Yoneda Y, Matsui D, Hashiguchi K, Koyama T, Iwai K, Watanabe I, Tanaka R, Omichi C, Mizuno S, Kurokawa M, Horii M, Niwa F, Iwasa K, Yamada S, Watanabe Y (2017) Association between loss of bone mass due to short sleep and leptin-sympathetic nervous system activity. Arch Gerontol Geriatr 70:201–208
Marques EA, Figueiredo P, Gudnason V, Lang T, Sigurdsson G, Sigurdsson S, Aspelund T, Siggeirsdottir K, Launer L, Eiriksdottir G, Harris TB (2017) Associations of 24-hour sleep duration and CT-derived measurements of muscle and bone: the AGES-Reykjavik study. Exp Gerontol 93:1–6
Lucassen EA, de Mutsert R, le Cessie S, Appelman-Dijkstra NM, Rosendaal FR, van Heemst D, de n Heijer M, Biermasz NR, group NEOs (2017) Poor sleep quality and later sleep timing are risk factors for osteopenia and sarcopenia in middle-aged men and women: the NEO study. PLoS One 12:e0176685
Kobayashi D, Takahashi O, Deshpande GA, Shimbo T, Fukui T (2012) Association between osteoporosis and sleep duration in healthy middle-aged and elderly adults: a large-scale, cross-sectional study in Japan. Sleep Breath 16:579–583
Lima MG, Bergamo Francisco PM, de Azevedo Barros MB (2012) Sleep duration pattern and chronic diseases in Brazilian adults (ISACAMP, 2008/09). Sleep Med 13:139–144
Means MK, Edinger JD, Glenn DM, Fins AI (2003) Accuracy of sleep perceptions among insomnia sufferers and normal sleepers. Sleep Med 4:285–296
Bianchi MT, Wang W, Klerman EB (2012) Sleep misperception in healthy adults: implications for insomnia diagnosis. J Clin Sleep Med 8:547–554
Kushida CA, Chang A, Gadkary C, Guilleminault C, Carrillo O, Dement WC (2001) Comparison of actigraphic, polysomnographic, and subjective assessment of sleep parameters in sleep-disordered patients. Sleep Med 2:389–396
(2012) Explore sleep deprivation and deficiency: how much sleep is enough? National Heart, Lung, and Blood Institute. http://www.nhlbi.nih.gov/health/health-topics/topics/sdd/howmuch
Watson NF, Badr MS, Belenky G et al (2015) Recommended amount of sleep for a healthy adult: a joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society. Sleep 38:843–844
Liu Y, Wheaton AG, Chapman DP, Cunningham TJ, Lu H, Croft JB (2016) Prevalence of healthy sleep duration among adults - United States, 2014. MMWR Morb Mortal Wkly Rep 65:137–141
Centers for Disease C (2014) Insufficient sleep is a public health epidemic. http://www.cdc.gov/features/dssleep/index.html#References
Cummings SR, Black DM, Nevitt MC et al (1990) Appendicular bone density and age predict hip fracture in women. The study of osteoporotic fractures research group. Jama 263:665–668
Blackwell T, Ancoli-Israel S, Gehrman PR, Schneider JL, Pedula KL, Stone KL (2005) Actigraphy scoring reliability in the study of osteoporotic fractures. Sleep 28:1599–1605
Spira AP, Stone KL, Redline S, Ensrud KE, Ancoli-Israel S, Cauley JA, Yaffe K (2017) Actigraphic sleep duration and fragmentation in older women: associations with performance across cognitive domains. Sleep 40
Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ (1989) The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 28:193–213
Johns MW (2000) Sensitivity and specificity of the multiple sleep latency test (MSLT), the maintenance of wakefulness test and the epworth sleepiness scale: failure of the MSLT as a gold standard. J Sleep Res 9:5–11
Liberman UA, Weiss SR, Broll J, Minne HW, Quan H, Bell NH, Rodriguez-Portales J, Downs RW Jr, Dequeker J, Favus M (1995) Effect of oral alendronate on bone mineral density and the incidence of fractures in postmenopausal osteoporosis. The Alendronate Phase III Osteoporosis Treatment Study Group. N Engl J Med 333:1437–1443
Siris ES, Miller PD, Barrett-Connor E, Faulkner KG, Wehren LE, Abbott TA, Berger ML, Santora AC, Sherwood LM (2001) Identification and fracture outcomes of undiagnosed low bone mineral density in postmenopausal women: results from the National Osteoporosis Risk Assessment. Jama 286:2815–2822
Stone KL, Ewing SK, Lui LY, Ensrud KE, Ancoli-Israel S, Bauer DC, Cauley JA, Hillier TA, Cummings SR (2006) Self-reported sleep and nap habits and risk of falls and fractures in older women: the study of osteoporotic fractures. J Am Geriatr Soc 54:1177–1183
Ancoli-Israel S, Kripke DF, Klauber MR, Mason WJ, Fell R, Kaplan O (1991) Sleep-disordered breathing in community-dwelling elderly. Sleep 14:486–495
Tamaki M, Bang JW, Watanabe T, Sasaki Y (2016) Night watch in one brain hemisphere during sleep associated with the first-night effect in humans. Curr Biol 26:1190–1194
Acknowledgments
The authors thank Lily Lui for her assistance with this analysis. In addition, the authors thank the Investigators in the Study of Osteoporotic Fractures Research Group: San Francisco Coordinating Center (California Pacific Medical Center Research Institute and University of California San Francisco): SR Cummings (co-principal investigator), K Yaffe (co-principal investigator), DC Bauer (co-investigator), DM Black (co-investigator), PM Cawthon (co-investigator), N Lane (co-investigator), C McCulloch (co-investigator), A Schwartz (co-investigator), G Tranah (co-investigator), D Evans (co-investigator), R Benard, T Blackwell, L Concepcion, S Ewing, SL Harrison, D Kriesel, N Parimi, K Peters, C Schambach, and J Ziarno.
Funding
CMS is supported by NIH grant T32DK007674-20, NIH grant T32DK007446-34, and 1K23AR070275-01.
The Study of Osteoporotic Fractures (SOF) is supported by the National Institutes of Health funding. The National Institute on Aging (NIA) provides support under the following grant numbers: R01 AG005407, R01 AR35582, R01 AR35583, R01 AR35584, R01 AG005394, R01 AG027574, R01 AG027576, and R01 AG026720.
The research reported in this publication was supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases of the National Institutes of Health under Award Number 1K23AR070275-01, P50 HD073063 (Kohrt), and the Eastern Colorado VA Geriatric, Research, Education, and Clinical Center (GRECC). The contents do not represent the views of the U.S. Department of Veterans Affairs or the United States Government. This research is also supported by NIH/NCATS Colorado CTSA Grant Number UL1 TR002535. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
The Institutional Review Board at each SOF clinical site approved the study, and all participants provided written consent.
Conflict of interest
In the interest of full disclosure, we report the following; however, we do not believe any of these pertain to the current work. PJB, JAC, HAF, MEW, WMK have nothing to disclose. CMS did consulting for Radius Health, Inc. ESL was PI on an unrelated Merck, Inc. grant given to her institution. This funding does not reflect a conflict of interest. KPW reports research support from the NIH, Office of Naval Research, Pac-12, Philips Inc., CurAegis Technologies (formerly known as Torvec Inc.), Somalogics; Financial relationships: consulting fees from or served as a paid member of scientific advisory boards for NIH (Sleep Disorders Research Advisory Board - National Heart, Lung and Blood Institute), CurAegis Technologies, Circadian Therapeutics, LTD, Kellogg Company; Board of Directors: Sleep Research Society; Speaker/educational consultant honorarium fees: American Academy of Sleep Medicine, American College of Chest Physicians, American Diabetes Association. ESO consults for and has received research support from Radius, Mereo, and Bayer. ESO, for The Osteoporotic Fractures in Men (MrOS) Study, is supported by the National Institutes of Health funding via the following institutes: the National Institute on Aging (NIA), the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS), the National Center for Advancing Translational Sciences (NCATS), and NIH Roadmap for Medical Research, under the following grant numbers: U01AG027810, U01 AG042124, U01 AG042139, U01 AG042140,U01 AG042143, U01 AG042145, U01 AG042168, U01AR066160, and UL1 TR000128. KLS has received grant funding from Merck.
Ethical approval
The current analysis utilized de-identified data and was deemed non-human subjects research by the Colorado Multiple Institutional Review Board.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Swanson, C., Blatchford, P., Orwoll, E. et al. Association between objective sleep duration and bone mineral density in older postmenopausal women from the Study of Osteoporotic Fractures (SOF). Osteoporos Int 30, 2087–2098 (2019). https://doi.org/10.1007/s00198-019-05007-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-019-05007-5