Abstract
Summary
The Osteoporosis Self Efficacy Scale was determined to equivalently measure calcium and exercise beliefs in both sexes. Despite data illustrating men’s and women’s similar self-efficacy, gender differences in clinical predictors of self-efficacy imply that efforts to improve care must account for more than self-efficacy.
Introduction
To understand the extent to which the Osteoporosis Self Efficacy (OSE) Scale is reliable for both men and women. A secondary objective was to evaluate sex differences in OSE.
Methods
For this cross-sectional study, we analyzed data collected as part of the Patient Activation after DXA Result Notification (PAADRN) pragmatic trial which enrolled 7749 community-residing adults aged 50 and older reporting for bone densitometry. We used univariable methods, item analysis, exploratory and confirmatory factor analyses, and linear regression to evaluate sex differences in OSE responses and measurement.
Results
In this sample, the confirmatory factor analysis model for OSE both overall and within groups indicated a poor fit. The sex differences in the measurement model, however, were minor and reflected configural invariance (i.e., constructs were measuring the same things in both men and women), confirming that the OSE was measuring the same constructs in men and women. Men overall had higher exercise self-efficacy and women higher calcium self-efficacy. Overall, education, hip fracture, and self-reported health status predicted exercise self-efficacy whereas prior DXA, self-reported osteoporosis, and history of pharmacotherapy use did not. Predictors of calcium self-efficacy differed by gender.
Conclusion
The OSE can be used to measure calcium and exercise self-efficacy in all older adults. However, gender differences in clinical predictors of self-efficacy and the lack of an association of prior DXA with self-efficacy imply that interventions to improve self-efficacy may be insufficient to drive significant improvement in rates of osteoporosis evaluation and treatment.
Trial registration
Patient Activation after DXA Result Notification (PAADRN), NCT01507662, https://clinicaltrials.gov/ct2/show/NCT01507662
Similar content being viewed by others
References
Kosma M, Cardinal BJ (2016) The transtheoretical model, physical activity, and falls risks among diverse older adults. Act Adapt Aging 40(1):35–52. https://doi.org/10.1080/01924788.2016.1127051
Keller C, Fleur J, Gregor-Holt N, Terris Thompson T (1999) Predictive ability of social cognitive theory in exercise research: an integrated literature review. Online J Knowl Synth Nurs 6(2). https://doi.org/10.1111/j.1524475X.1999.00019.x
Ruthig JC (2016) Health risk perceptions and exercise in older adulthood: an application of protection motivation theory. J Appl Gerontol 35(9):939–959. https://doi.org/10.1177/0733464814544214
Zhu SJ, Nahm ES, Resnick B, Friedmann E, Brown C, Park J et al (2017) The moderated mediating effect of self-efficacy on exercise among older adults in an online bone health intervention study: a parallel process latent growth curve model. J Aging Phys Act 25(3):378–386. https://doi.org/10.1123/japa.2016-0216
Wright NC, Looker AC, Saag KG, Curtis JR, Delzell ES, Randall S, Dawson-Hughes B (2014) The recent prevalence of osteoporosis and low bone mass in the United States based on bone mineral density at the femoral neck or lumbar spine. J Bone Miner Res 29(11):2520–2526
Singer A, Exuzides A, Spangler L, O’Malley C, Colby C, Johnston K, Agodoa I, Baker J, Kagan R (2015) Burden of illness for osteoporotic fractures compared with other serious diseases among postmenopausal women in the United States. Mayo Clin Proc 90(1):53–62
Office of Inspector General (2010) Healthcare inspection: management of osteoporosis in veterans with fractures. (09-03138-191). Washington, DC
King AB, Fiorentino DM (2011) Medicare payment cuts for osteoporosis testing reduced use despite tests’ benefit in reducing fractures. Health Aff (Millwood) 30(12):2362–2370. https://doi.org/10.1377/hlthaff.2011.0233
O’Malley CD, Johnston SS, Lenhart G, Cherkowski G, Palmer L, Morgan SL (2011) Trends in dual-energy X-ray absorptiometry in the United States, 2000–2009. J Clin Densitom 14(2):100–107. https://doi.org/10.1016/j.jocd.2011.03.003
Ali N, Shonk C, El-Sayed M (2009) Bone health in men: influencing factors. Am J Health Behav 33(2):213–222. https://doi.org/10.5993/AJHB.33.2.10
Solimeo SL (2011) Living with a ‘women’s disease’: risk appraisal and management among men with osteoporosis. J Mens Health 8(3):185–191. https://doi.org/10.1016/j.jomh.2011.06.001
Schweser KM, Crist BD (2017) Osteoporosis: a discussion on the past 5 years. Current Reviews in Musculoskeletal Medicine 10(2):265–274. https://doi.org/10.1007/s12178-017-9410-y
Miller PD (2016) Underdiagnoses and undertreatment of osteoporosis: the battle to be won. J Clin Endocrinol Metab 101(3):852–859. https://doi.org/10.1210/jc.2015-3156
Stoecker WV, Carson A, Nguyen VH, Willis AB, Cole JG, Rader RK (2017) Addressing the crisis in the treatment of osteoporosis: better paths forward. J Bone Miner Res 32(6):1386–1387. https://doi.org/10.1002/jbmr.3145
Horan ML, Kim KK, Gendler P, Froman RD, Patel MD (1998) Development and evaluation of the osteoporosis self-efficacy scale. Res Nurs Health 21(5):395–403. https://doi.org/10.1002/(SICI)1098-240X(199810)21:5<395::AID-NUR3>3.0.CO;2-I
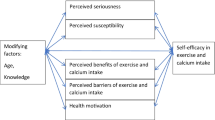
Doheny MO, Sedlak CA, Hall RJ (2010) Structural model for osteoporosis preventing behavior in men. Am J Mens Health 4(4):334–343. https://doi.org/10.1177/1557988309351953
Blankson AN, McArdle JJ (2013) Measurement invariance of cognitive abilities across ethnicity, gender, and time among older Americans. J Gerontol Ser B Psychol Sci Soc Sci 70(3):386–397. https://doi.org/10.1093/geronb/gbt106
Wolinksy FD, Lou Y, Edmonds SW, Hall SF, Jones MP, Wright NC, Saag KG, Cram P, Roblin D, on behalf of the PAADRN Investigatorsa (2017) Activating patients with a tailored bone density test results letter and educational brochure: the PAADRN randomized controlled trial. J Clin Densitom 20(4):464–471. https://doi.org/10.1016/j.jocd.2016.08.012
Edmonds SW, Wolinsky FD, Christensen AJ, Lu X, Jones MP, Roblin DW, Saag KG, Cram P, on behalf of the PAADRN Investigators (2013) The PAADRN study: a design for a randomized controlled practical clinical trial to improve bone health. Contemp Clinc trials 34(1):90–100. https://doi.org/10.1016/j.cct.2012.10.002
Cram P, Wolinsky FD, Lou Y, Edmonds SW, Hall SF, Roblin DW, Wright NC, Jones MP, Saag KG, on behalf of the PAADRN Investigators (2016) Patient-activation and guideline-concordant pharmacological treatment after bone density testing: the PAADRN randomized controlled trial. Osteoporos Int 27(12):3513–3524. https://doi.org/10.1007/s00198-016-3681-9
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG (2009) Research electronic data capture (REDCap) – a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 42(2):377–381
Kim K, Horan M, Gendler P (1991) Osteoporosis knowledge test, osteoporosis health belief scale, and osteoporosis self-efficacy scale. Allendale, MI
van Buuren S (2007) Multiple imputation of discrete and continuous data by fully conditional specification. Stat Methods Med Res 16(3):219–242. https://doi.org/10.1177/0962280206074463
Jöreskog KG (1969) A general approach to confirmatory maximum likelihood factor analysis. Psychometrika 34(2):183–202
Campbell DT, Fiske DW (1959) Convergent and discriminant validation by the multitrait-multimethod matrix. Psychol Bull 56(2):81–105
Lee C, Segal R, Kimberlin C, Smith WT, Weiler RM (2014) Reliability and validity for the measurement of moral disengagement in pharmacists. Res Soc Adm Pharm 10(2):297–312
Abdulameer SA, Syed Sulaiman SA, Hassali MA, Subramaniam K, Sahib MN (2013) Psychometric properties and osteoprotective behaviors among type 2 diabetic patients: osteoporosis self-efficacy scale Malay version (OSES-M). Osteoporos Int 24(3):929–940. https://doi.org/10.1007/s00198-012-2071-1
McLeod KM, Johnson CS (2011) A systematic review of osteoporosis health beliefs in adult men and women. J Osteoporos 2011:197454–197411. https://doi.org/10.4061/2011/197454
Doheny MO, Sedlak CA, Estok PJ, Zeller R (2007) Osteoporosis knowledge, health beliefs, and DXA T-scores in men and women 50 years of age and older. Orthop Nurs 26(4):243–250. https://doi.org/10.1097/01.NOR.0000284654.68215.de
Shawa H, Favela E, Diaz J (2011) Knowledge of osteoporosis among men in the primary care setting. South Med J 104(8):584–588. https://doi.org/10.1097/SMJ.0b013e3182241da1
Malekshahi F, Hidarnia A, Niknami S, Aminshokravi F (2015) The determination of predictive construct of physical behavior change on osteoporosis prevention women aged 30–50: a trans-theoretical method study. Global J Health Sci 8(3):183–193. https://doi.org/10.5539/gjhs.v8n3p183
Gammage KL, Klentrou P (2011) Predicting osteoporosis prevention behaviors: health beliefs and knowledge. Am J Health Behav 35(3):371–382. https://doi.org/10.5993/AJHB.35.3.10
Binkley N (2009) A perspective on male osteoporosis. Best Pract Res Clin Rheumatol 23(6):755–768. https://doi.org/10.1016/j.berh.2009.10.001
Gough B, Conner MT (2006) Barriers to healthy eating amongst men: a qualitative analysis. Soc Sci Med 62:387–395. https://doi.org/10.1016/j.socscimed.2005.05.032
Mahalik JR, Burns SM, Syzdek M (2007) Masculinity and perceived normative health behaviors as predictors of men's health behaviors. Soc Sci Med 64(11):2201–2209. https://doi.org/10.1016/j.socscimed.2007.02.035
Compton M, Mortenson B, Sale J, Crossman A, Ashe MC (2018) Men’s perceptions of living with osteoporosis: a systematic review of qualitative studies. Int J of Orthop Trauma Nurg. https://doi.org/10.1016/j.ijotn.2018.11.007
Acknowledgements
We thank Rebecca Burmeister, MPH (UI), Mollie Giller, MPH (UI), April Miller RT (UI), CBDT, Amna Rizvi-Toner, BA, BS (UI), Kara Wessels, BA (UI), Brandi Robinson (KP), Akeba Mitchell (KP), Aimee Khamar (KP), and Roslin Nelson (KP) and all of the staff at the Iowa Social Science Research Center for recruiting and interviewing all study participants. All except Ms. Miller were compensated from grant funds for their time. We also thank Ryan Outman, MS (UAB), for coordinating and facilitating recruitment of study participants. Finally, we thank the 7749 patients who participated in PAADRN.
Funding
This work was supported by the National Institute on Aging at the United States (U.S.) National Institutes of Health (R01 AG033035 to PC and FDW). SL Solimeo receives support from the Center for Comprehensive Access & Delivery Research and Evaluation (CADRE), Department of Veterans Affairs, Iowa City VA Health Care System, Iowa City, IA (Award no. CIN 13-412), and a VA HSR&D Career Development Award (Award no. CDA 13-272).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
SL Solimeo, VT Nguyen, SW Edmonds, Y Lou, DW Roblin, P Cram, and FD Wolinsky have no conflicts to report. KG Saag has received grants from Amgen, Eli Lilly, and Merck and has served as a paid consultant to Amgen, Eli Lilly, and Merck unrelated to this project.
Disclaimer
The US Department of Health and Human Services, National Institutes of Health’s National Institute on Aging had no role in the analysis or interpretation of data or the decision to report these data in a peer-reviewed journal. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the US government.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Solimeo, S.L., Nguyen, VT.T., Edmonds, S.W. et al. Sex differences in osteoporosis self-efficacy among community-residing older adults presenting for DXA. Osteoporos Int 30, 1033–1041 (2019). https://doi.org/10.1007/s00198-019-04854-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-019-04854-6