Abstract
Summary
The addition of Limited Use criteria (less restrictive access) for zoledronic acid resulted in an immediate and significant increase in uptake and resulted in differences in patient/physician characteristics. In comparison, the uptake of denosumab (only listed with Limited Use) was rapid. Thus, formulary access restrictions have significant implications for prescribing.
Introduction
We sought to describe the use of zoledronic acid and denosumab by physicians and patients over time and examine the impact of a 2012 provincial formulary modification that removed the administrative burden on physicians when prescribing zoledronic acid.
Methods
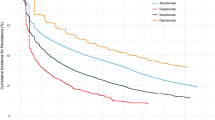
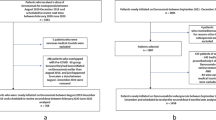
We identified users of zoledronic acid and denosumab using Ontario pharmacy claims data. The number of new patients and physicians was plotted and examined over time. Interrupted time series analysis examined the impact of a formulary modification to zoledronic acid use and prescribing. Descriptive characteristics of patients and prescribers were summarized pre- and post-formulary modification for zoledronic acid and overall for denosumab.
Results
We identified 1463 zoledronic acid patients treated by 627 physicians and 16,736 denosumab patients treated by 2904 physicians. In the first 2 months on the market, we identified a rapid uptake of denosumab (>450 physicians and >1200 patients) in contrast to zoledronic acid (<10 physicians and <10 patients). Zoledronic acid use increased significantly in the 2-month post-formulary change, yet no change in denosumab was observed. Prior to the formulary modification, more zoledronic acid patients had a history of osteoporosis therapy (41 vs. 26 %) or bone density testing (30 vs. 10 %). Compared to zoledronic patients (post-formulary modification), more denosumab patients had prior osteoporosis therapy (55 vs. 26 %), yet fewer had a gastrointestinal diagnosis (6 vs. 11 %).
Conclusion
We identified a rapid uptake of denosumab in only 15 months of observation. A provincial formulary modification to zoledronic acid resulted in an increase in utilization and impacted patient characteristics.



Similar content being viewed by others
References
Aclasta receives Health Canada approval as once-yearly treatment for postmenopausal osteoporosis. November 6th, 2007. http://www.firstwordpharma.com/node/79998?tsid=17#axzz35a6Vb8bz
Prolia (denosumab) approved by Health Canada for the treatment of postmenopausal women with osteoporosis at high risk for fracture. September 8, 2010. In: Amgen. http://www.amgen.ca/english/media/treatment_of_postmenopausal.html
Women in Ontario now have access to Prolia (denosumab) for postmenopausal osteoporosis. February 29, 2012. http://www.newswire.ca/en/story/929571/women-in-ontario-now-have-access-to-prolia-denosumab-for-postmenopausal-osteoporosis
Gamble J-M, McAlister FA, Johnson JA, Eurich DT (2012) Restrictive drug coverage policies can induce substantial drug exposure misclassification in pharmacoepidemiologic studies. Clin Ther 34:1379–1386. doi:10.1016/j.clinthera.2012.04.009, e3
Schneeweiss S, Gagne JJ, Glynn RJ et al (2011) Assessing the comparative effectiveness of newly marketed medications: methodological challenges and implications for drug development. Clin Pharmacol Ther 90:777–790. doi:10.1038/clpt.2011.235
Ontario Ministry of Health and Long-Term Care. Ontario Public Drug Programs - Exceptional Access Program. http://www.health.gov.on.ca/en/pro/programs/drugs/eap_mn.aspx
(2012) New limited use code for zoledronic acid. In: Ontario Rheumatol. Assoc. http://ontariorheum.ca/home/new-limited-use-code-for-zolendronic-acid. Accessed 4 Jan 2014
Limited use codes for zoledronic acid and denosumab. In: Ontario Rheumatol. Assoc. http://ontariorheum.ca/drug-forms-and-codes/limited-use-codes
Cramer JA, Amonkar MM, Hebborn A, Altman R (2005) Compliance and persistence with bisphosphonate dosing regimens among women with postmenopausal osteoporosis. Curr Med Res Opin 21:1453–1460. doi:10.1185/030079905X61875
Ringe JD, Farahmand P (2013) Improved real-life adherence of 6-monthly denosumab injections due to positive feedback based on rapid 6-month BMD increase and good safety profile. Rheumatol Int. doi:10.1007/s00296-012-2663-2
Penning-van Beest FJA, Goettsch WG, Erkens JA, Herings RMC (2006) Determinants of persistence with bisphosphonates: a study in women with postmenopausal osteoporosis. Clin Ther 28:236–242. doi:10.1016/j.clinthera.2006.01.002
Hashim S, Gomes T, Juurlink D et al (2013) The rise and fall of the thiazolidinediones: impact of clinical evidence publication and formulary change on the prescription incidence of thiazolidinediones. J Popul Ther Clin Pharmacol 20:e238–e242
Dickey DA, Fuller WA (1979) Distribution of the estimators for autoregressive time series with a unit root. J Am Stat Assoc 74:427–431
Ljung GM, Box GEP (1978) On a measure of lack of fit in time series models. Biometrika 65:297–303. doi:10.1093/biomet/65.2.297
Brown JP, Morin S, Leslie W et al (2014) Bisphosphonates for treatment of osteoporosis: expected benefits, potential harms, and drug holidays. Can Fam Physician 60:324–333
Ontario Ministry of Health and Long-Term Care. Ontario Drug Benefit Program: once you turn age 65
Cadarette SM, Carney G, Baek D et al (2012) Osteoporosis medication prescribing in British Columbia and Ontario: impact of public drug coverage. Osteoporos Int 23:1475–1480. doi:10.1007/s00198-011-1771-2
Boonen S, Sellmeyer DE, Lippuner K et al (2008) Renal safety of annual zoledronic acid infusions in osteoporotic postmenopausal women. Kidney Int 74:641–648. doi:10.1038/ki.2008.193
Jandoc R, Burden AM, Mamdani M, Cadarette SM Time series methods in drug utilization research: a systematic review [abstract]. J Clin Epi
Tadrous M, Juurlink DN, Krahn MD, et al. (2014) Looking both ways before using the disease risk score (DRS): performance of the DRS in a cohort with known selection bias. Pharmacoepidemiol Drug Saf 249
Crilly RG, Tanner DA, Kloseck M, Chesworth BM (2010) Hip fractures in long-term care: is the excess explained by the age and gender distribution of the residents? J Aging Res 2010:291258. doi:10.4061/2010/291258
Penfold RB, Zhang F Use of interrupted time series analysis in evaluating health care quality improvements. Acad Pediatr 13:S38–44. doi: 10.1016/j.acap.2013.08.002
Zhang F, Wagner AK, Soumerai SB, Ross-Degnan D (2009) Methods for estimating confidence intervals in interrupted time series analyses of health interventions. J Clin Epidemiol 62:143–148. doi:10.1016/j.jclinepi.2008.08.007
Wagner AK, Soumerai SB, Zhang F, Ross-Degnan D (2002) Segmented regression analysis of interrupted time series studies in medication use research. J Clin Pharm Ther 27:299–309. doi:10.1046/j.1365-2710.2002.00430.x
Acknowledgments
This research was supported by a research grant to Dr. Cadarette from the Ontario Ministry of Research and Innovation (OMRI, Early Research Award ER09-06-043). Dr. Cadarette was supported by a CIHR New Investigator Award in Aging and Osteoporosis (MSH-95364), Andrea Burden was supported by an Ontario Graduate Scholarship for doctoral research, and Mina Tadrous was supported by a CIHR Doctoral Award—Frederick Banting and Charles Best Canada Graduate Scholarship (GSD-11342). The authors acknowledge Brogan Inc. for providing access to drug identification numbers used to identify eligible drugs and the Institute for Clinical Evaluative Sciences (ICES) where all data analyses were completed. ICES is a non-profit research corporation funded by the Ontario Ministry of Health and Long-Term Care. As a prescribed entity under Ontario’s privacy law (Section 45 of the Personal Health Information Protection Act and Regulation 329/04, Section 18), ICES is legally permitted to receive and use personal health information for health services research. To have this privilege, ICES maintains policies, practices, and procedures that are approved and regularly audited by the Information and Privacy Commissioner of Ontario (www.ipc.on.ca). The opinions, results, and conclusions are those of the authors and are independent from the funding sources. No endorsement by CIHR, ICES, OMRI, or the Ontario Ministry of Health and Long-Term Care is intended or should be inferred.
A portion of this research was presented at the following conferences: The International Osteoporosis Foundation World Congress on Osteoporosis, Osteoarthritis, and Musculoskeletal Diseases in Seville, Spain, April 2014; The Canadian Association for Health Services and Policy Research Annual Conference in Toronto ON, Canada, May 2014. This work has also been accepted for presentation at the American Society for Bone and Mineral Research Annual Meeting in Houston, TX, USA, September 2014, and at the International Conference of Pharmacoepidemiology and Therapeutic Risk Management in Taipei, Taiwan, October 2014.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Burden, A.M., Tadrous, M., Calzavara, A. et al. Uptake and characteristics of zoledronic acid and denosumab patients and physicians in Ontario, Canada: impact of drug formulary access. Osteoporos Int 26, 1525–1533 (2015). https://doi.org/10.1007/s00198-014-3023-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-014-3023-8