Abstract
Summary
We detected disease-causing mutations in 585 of 598 individuals (98 %) with typical features of osteogenesis imperfecta (OI). In mild OI, only collagen type I encoding genes were involved. In moderate to severe OI, mutations in 12 different genes were found; 11 % of these patients had mutations in recessive genes.
Introduction
OI is usually caused by mutations in COL1A1 or COL1A2, the genes encoding collagen type I alpha chains, but mutations in at least 16 other genes have also been associated with OI. It is presently unknown what proportion of individuals with clinical features of OI has a disease-causing mutation in one of these genes.
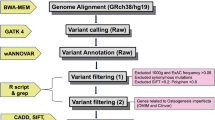
Methods
DNA sequence analysis was performed on 598 individuals from 487 families who had a typical OI phenotype. OI type I was diagnosed in 43 % of individuals, and 57 % had moderate to severe OI, defined as OI types other than type I.
Results
Disease-causing variants were detected in 97 % of individuals with OI type I and in 99 % of patients with moderate to severe OI. All mutations found in OI type I were dominant and exclusively affected COL1A1 or COL1A2. In moderate to severe OI, dominant mutations were found in COL1A1/COL1A2 (77 %), IFITM5 (9 %), and P4HB (0.6 %). Mutations in one of the recessive OI-associated gene were observed in 12 % of individuals with moderate to severe OI. The genes most frequently involved in recessive OI were SERPINF1 (4.0 % of individuals with moderate to severe OI) and CRTAP (2.9 %).
Conclusions
DNA sequence analysis of currently known OI-associated genes identifies disease-causing variants in almost all individuals with a typical OI phenotype. About 20 % of individuals with moderate to severe OI had mutations in genes other than COL1A1/COL1A2.

Similar content being viewed by others
References
Forlino A, Marini JC (2016) Osteogenesis imperfecta. Lancet 387:1657–1671
Sillence DO, Senn A, Danks DM (1979) Genetic heterogeneity in osteogenesis imperfecta. J Med Genet 16:101–116
Bonafe L, Cormier-Daire V, Hall C et al (2015) Nosology and classification of genetic skeletal disorders: 2015 revision. Am J Med Genet A 167A:2869–2892
Rauch F, Glorieux FH (2004) Osteogenesis imperfecta. Lancet 363:1377–1385
Van Dijk FS, Sillence DO (2014) Osteogenesis imperfecta: clinical diagnosis, nomenclature and severity assessment. Am J Med Genet A 164A:1470–1481
Bonadio J, Holbrook KA, Gelinas RE, Jacob J, Byers PH (1985) Altered triple helical structure of type I procollagen in lethal perinatal osteogenesis imperfecta. J Biol Chem 260:1734–1742
Wenstrup RJ, Willing MC, Starman BJ, Byers PH (1990) Distinct biochemical phenotypes predict clinical severity in nonlethal variants of osteogenesis imperfecta. Am J Hum Genet 46:975–982
Lindahl K, Astrom E, Rubin CJ, Grigelioniene G, Malmgren B, Ljunggren O, Kindmark A (2015) Genetic epidemiology, prevalence, and genotype-phenotype correlations in the Swedish population with osteogenesis imperfecta. Eur J Hum Genet 23:1042–1050
Ogden CL, Kuczmarski RJ, Flegal KM, Mei Z, Guo S, Wei R, Grummer-Strawn LM, Curtin LR, Roche AF, Johnson CL (2002) Centers for Disease Control and Prevention 2000 growth charts for the United States: improvements to the 1977 National Center for Health Statistics version. Pediatrics 109:45–60
Korkko J, Ala-Kokko L, De Paepe A, Nuytinck L, Earley J, Prockop DJ (1998) Analysis of the COL1A1 and COL1A2 genes by PCR amplification and scanning by conformation-sensitive gel electrophoresis identifies only COL1A1 mutations in 15 patients with osteogenesis imperfecta type I: identification of common sequences of null-allele mutations. Am J Hum Genet 62:98–110
Rauch F, Lalic L, Glorieux FH, Moffatt P, Roughley P (2014) Targeted sequencing of a pediatric metabolic bone gene panel using a desktop semiconductor next-generation sequencer. Calcif Tissue Int 95:323–331
Richards S, Aziz N, Bale S et al (2015) Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med 17:405–424
Bardai G, Lemyre E, Moffatt P, Palomo T, Glorieux FH, Tung J, Ward L, Rauch F (2016) Osteogenesis imperfecta type I caused by COL1A1 deletions. Calcif Tissue Int 98:76–84
Rauch F, Moffatt P, Cheung M, Roughley P, Lalic L, Lund AM, Ramirez N, Fahiminiya S, Majewski J, Glorieux FH (2013) Osteogenesis imperfecta type V: marked phenotypic variability despite the presence of the IFITM5 c.-14C > T mutation in all patients. J Med Genet 50:21–24
Rauch F, Fahiminiya S, Majewski J, Carrot-Zhang J, Boudko S, Glorieux F, Mort JS, Bachinger HP, Moffatt P (2015) Cole-Carpenter syndrome is caused by a heterozygous missense mutation in P4HB. Am J Hum Genet 96:425–431
Wekre LL, Froslie KF, Haugen L, Falch JA (2010) A population-based study of demographical variables and ability to perform activities of daily living in adults with osteogenesis imperfecta. Disabil Rehabil 32:579–587
van Dijk FS, Byers PH, Dalgleish R, Malfait F, Maugeri A, Rohrbach M, Symoens S, Sistermans EA, Pals G (2012) EMQN best practice guidelines for the laboratory diagnosis of osteogenesis imperfecta. Eur J Hum Genet 20:11–19
Pepin MG, Byers PH (2015) What every clinical geneticist should know about testing for osteogenesis imperfecta in suspected child abuse cases. Am J Med Genet C Semin Med Genet 169:307–313
Sykes B, Ogilvie D, Wordsworth P et al (1990) Consistent linkage of dominantly inherited osteogenesis imperfecta to the type I collagen loci: COL1A1 and COL1A2. Am J Hum Genet 46:293–307
Cho TJ, Lee KE, Lee SK et al (2012) A single recurrent mutation in the 5′-UTR of IFITM5 causes osteogenesis imperfecta type V. Am J Hum Genet 91:343–348
Rauch F, Husseini A, Roughley P, Glorieux FH, Moffatt P (2012) Lack of circulating pigment epithelium-derived factor is a marker of osteogenesis imperfecta type VI. J Clin Endocrinol Metab 97:E1550–E1556
Ward LM, Rauch F, Travers R, Chabot G, Azouz EM, Lalic L, Roughley PJ, Glorieux FH (2002) Osteogenesis imperfecta type VII: an autosomal recessive form of brittle bone disease. Bone 31:12–18
Morello R, Bertin TK, Chen Y et al (2006) CRTAP is required for prolyl 3-hydroxylation and mutations cause recessive osteogenesis imperfecta. Cell 127:291–304
Forlino A, Cabral WA, Barnes AM, Marini JC (2011) New perspectives on osteogenesis imperfecta. Nat Rev Endocrinol 7:540–557
Fahiminiya S, Majewski J, Al-Jallad H, Moffatt P, Mort J, Glorieux FH, Roschger P, Klaushofer K, Rauch F (2014) Osteoporosis caused by mutations in PLS3: clinical and bone tissue characteristics. J Bone Miner Res 29:1805–1814
Fahiminiya S, Al-Jallad H, Majewski J, Palomo T, Moffatt P, Roschger P, Klaushofer K, Glorieux FH, Rauch F (2015) A polyadenylation site variant causes transcript-specific BMP1 deficiency and frequent fractures in children. Hum Mol Genet 24:516–524
Acknowledgments
We thank Patty Mason for technical assistance and Mark Lepik for the preparation of the figures. F.R. received salary support from the Chercheur-Boursier Clinicien program of the Fonds de Recherche du Québec-Santé. This study was supported by the Shriners of North America and the Fonds de recherche Québec-Santé.
Roles of the authors
GB performed analyses. FHG contributed patient information. PM revised manuscript content. FR conceptualized the project, contributed patient information, finalized the report, and accepts responsibility for the integrity of the data analysis. All authors have read and approved the final version of the manuscript.
Conflicts of interest
Ghalib Bardai, Pierre Moffatt, Francis H Glorieux, and Frank Rauch declare that they have no conflict of interest.
Web resources
Exome Aggregation Consortium (ExAC) Browser: http://exac.broadinstitute.org/
Online Mendelian Inheritance in Man (OMIM), http://www.omim.org
Osteogenesis Imperfecta Variant Database: https://oi.gene.le.ac.uk/
UCSC database, version hg19: http://www.genome.ucsc.edu/
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOCX 239 kb)
Rights and permissions
About this article
Cite this article
Bardai, G., Moffatt, P., Glorieux, F.H. et al. DNA sequence analysis in 598 individuals with a clinical diagnosis of osteogenesis imperfecta: diagnostic yield and mutation spectrum. Osteoporos Int 27, 3607–3613 (2016). https://doi.org/10.1007/s00198-016-3709-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-016-3709-1