Abstract
Summary
Meaured spinal kyphosis, as a predictor of prevalent and incident vertebral deformity, was examined in older women (>70 years) and found to not have sufficient sensitivity or specificity to justify its use as a predictor of present or future vertebral deformity risk.
Introduction
Kyphosis may be attributable to vertebral deformity and was investigated as a clinical tool for predicting the presence and future risk of vertebral deformity.
Methods
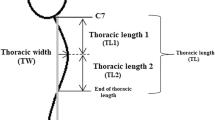
Kyphosis was measured in 434 women aged 70 years or older and the kyphosis index (KI) calculated. Prevalent and incident vertebral deformities were assessed by morphometric X-ray absorptiometry (MXA). The predictive value of KI was examined.
Results
Severity of kyphosis was categorised by tertile of KI; 65% of anterior thoracic deformities occurred in the 33% of subjects in the highest (most kyphotic) tertile. Using this tertile as a predictor of anterior thoracic deformity, the probability for a positive test rose from 14% for the whole population to 28% and for a negative test the probability fell to 8%. For any spinal deformity the highest tertile of KI increased the probability of a positive test from 34% to 42% and reduced the probability for a negative test to 30%. The incidence of new deformities was 6% over 4 years; a high KI tertile did not increase the probability of any vertebral deformity.
Conclusions
Severe kyphosis does not increase the probability of detection of a prevalent or incident spinal deformity sufficiently to make it a useful method of selecting patients for further evaluation of spinal deformity.




Similar content being viewed by others
References
Riggs BL, Melton LJ 3rd (1986) Involutional osteoporosis. N Engl J Med 314:1676–1686
Hall SE, Criddle RA, Comito TL, Prince RL (1999) A case-control study of quality of life and funcational impairment in women with long-standing vertebral osteoporotic fracture. Osteoporosis Int 9:508–515
Kado DM, Browner WS, Palermo L, Nevitt MC, Genant HK, Cummings SR (1999) Vertebral fractures and mortality in older women: a prospective study. Study of Osteoporotic Fractures Research Group. Arch Intern Med 159:1215–1220
Cooper C, Atkinson EJ, Jacobsen SJ, O’Fallon WM, Melton LJ 3rd (1993) Population-based study of survival after osteoporotic fractures. Am J Epidemiol 137:1001–1005
Center JR, Nguyen TV, Schneider D, Sambrook PN, Eisman JA (1999) Mortality after all major types of osteoporotic fracture in men and women: an observational study. Lancet 353:878–882
Doherty DA, Sanders KM, Kotowicz MA, Prince RL (2001) Lifetime and five-year age-specific risks of first and subsequent osteoporotic fractures in postmenopausal women. Osteoporos Int 12:16–23
Sornay-Rendu E, Munoz F, Garnero P, Duboeuf F, Delmas PD (2005) Identification of osteopenic women at high risk of fracture: the OFELY study. J Bone Miner Res 20:1813–1819
Kaptoge S, Armbrecht G, Felsenberg D, Lunt M, Weber K, Boonen S, Jajic I, Stepan JJ, Banzer D, Reisinger W, Janott J, Kragl G, Scheidt-Nave C, Felsch B, Matthis C, Raspe HH, Lyritis G, Poor G, Nuti R, Miazgowski T, Hoszowski K, Armas JB, Vaz AL, Benevolenskaya LI, Masaryk P, Cannata JB, Johnell O, Reid DM, Bhalla A, Woolf AD, Todd CJ, Cooper C, Eastell R, Kanis JA, O’Neill TW, Silman AJ, Reeve J (2006) Whom to treat? The contribution of vertebral X-rays to risk-based algorithms for fracture prediction. Results from the European Prospective Osteoporosis Study. Osteoporos Int 17:1369–1381
Holmberg AH, Johnell O, Nilsson PM, Nilsson J, Berglund G, Akesson K (2006) Risk factors for fragility fracture in middle age. A prospective population-based study of 33,000 men and women. Osteoporos Int 17:1065–1077
Huang MH, Barrett-Connor E, Greendale GA, Kado DM (2006) Hyperkyphotic posture and risk of future osteoporotic fractures: the Rancho Bernardo study. J Bone Miner Res 21:419–423
Ferrar L, Jiang G, Barrington NA, Eastell R (2000) Identification of vertebral deformities in women: comparison of radiological assessment and quantitative morphometry using morphometric radiography and morphometric X-ray absorptiometry. J Bone Miner Res 15:575–585
Rea JA, Chen MB, Li J, Blake GM, Steiger P, Genant HK, Fogelman I (2000) Morphometric X-ray absorptiometry and morphometric radiography of the spine: a comparison of prevalent vertebral deformity identification. J Bone Miner Res 15:564–574
Ross PD (1997) Clinical consequences of vertebral fractures. Am J Med 103:30S–42S; discussion 42S–43S
Edmond SL, Kiel DP, Samelson EJ, Kelly-Hayes M, Felson DT (2005) Vertebral deformity, back symptoms, and functional limitations among older women: the Framingham Study. Osteoporos Int 16:1086–1095
Crans GG, Genant HK, Krege JH (2005) Prognostic utility of a semiquantitative spinal deformity index. Bone 37:175–179
Milne JS, Lauder IJ (1976) The relationship of kyphosis to the shape of vertebral bodies. Ann Hum Biol 3:173–179
Lundon KM, Li AM, Bibershtein S (1998) Interrater and intrarater reliability in the measurement of kyphosis in postmenopausal women with osteoporosis. Spine 23:1978–1985
Bruce DG, Devine A, Prince RL (2002) Recreational physical activity levels in healthy older women: the importance of fear of falling. J Am Geriatr Soc 50:84–89
Ettinger B, Black DM, Palermo L, Nevitt MC, Melnikoff S, Cummings SR (1994) Kyphosis in older women and its relation to back pain, disability and osteopenia: the study of osteoporotic fractures. Osteoporos Int 4:55–60
McCloskey EV, Spector TD, Eyres KS, Fern ED, O’Rourke N, Vasikaran S, Kanis JA (1993) The assessment of vertebral deformity: a method for use in population studies and clinical trials. Osteoporos Int 3:138–147
Eastell R, Cedel SL, Wahner HW, Riggs BL, Melton LJ 3rd (1991) Classification of vertebral fractures. J Bone Miner Res 6:207–215
Melton LJ, Kan SH, Frye MA, Wahner HW, O’Fallon WM, Riggs BL (1989) Epidemiology of vertebral fractures in women. Am J Epidemiol 129:1000–1011
Edmondston SJ, Price RI, Valente B, Singer P (1999) Measurement of vertebral body heights: ex vivo comparisons between morphometric X-ray absorptiometry, morphometric radiography and direct measurements. Osteoporos Int 10:7–13
Melton LJ, Lane AW, Cooper C, Eastell R, O’Fallon WM, Riggs BL (1993) Prevalence and incidence of vertebral deformities. Osteoporosis Int 3:113–119
Acknowledgments
Prof. K. Singer suggested the use of the flexible rule to measure kyphosis. This study was supported by research grants from the Healthway Health Promotion Foundation of Western Australia, the Australasian Menopause Society and the National Health and Medical Research Council of Australia (project grant 254627).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Prince, R.L., Devine, A. & Dick, I.M. The clinical utility of measured kyphosis as a predictor of the presence of vertebral deformities. Osteoporos Int 18, 621–627 (2007). https://doi.org/10.1007/s00198-006-0289-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-006-0289-5