Abstract
Summary
A majority of adults with persistently low serum alkaline phosphatase values carry a pathogenic or likely pathogenic variant in the ALPL gene and also have elevated alkaline phosphatase substrate values in serum and urine. These adults may fall within the spectrum of the adult form of hypophosphatasia.
Introduction
The primary objective of this study was to determine what proportion of adults with persistently low serum alkaline phosphatase values (hypophosphatasemia) harbor mutations in the ALPL gene or have elevated alkaline phosphatase (ALP) substrates. Some adults with persistent hypophosphatasemia share clinical and radiographic features with the adult form of hypophosphatasia (HPP). In HPP, ALPL mutations result in persistent hypophosphatasemia and ALP substrate accumulation in plasma (pyridoxal-5-phosphate (PLP)) and urine (phosphoethanolamine (PEA)).
Methods
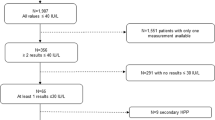
Biochemical analyses, including serum ALP activity, bone-specific ALP, plasma PLP, and urine PEA, were performed in adults with persistent hypophosphatasemia. Mutational analyses were performed using PCR and Sanger sequencing methods. Gene variants were classified as pathogenic (P), likely pathogenic (LP), variants of uncertain significance (VUS), likely benign (LB), and benign (B). P and LP variants were further grouped as “Positive ALPL variants” and LB and B grouped as “Negative ALPL variants.”
Results
Fifty subjects completed all mutational and biochemical analyses. Sixteen percent carried only Negative ALPL variants. Of the remaining 42 subjects, 67% were heterozygous for a P variant, 19% for an LP variant, and 14% for a VUS. Biochemical results were highly inter-correlated and consistent with the expected inverse relationship between ALP and its substrates. Subjects harboring Positive ALPL variants showed lower ALP and BSAP and higher PLP and PEA values compared with subjects harboring only Negative ALPL variants. Approximately half of all subjects harboring Positive ALPL variants or ALPL VUS showed elevations in plasma PLP, and three quarters showed elevations in urine PEA.
Conclusion
Adults with persistent hypophosphatasemia frequently harbor ALPL mutations and have elevated ALP substrates. These adults may fall within the spectrum of the adult form of hypophosphatasia. Clinicians should take note of persistent hypophosphatasemia in their patients and be cautious in prescribing bisphosphonates when present.

Similar content being viewed by others
References
McKiernan FE, Shrestha LK, Berg RL, Fuehrer J (2014) Acute hypophosphatasemia. Osteoporos Int 25:519–523
Ponce A, Peris P, Alvarez L, Muñoz-Gómez J (1996) Benign familial hypophosphatasemia. Rev Clin Esp 196:342
Whyte MP (2017) Hypophosphatasia: an overview for 2017. Bone. doi:10.1016/j.bone.2017.02.011
Mornet E Tissue nonspecific alkaline phosphatase gene mutation database. http://www.sesep.uvsq.fr/03_hypo_mutations.php. Accessed 1 March 2017
Chuck AJ, Pattrick MG, Hamilton E, Wilson R, Doherty M (1989) Crystal deposition in hypophosphatasia: a reappraisal. Ann Rheum Dis 48:571–576
Whyte MP, Murphy WA, Fallon MD (1982) Adult hypophosphatasia with chondrocalcinosis and arthropathy. Variable penetrance of hypophosphatasemia in a large Oklahoma kindred. Am J Med 72:631–641
Guanabens N, Mumm S, Möller I et al (2014) Calcific periarthritis as the only clinical manifestation of hypophosphatasia in middle-aged sisters. J Bone Miner Res 29:929–934
Weinstein RS, Whyte MP (1981) Fifty-year follow-up of hypophosphatasia. Arch Int Med 141:1720–1721
McKiernan FE, Berg RL, Fuehrer J (2014) Clinical and radiographic findings in adults with persistent hypophosphatasemia. J Bone Miner Res 29:1651–1660
Richards S, Aziz N, Bale S, Bick D, Das S, Gastier-Foster J, Grody WW, Hegde M, Lyon E, Spector E, Voelkerding K, Rehm HL, ACMG Laboratory Quality Assurance Committee (2015) Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med 17:405–424
Maman E, Borderie D, Roux C, Briot K (2016) Absence of recognition of low alkaline phosphatase level in a tertiary care hospital. Osteoporos Int 27:1251–1254
Harris H, Robson EB (1959) A genetical study of ethanolamine phosphate excretion in hypophosphatasia. Ann Hum Gen 23:421–441
Nielsen CM, Zmuda JM, Carlos AS, Wagoner WJ, Larson EA, Orwoll ES, Klein RF (2012) Rare coding variants in ALPL are associated with low alkaline phosphatase and low bone mineral density. J Bone Min Res 27:93–103
Riancho-Zarriabietia L, García-Unzueta M, Tenorio JA, Gómez-Gerique JA, Pérez VLR, Heath KE, Lapunzina P, Riancho JA (2016) Clinical, biochemical and genetic spectrum of low alkaline phosphatase levels in adults. Eur J Int Med 29:40–45
Whyte MP et al (2015) Hypophosphatasia: validation and expansion of the clinical nosology for children from 25 years experience with 173 pediatric patients. Bone 75:229–239
Fauvert D, Brun-Heath I, Lia-Baldini AS, Bellazi L, Taillandier A, Serre JL, de Mazancourt P, Mornet E (2009) Mild forms of hypophosphatasia mostly result from dominant negative effects of severe alleles or from compound heterozygosity for severe and moderate alleles. BMC Med Gen 10:51
Berkseth KE, Tebben PJ, Drake MT, Hefferan TE, Jewison DE, Wermers RA (2013) Clinical spectrum of hypophosphatasia diagnosed in adults. Bone 54(1):21–27
Greenspan SL, Emkey RD, Bone HG, Weiss SR, Bell NH, Downs RW, McKeever C, Miller SS, Davidson M, Bolognese MA, Mulloy AL, Heyden N, Wu M, Kaur A, Lombardi A (2002) Significant differential effects of alendronate, estrogen, or combination therapy on the rate of bone loss after discontinuation of treatment of postmenopausal osteoporosis. Ann Intern Med 137:875–883
Sutton RA, Mumm S, Coburn SP, Ericson KL, Whyte MP (2012) “Atypical femur fracture” during bisphosphonate exposure in adult hypophosphatasia. J Bone Miner Res 27:987–994
Maman E, Briot K, Roux C (2016) Atypical femur fracture in a 51-year-old woman. Revealing a hypophosphatasia 83:346–348
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Fergus McKiernan, Juan Dong, Erica Scotty, Richard Berg, Lisa Larson, Pamela Mundt, and Indira Rai have no conflict of interest to declare.
Funding
This study was funded in part by Alexion Pharmaceuticals, Inc Investigator-Sponsored Research Grant No. 100105 provided to Marshfield Clinic.
Rights and permissions
About this article
Cite this article
McKiernan, F.E., Dong, J., Berg, R.L. et al. Mutational and biochemical findings in adults with persistent hypophosphatasemia. Osteoporos Int 28, 2343–2348 (2017). https://doi.org/10.1007/s00198-017-4035-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-017-4035-y