Abstract
Summary
Twenty-nine children with malignancies and age, gender-matched controls were prospectively studied over 14 months. Patients had higher parathyroid hormone (PTH) levels and fat mass, lower bone mass, and bone mass increments at follow-up than controls. Lean mass, age at diagnosis, systemic and intrathecal therapy were predictors of bone mass changes on adjusted analyses.
Introduction
Children with hematologic malignances have low bone mass. We prospectively investigated anthropometric, clinical, and hormonal predictors of changes in bone mass in children receiving cancer therapy.
Methods
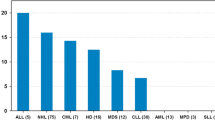
Twenty-nine children, mean age of 9 ± 2.9 years and 32 age and gender-matched controls, were studied. Seven had completed their course 40 ± 22 weeks prior, while 22 were still receiving therapy for 80 ± 28 weeks. Age at diagnosis, calcium intake, exercise activity, systemic corticosteroids in dexamethasone (Dex) dose, and methotrexate (MTX), and intrathecal MTX therapy received within follow-up period were assessed. Routine chemistries, PTH, 25-hydroxy vitamin D (25-OHD), bone remodeling markers, bone mass, and body composition were measured at baseline and 14 months.
Results
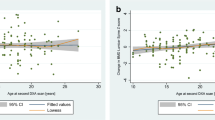
Patients had lower exercise activity, sun exposure, and bone markers levels than controls. They had higher PTH levels and fat mass, lower bone mass at the spine, hip, and total body, and lower increments at these sites on follow-up. Predictors of bone mass changes on univariate analyses were: age at diagnosis (R = −0.50 to −0.44, p < 0.05), Dex–MTX doses (R = −0.58 to −0.41, p < 0.05), intrathecal therapy (p < 0.03),% changes in lean mass (R = 0.37 to 0.54, p < 0.04), 25-OHD levels (R = 0.39, p < 0.03), and PTH levels (R = −0.47 to −0.41, p < 0.05). Lean mass, age at diagnosis, systemic and intrathecal therapy were predictors of bone mass changes on adjusted analyses.
Conclusion
This study provides insight into the pathophysiology of bone loss in children receiving cancer therapy and possible interventions to optimize their skeletal health.
Similar content being viewed by others
Abbreviations
- MTX:
-
Methotrexate
- CS:
-
Corticosteroids
- Dex:
-
Dexamethasone
- S-Ca:
-
Serum calcium
- S-P:
-
Serum phosphorus
- S-Mg:
-
Serum magnesium
- S-Cr:
-
Serum creatinine
- TSP:
-
Total serum protein
- PTH:
-
Parathyroid hormone
- 25-OHD:
-
25-hydroxy vitamin D
- ALKP:
-
Alkaline phosphatase
- S-Osteocalcin:
-
Serum osteocalcin
- S-Crosslaps:
-
Serum crosslaps
- BMD:
-
Bone mineral density
- BMC:
-
Bone mineral content
- BMAD:
-
Bone mineral adjusted density
References
Tillman V, Darlington ASE, Eiser C, Bishop NJ, Davies HA (2002) Male sex and low physical activity are associated with reduced spine bone mineral density in survivors of childhood acute lymphoblastic leukemia. J Bone Miner Res 17:1073–1080
Mulder JE, Bilezikian JP (2004) Bone density in survivors of childhood cancer. J Clin Densitom 7:432–442
Pagano-Therrien J, Santacroce SJ (2005) Bone mineral density decrements and children diagnosed with cancer. J Pediatr Oncol Nurs 22:328–338
Arikoski P, Komulainen J, Riikonen P, Jurvelin JS, Voutilainen R, Kroger H (1999) Reduced bone density at completion of chemotherapy for a malignancy. Arch Dis Child 80:143–148
Nysom K, Holm K, Michaelsen KF, Hetrz H, Muller J, Molgaard C (2001) Bone mass after treatment of malignant lymphoma in childhood. Med Pediatr Oncol 37:518–524
Hoorweg-Nijman JJ, Kardos G, Roos JC et al (1999) Bone mineral density and markers of bone turnover in young adult survivors of childhood lymphoblastic leukaemia. Clin Endocrinol 50:237–244
Chaiban J, Muwakkit S, Arabi A et al (2009) Modeling pathways for low bone mass in children with malignancies. J Clin Densitom 12:441–449
Kaste SC, Ahn H, Liu T et al (2008) Bone mineral density deficits in pediatric patients treated for sarcoma. Pediatr Blood Canc 50:1032–1038
Wasilewski-Masker K, Kaste S, Hudson M, Esiashvili N, Mattano L, Meacham L (2008) Bone mineral density deficits in survivors of childhood cancer: long term follow-up guidelines and review of the literature. Pediatrics 121:e705–e713
Pui CH, Evans WE (2006) Treatment of acute lymphoblastic leukemia. N Engl J Med 354:166–178
Halton J, Gaboury I, Grant R et al (2009) Advanced vertebral fracture among newly diagnosed children with acute lymphoblastic leukemia: results of the Canadian Steroid-Associated Osteoporosis in the Pediatric Population (STOPP) research program. J Bone Miner Res 24:1326–1334
Kelly J, Damron T, Grant W et al (2005) Cross-sectional study of bone mineral density in adult survivors of solid pediatric cancers. J Pediatr Hematol Oncol 27:248–253
Kelly KM, Thornton JC, Hughes D et al (2009) Total body bone measurements: a cross-sectional study in children with acute lymphoblastic leukemia during the following completion of therapy. Pediatr Blood Canc 52:33–38
van der Sluis IM, van den Heuvel-Eibrink MM, Hählen K, Krenning EP, de Muinck Keizer-Schrama SM (2000) Bone mineral density, body composition, and height in long-term survivors of acute lymphoblastic leukemia in childhood. Med Pediatr Oncol 35:415–420
Cicognani A, Pasini A, Pession A et al (2003) Gonadal function and pubertal development after treatment of a childhood malignancy. J Pediatr Endocrinol Metab 16:321–326
Chemaitilly W, Mertens AC, Mitby P et al (2006) Acute ovarian failure in the childhood cancer survivor study. J Clin Endocrinol Metab 91:1723–1728
Arikoski P, Komulainen J, Riikonen P, Voutilainen R, Knip M, Kroger H (1999) Alterations in bone turnover and impaired development of bone mineral density in newly diagnosed children with cancer: a 1 year prospective study. J Clin Endocrinol Metab 84:3174–3181
Arikoski P, Komulainen J, Riikonen P et al (1999) Impaired development of BMD during chemotherapy: a prospective analysis of 46 children newly diagnosed with Cancer. J Bone Miner Res 14:2002–2009
Marinovic D, Dorgeret S, Lescoeur B et al (2005) Improvement in bone mineral density and body composition in survivors of childhood acute lymphoblastic leukemia: a 1-year prospective study. Pediatrics 116:e102–e108
Pui CH, Campana D, Pei D et al (2009) Treating acute lymphoblastic leukemia without cranial irradiation. N Engl J Med 360:2730–2741
Tanner JM (1978) Physical growth and development. In: Forfar JO, Arneil GC, eds. Textbook of Pediatrics, 2nd Ed. Vol. 1 Edinburgh: Churchill Livingstone pp.249–303
Salamoun MM, Kizirian AS, Tannous RI et al (2005) Low calcium and vitamin D intake in healthy children and adolescents and their correlates. Eur J Clin Nutr 59:177–184
Fleming KH, Heimbach JT (1994) Consumption of calcium in the US: food sources and intake levels. J Nutr 124:1426S–1430S
Gordon CM, Bachrach LK, Carpenter TO et al (2008) Dual energy X-ray absorptiometry interpretation and reporting in children and adolescents: the 2007 ISCD Pediatric Official Positions. J Clin Densitom 11:43–58
Athanassiadou F, Tragiannidis A, Rousso I et al (2005) Evaluation of bone metabolism in children with acute lymphoblastic leukemia after induction chemotherapy treatment. Pediatr Hematol Oncol 22:285–289
Rai SN, Hudson MM, McCammon E et al (2008) Implementing an intervention to improve bone mineral density in survivors of childhood acute lymphoblastic leukemia: BONEII, a prospective placebo-controlled double blind randomized interventional longitudinal study design. Contemp Clin Trials 29:711–719
Reis JP, von Muhlen D, Kritz-Silverstein D, Wingard DL, Barrett-Connor E (2007) Vitamin D, parathyroid hormone levels and the metabolic syndrome in community-dwelling older adults. Diabetes Care 30:1549–1555
Parikh SJ, Edelman M, Uwaifo GI et al (2004) The relationship between obesity and serum 1, 25 dihydroxy vitamin D concentrations in healthy adults. J Clin Endocrinol Metab 89:1196–1199
Zhao LJ, Jiang H, Papasian CJ et al (2008) Correlation of obesity and osteoporosis: effect of fat mass on the determination of osteoporosis. J Bone Miner Res 23:17–29
Strauss AJ, Su JT, Dalton VM, Gelber RD, Sallan SE, Silverman LB (2001) Bony morbidity in children treated for acute lymphoblastic leukemia. J Clin Oncol 19:3066–3072
Acknowledgments
We would like to thank the children and their parents for study participation and acknowledge Ms Randa Shahine for assistance in study progress, Ms Samia Mroueh for BMD analyses, and Ms Carmen Hajj-Chahine for the hormonal assays. This study was supported by an investigator-initiated grant funded by Novartis Pharmaceuticals.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Appendix I
Appendix I
Hormonal assays
Serum 25-OHD was measured by a competitive protein-binding assay, RIA (radioimmunoassay) with inter- and intra-assay CV (coefficient of variation) between 5% and 8.2% for values between 15.6 and 60.5 ng/ml (IDS, Immuno-Diagnostic Systems, Boldon, UK), 1,25-(OH)2D by RIA with inter- and intra-assay CV between 9.3% and 13.6% for values between 8.6 and 56.8 pg/ml, serum PTH with ELSA-PTH, IRMA (immunoradiometric assay) with inter-and intra-assay CV <7% for values between 6 and 887 pg/ml (CIS Bio International, Gif-sur-Yvette, France), serum C-TX by ECLIA (electrochemiluminescence immunoassay) (Elecsys) with inter- and intra-assay CV between 1% and 5.5% for values between 140 and 359 pg/ml (Roche Diagnostics), serum OC by IRMA (immunoradiometric assay) (CIS Bio International, Gif-Sur-Yvette, France), with inter- and intra-assay CV between 1.2% and 5.2% for values between 20.4 and 220 ng/ml, TSH by ECLIA (Elecsys) with inter- and intra-assay CV between 4.3% and 5.3% for values between 0.2 and 7.9 μU/ml, FT4 by ECLIA (Elecsys) with inter- and intra-assay CV between 2.77% and 4.08% for values between 1 and 3.2 ng/dl, testosterone by RIA (CIS Bio International, Gif-Sur-Yvette, France), with inter- and intra-assay CV between 3.8% and 7.5% for values between 46 and 763 ng/dl, estradiol by IRMA with inter- and intra-assay CV between 3.5% and 4.9% for values between 347 and 2,609 pg/ml (CIS Bio International, Gif-Sur-Yvette, France), IGF1 by IRMA with inter-and intra-assay CV between 3.2% and 5.9% at values between 39.1 and 509 ng/ml (CIS Bio International, Gif-Sur-Yvette, France).
Rights and permissions
About this article
Cite this article
El-Hajj Fuleihan, G., Muwakkit, S., Arabi, A. et al. Predictors of bone loss in childhood hematologic malignancies: a prospective study. Osteoporos Int 23, 665–674 (2012). https://doi.org/10.1007/s00198-011-1605-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-011-1605-2