Abstract
Summary
A model-based meta-analysis method was performed to quantitatively analyze the efficacy characteristics of calcium intake in BMD increase among postmenopausal women. We found that age and calcium intake dose were key factors affecting the efficiency and onset of BMD change, and daily 1200 mg calcium was suggested to be a beneficial dosage.
Introduction
This paper aims to quantify the efficacy of calcium intake in preventing bone mineral density (BMD) decrease among postmenopausal women and to investigate the factors that may affect the efficacy.
Methods
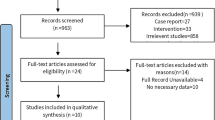
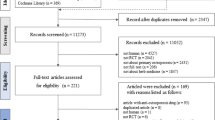
Comprehensive literature search was conducted in PubMed and EMBASE from January 2016. Placebo-controlled or no-treatment controlled randomized trials focused on calcium intake for the management of osteoporosis in postmenopausal women were included. The clinical and demographic characteristics of participants and efficacy data, defined as the mean percentage change of spine BMD (L2–L4) at each observation time point compared with that of baseline, were extracted from the studies. Model-based meta-analysis (MBMA) was used to describe the time course of BMD change by calcium intake and identify the related factors.
Results
This study includes 17 trials involving 2537 subjects. The results showed that a classic pharmacodynamic maximal effect (E max) model could describe the time course of BMD change by calcium intake. Using this model, we found that age and calcium intake dose were key factors affecting the efficiency and onset of BMD change. A 60-year-old woman administered with 800 mg/day calcium can achieve a maximum BMD increasing rate of 2.38%, and the time to reach 50% of this maximum (known as onset time) was 9.44 months. An increase of 0.0817% per year was noted in the maximal effect value for women aged between 50 and 83 years. For calcium dose interval from 250 to 2000 mg/day, the onset time was expressed as 9.44 × (dose/800)−1.33 months. Two-year calcium intake of 700, 1200, and 2000 mg/day resulted in a maximum efficacy of BMD of 68.0, 81.3, and 89.6%, respectively. This indicates that the final efficacy had already reached the plateau (>80% E max) under the 1200-mg/day dose.
Conclusion
Calcium intake can effectively postpone the tendency of BMD decrease in postmenopausal women. An increased calcium dose contributes to the shortening of the onset time. Considering the drug-acting rate and safety into account, menopausal women can be administered with a rational dose of 1200 mg/day to reduce bone loss.




Similar content being viewed by others
Reference
National Osteoporosis Foundation (2002) America’s bone health: the state of osteoporosis and low bone mass in our nation. National Osteoporosis Foundation, Washington, DC
Wright NC, Looker AC, Saag KG et al (2014) The recent prevalence of osteoporosis and low bone mass in the United States based on bone mineral density at the femoral neck or lumbar spine. J Bone Miner Res 29:2520–2526. doi:10.1002/jbmr.2269
Burge R, Dawson-hughes B, Solomon DH et al (2007) Incidence and economic burden of osteoporosis-related fractures in the United States, 2005–2025. J Bone Miner Res 22:465–475. doi:10.1359/JBMR.061113
World Health Organization (1994) Assessment of fracture risk and its application to screening for postmenopausal osteoporosis. WHO technical report series, Geneva
Johnell O, Kanis J (2005) Epidemiology of osteoporotic fractures. Osteoporos Int 16:6–10. doi:10.1007/s00198-004-1702-6
Khosla S, Riggs BL (2005) Pathophysiology of age-related bone loss and osteoporosis. Endocrinol Metab Clin N Am 34:1015–1030. doi:10.1016/j.ecl.2005.07.009
North American Menopause Society (2010) Management of osteoporosis in postmenopausal women: 2010 position statement of the North American Menopause Society. Menopause 17:25–54. doi:10.1097/gme.0b013e3181cdd4a7
Jepsen KJ, Bigelow EMR, Ramcharan M et al (2016) Moving toward a prevention strategy for osteoporosis by giving a voice to a silent disease. Women’s Midlife Heal 2:3. doi:10.1186/s40695-016-0016-0
Cosman F, de Beur SJ, LeBoff MS et al (2014) Clinician’s guide to prevention and treatment of osteoporosis. Osteoporos Int 25:2359–2381. doi:10.1007/s00198-014-2794-2
Food and Nutrition Board and Institute of Medicine Standing Committee on the Scientific Evaluation of Dietary Reference Intakes (1997) Dietary reference intakes for calcium, phosphorus, magnesium, vitamin D, and fluoride. doi: 10.17226/5776
Food and Agriculture Organization, World Health Organization (2001) Human vitamin and mineral requirements. Report of a joint FAO/WHO expert consultation, Bangkok, Thailand. Food and Agriculture Organization of the United Nations, Rome
Committee on Medical Aspects of Food and Nutrition Policy (1998) Report on Health and Social Subjects 49: Report of the Subgroup on Bone Health. London
Reid IR, Bristow SM, Bolland MJ (2015) Calcium supplements: benefits and risks. J Intern Med 278:354–368. doi:10.1111/joim.12394
Walker E, Hernandez AV, Kattan MW (2008) Meta-analysis: its strengths and limitations. Cleve Clin J Med 75:431–439
Levy JI, Fabian MP, Peters JL (2014) Meta-analytic approaches for multistressor dose-response function development: strengths, limitations, and case studies. Risk Anal 35 . doi:10.1111/risa.12208n/a-n/a.
Mould DR (2012) Model-based meta-analysis: an important tool for making quantitative decisions during drug development. Clin Pharmacol Ther 92:283–286. doi:10.1038/clpt.2012.122
Mandema JW, Salinger DH, Baumgartner SW, Gibbs M a (2011) A dose-response meta-analysis for quantifying relative efficacy of biologics in rheumatoid arthritis. Clin Pharmacol Ther 90:828–835. doi:10.1038/clpt.2011.256
Li L, Lv Y, Xu L, Zheng Q (2015) Quantitative efficacy of soy isoflavones on menopausal hot flashes. Br J Clin Pharmacol 79:593–604. doi:10.1111/bcp.12533
Ahn JE, French JL (2010) Longitudinal aggregate data model-based meta-analysis with NONMEM: approaches to handling within treatment arm correlation. J Pharmacokinet Pharmacodyn 37:179–201. doi:10.1007/s10928-010-9152-6
Mandema J, Sweeney K, Terra S, et al Model-based meta-analysis of the HbA1c lowering effect of PF-04971729, a sodium glucose co-transporter-2 inhibitor (SGLT2i), in comparison to other SGLT2i and anti-diabetic agents (ADA).
Liesenfeld K, Schäfer HG, Trocóniz IF et al (2006) Effects of the direct thrombin inhibitor dabigatran on ex vivo coagulation time in orthopaedic surgery patients: a population model analysis. Br J Clin Pharmacol 62:527–537. doi:10.1111/j.1365-2125.2006.02667.x
Health T, Ce S (1997) Basic concepts of pharmacokinetic/pharmacodynamic(PK/PD) modeling. Int J Clin Pharmacol Ther 35:401–413
Gibbs JP, Fredrickson J, Barbee T (2012) Quantitative model of the relationship inhibition and response: meta-analysis of vildagliptin efficacy results. J Clin Pharmacol 52:1494–1505. doi:10.1177/0091270011420153
Beal S, Sheiner L, Boeckmann A, Bauer R (2013) NONMEM users guides. ICON Development Solutions, Ellicott City, MD
Kuti JL, Dandekar PK, Nightingale CH, Nicolau DP (2003) Use of Monte Carlo simulation to design an optimized pharmacodynamic dosing strategy for meropenem. J Clin Pharmacol 43:1116–1123. doi:10.1177/0091270003257225
Goulooze SC, Galettis P, Boddy AV, Martin JH (2016) Monte Carlo simulations of the clinical benefits from therapeutic drug monitoring of sunitinib in patients with gastrointestinal stromal tumours. Cancer Chemother Pharmacol 78:209–216. doi:10.1007/s00280-016-3071-1
Post TM, Freijer JI, Ploeger BA (2008) Extensions to the visual predictive check to facilitate model performance evaluation. J Pharmacokinet Pharmacodyn:185–202. doi:10.1007/s10928-007-9081-1
Holford NHG, Chan PLS, Nutt JG et al (2006) Disease progression and pharmacodynamics in Parkinson disease—evidence for functional protection with levodopa and other treatments. J Pharmacokinet Pharmacodyn 33:281–311. doi:10.1007/s10928-006-9012-6
Serbin SP, Dillaway DN, Kruger EL, Townsend PA (2012) Leaf optical properties reflect variation in photosynthetic metabolism and its sensitivity to temperature. J Exp Bot 63:489–502. doi:10.1093/jxb/err294
Bjarnason NH, Alexandersen P, Christiansen C (2002) Number of years since menopause: spontaneous bone loss is dependent but response to hormone replacement therapy is independent. Bone 30:637–642. doi:10.1016/S8756-3282(02)00678-6
Wilsnack RW, Wilsnack SC (2016) Calcium supplements: do they help or harm? Menopause 2:5–8
Reid IR, Mason B, Horne A et al (2006) Randomized controlled trial of calcium in healthy older women. Am J Med 119:777–785. doi:10.1016/j.amjmed.2006.02.038
Wang X, Chen H, Ouyang Y et al (2014) Dietary calcium intake and mortality risk from cardiovascular disease and all causes: a meta-analysis of prospective cohort studies. BMC Med 12:1–23. doi:10.1186/s12916-014-0158-6
Rosen CJ (2006) Age-related osteoporosis and skeletal markers of bone turnover. In: Dyn. Bone Cartil. Metab., 2 Edition. Academies Press, pp 671–687
Committee to Review Dietary Reference Intakes for Vitamin D and Calcium Food and Nutrition Board (2011) Dietary reference intakes for calcium and vitamin D. National Academies Press, Washington, DC
Food and Agriculture Organization of the United Nations (2010) FAO Statistics Division 2010. Food balance sheets.
Tai V, Leung W, Grey A et al (2015) Calcium intake and bone mineral density: systematic review and meta-analysis. BMJ 351:h4183. doi:10.1136/bmj.h4183
Fujita T, Ohue T, Fujii Y et al (1996) Heated oyster shell-seaweed calcium (AAA Ca) on osteoporosis. Calcif Tissue Int 58:226–230. doi:10.1007/BF02508640
Gui J-C, Brašić JR, Liu X-D et al (2012) Bone mineral density in postmenopausal Chinese women treated with calcium fortification in soymilk and cow’s milk. Osteoporos Int 23:1563–1570. doi:10.1007/s00198-012-1895-z
Manios Y, Moschonis G, Trovas G, Lyritis GP (2007) Changes in biochemical indexes of bone metabolism and bone mineral density after a 12-mo dietary intervention program: the postmenopausal health study. Am J Clin Nutr 86:781–789. doi:10.3945/ajcn.113.073056.1
Strause L, Saltman P, Smith KT et al (1994) Spinal bone loss in postmenopausal women supplemented with calcium and trace minerals. J Nutr 124:1060–1064
Baeksgaard L, Andersen KP, Hyldstrup L (1998) Calcium and vitamin D supplementation increases spinal BMD in healthy, postmenopausal women. Osteoporos Int 8:255–260. doi:10.1007/s001980050062
Dawson-Hughes B, Dallal GE, Krall EA et al (1990) A controlled trial of the effect of calcium supplementation on bone density in postmenopausal women. N Engl J Med 323:878–883. doi:10.1056/NEJM199009273231305
Nakamura K, Saito T, Kobayashi R et al (2012) Effect of low-dose calcium supplements on bone loss in perimenopausal and postmenopausal Asian women: a randomized controlled trial. J Bone Miner Res 27:2264–2270. doi:10.1002/jbmr.1676
Rajatanavin R, Chailurkit L, Saetung S et al (2013) The efficacy of calcium supplementation alone in elderly Thai women over a 2-year period: a randomized controlled trial. Osteoporos Int 24:2871–2877. doi:10.1007/s00198-013-2387-5
Ruml LA, Sakhaee K, Peterson R et al (1999) The effect of calcium citrate on bone density in the early and mid-postmenopausal period: a randomized placebo-controlled study. Am J Ther 6:303–311
Son SM, Chun YN (2001) Effect of oral therapy with alphacalcidol or calcium in Korean elderly women with osteopenia and low dietary calcium. Nutr Res 21:1347–1355. doi:10.1016/S0271-5317(01)00317-7
Storm D, Eslin R, Porter ES et al (1998) Calcium supplementation prevents seasonal bone loss and changes in biochemical markers of bone turnover in elderly New England women: a randomized placebo controlled trial. J Clin Endocrinol {&} Metab 83:3817–3825
Chee WSS, Suriah AR, Chan SP et al (2003) The effect of milk supplementation on bone mineral density in postmenopausal Chinese women in Malaysia. Osteoporos Int 14:828–834. doi:10.1007/s00198-003-1448-6
ELDERS PJM, NETELENBOS JC, LIPS P et al (1991) Calcium supplementation reduces vertebral bone loss in perimenopausal women: a controlled trial in 248 women between 46 and 55 years of age*. J Clin Endocrinol Metab 73:533–540. doi:10.1210/jcem-73-3-533
Grados F, Brazier M, Kamel S et al (2003) Effects on bone mineral density of calcium and vitamin D supplementation in elderly women with vitamin D deficiency. Jt Bone Spine 70:203–208. doi:10.1016/S1297-319X(03)00046-0
Lau EM, Woo J, Lam V, Hong A (2001) Milk supplementation of the diet of postmenopausal Chinese women on a low calcium intake retards bone loss. J Bone Miner Res 16:1704–1709. doi:10.1359/jbmr.2001.16.9.1704
Lau EMC, Woo J, Leung PC et al (1992) The effects of calcium supplementation and exercise on bone density in elderly Chinese women. Osteoporos Int 2:168–173. doi:10.1007/BF01623922
Reid IR, Ames RW, Evans MC et al (1993) Effect of calcium supplementation on bone loss in postmenopausal women. N Engl J Med 328:460–464. doi:10.1056/NEJM199302183280702
Acknowledgements
This study was financially supported by the project budget for Shanghai University of Traditional Chinese Medicine (2014YSN17).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflicts of interest
None.
Electronic supplementary material
ESM 1
(PDF 1345 kb)
Rights and permissions
About this article
Cite this article
Wu, J., Xu, L., Lv, Y. et al. Quantitative analysis of efficacy and associated factors of calcium intake on bone mineral density in postmenopausal women. Osteoporos Int 28, 2003–2010 (2017). https://doi.org/10.1007/s00198-017-3993-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-017-3993-4