Abstract
Summary
The study aims to estimate the direct disease-related costs of osteoporotic vertebral compression fractures (OVCF) in patients with newly diagnosed fracture in the first year after index in Germany. Analyses reveal that OVCFs are associated with significant costs. In light of high and increasing incidence, the results emphasize importance of research in this field.
Introduction
OVCF are among the most common fractures related to osteoporosis. They have been shown to be associated with excess mortality and meaningful healthcare costs. Costs calculations have illustrated the significant financial burden to society and national social security systems. However, this information is not available for Germany. Therefore, aim of the study was to estimate the direct disease-related costs of OVCF in patients with newly diagnosed fracture in the first year after index in Germany.
Methods
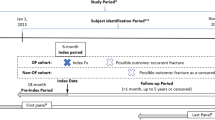
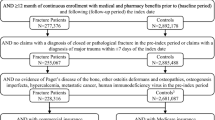
Data were obtained from a claims dataset of a large German health insurance fund. Subjects ≥60 years with a new vertebral fracture between 2006 and 2010 were studied retrospectively compared to a matched paired OVCF-free patient group. All-cause and fracture-specific medical costs were calculated in the 1-year baseline and follow-up period. Generalized linear model (GLM) was estimated for total follow-up healthcare cost.
Results
A total of 2,277 pairs of matched OVCF and OVCF-free patients were included in the analysis. Baseline costs were higher in the OVCF group. Mean unadjusted all-cause healthcare cost difference in the four quarters following the index date between OVCF and OVCF-free patients was 8,200 € (p < 0.001). Of the difference, almost two third was attributable to inpatient services and one quarter to prescription drug costs. The GLM procedure revealed that OVCF-related costs in the first year after the index date add up to 6,490 € (p < 0.001; CI 5,809 €–6,731 €).
Conclusions
Despite limitations of this study, our results are consistent with other research and demonstrate that OVCFs are associated with significant costs. The results underline the importance of medical interventions that can help to prevent fractures and treatments, which are cost-effective and can prevent recurrent fractures.



Similar content being viewed by others
References
(1991) Consensus development conference: prophylaxis and treatment of osteoporosis. The American Journal of Medicine 90:107–110. doi: 10.1016/0002-9343(91)90512-V
Häussler B, Gothe H, Göl D, Glaeske G, Pientka L, Felsenberg D (2007) Epidemiology, treatment and costs of osteoporosis in Germany—the BoneEVA Study. Osteoporos Int 18:77–84. doi:10.1007/s00198-006-0206-y
Becker S, Ogon M (2006) Balloon kyphoplasty. Springer, Wien
Johnell O, Kanis JA (2006) An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int 17:1726–1733
Cooper C, Cole ZA, Holroyd CR, Earl SC, Harvey NC, Dennison EM, Melton LJ, Cummings SR, Kanis JA (2011) Secular trends in the incidence of hip and other osteoporotic fractures. Osteoporos Int 22:1277–1288. doi:10.1007/s00198-011-1601-6
Ström O, Borgström F, Kanis JA, Compston J, Cooper C, McCloskey EV, Jónsson B (2011) Osteoporosis: burden, health care provision and opportunities in the EU: a report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos 6:59–155. doi:10.1007/s11657-011-0060-1
Hernlund E, Svedbom A, Ivergård M, Compston J, Cooper C, Stenmark J, McCloskey EV, Jönsson B, Kanis JA (2013) Osteoporosis in the European Union: medical management, epidemiology and economic burden. Arch Osteoporos 8. doi: 10.1007/s11657-013-0136-1
Lau E, Ong KL, Kurtz SM, Schmier J, Edidin AA (2008) Mortality following the diagnosis of a vertebral compression fracture in the Medicare population. J Bone Joint Surg Am 90:1479–1486
Dimai H, Redlich K, Peretz M, Borgström F, Siebert U, Mahlich J (2012) Economic burden of osteoporotic fractures in Austria. Health Econ Rev 2:12. doi:10.1186/2191-1991-2-12
Sedrine WB, Radican L, Raginster J (2001) On conducting burden-of-osteoporosis studies: a review of the core concepts and practical issues. A study carried out under the auspices of a WHO Collaborating Center. Rheumatology 40:7–14. doi:10.1093/rheumatology/40.1.7
Lange A, Kasperk C, Alvares L, Sauermann S, Braun S (2014) Survival and cost comparison of kyphoplasty and percutaneous vertebroplasty using German claims data. Spine 39:318–326. doi: 10.1097/BRS.0000000000000135
Kassenärztliche Bundesvereinigung (ed) (2008) Erweiterter Bewertungsausschuss nach § 87 Abs. 4 SGB V—7. Sitzung, 27./28. August 2008; Teil A zur erstmaligen Festlegung des Orientierungswertes nach § 87 Abs. 2e Satz 1 Nr. 1 SGB V für das Jahr 2009. 2008
Prenzler A, Zeidler J, Braun S, Schulenburg J (2010) Bewertung von Ressourcen im Gesundheitswesen aus der Perspektive der deutschen Sozialversicherung. Pharmacoeconomics Ger Res Art 8:47–66. doi:10.1007/BF03320765
Elixhauser A, Steiner C, Harris DR, Coffey RM (1998) Comorbidity measures for use with administrative data. Med Care 36:8–27
Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, Saunders LD, Beck CA, Feasby TE, Ghali WA (2005) Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10. Med Care 43:1130–1139
van Walraven C, Austin PC, Jennings A, Quan H, Forster AJ (2009) A modification of the Elixhauser comorbidity measures into a point system for hospital death using administrative data. Med Care 47:626–633. doi:10.1097/MLR.0b013e31819432e5
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40:373–383
Ho DE, Imai K, King G, Stuart EA (2006) Matching as nonparametric preprocessing for reducing model dependence in parametric causal inference. Polit Anal 15:199–236. doi:10.1093/pan/mpl013
Manning WG, Mullahy J (2001) Estimating log models: to transform or not to transform? J Health Econ 20:461–494. doi:10.1016/S0167-6296(01)00086-8
Pregibon D (1980) Goodness of link tests for generalized linear models. J R Stat Soc: Ser C: Appl Stat 29:15–24. doi:10.2307/2346405
Hosmer DW, Lemeshow S (2000) Applied logistic regression, 2nd edn. Wiley-Interscience, New York
Wedderburn RW (1974) Quasi-likelihood functions, generalized linear models, and the Gauss-Newton method. Biometrika 61:439–447. doi:10.2307/2334725
Manning WG (1998) The logged dependent variable, heteroscedasticity, and the retransformation problem. J Health Econ 17:283–295. doi:10.1016/S0167-6296(98)00025-3
Glick HA, Doshi JA, Sonnad SS, Polsky D (2007) Economic evaluation in clinical trials. Oxford Univ. Press, Oxford
Wooldridge JM (2010) Econometric analysis of cross section and panel data, 2nd edn. MIT Press, Cambridge
Gabriel SE, Tosteson AN, Leibson CL, Crowson CS, Pond GR, Melton LJ, Hammond CS (2002) Direct medical costs attributable to osteoporotic fractures. Osteoporos Int 13:323–330
Ray NF, Chan JK, Thamer M, Melton LJ (1997) Medical expenditures for the treatment of osteoporotic fractures in the United States in 1995: report from the National Osteoporosis Foundation. J Bone Miner Res 12:24–35. doi:10.1359/jbmr.1997.12.1.24
de Laet CE, van Hout BA, Burger H, Weel AE, Hofman A, Pols HA (1999) Incremental cost of medical care after hip fracture and first vertebral fracture. The Rotterdam study. Osteoporos Int 10:66–72
Shi N, Foley K, Lenhart G, Badamgarav E (2009) Direct healthcare costs of hip, vertebral, and non-hip, non-vertebral fractures. Bone 45:1084–1090. doi:10.1016/j.bone.2009.07.086
Rousculp MD, Long SR, Wang S, Schoenfeld MJ, Meadows ES (2007) Economic burden of osteoporosis-related fractures in Medicaid. Value Health 10:144–152. doi:10.1111/j.1524-4733.2006.00161.x
Rovithis D (2013) Do health economic evaluations using observational data provide reliable assessment of treatment effects? Health Econ Rev 3:21. doi:10.1186/2191-1991-3-21
Rubin DB (1973) The use of matched sampling and regression adjustment to remove bias in observational studies. Biometrics 29:185–203. doi:10.2307/2529685
Borgström F (2006) Health economics of osteoporosis, Stockholm
Borgström F, Sobocki P, Strom O, Jonsson B (2007) The societal burden of osteoporosis in Sweden. Bone 40:1602–1609. doi:10.1016/j.bone.2007.02.027
Ong KL, Lau E, Kemner JE, Kurtz SM (2013) Two-year cost comparison of vertebroplasty and kyphoplasty for the treatment of vertebral compression fractures: are initial surgical costs misleading? Osteoporos Int 24:1437–1445. doi:10.1007/s00198-012-2100-0
Stuart EA (2010) Matching methods for causal inference: a review and a look forward. Stat Sci 25:1–21. doi:10.1214/09-STS313
Conflicts of interest
None.
The study was funded by an unrestricted grant from Medtronic International. Herescon GmbH has received payment from Medtronic.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lange, A., Zeidler, J. & Braun, S. One-year disease-related health care costs of incident vertebral fractures in osteoporotic patients. Osteoporos Int 25, 2435–2443 (2014). https://doi.org/10.1007/s00198-014-2776-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-014-2776-4