Abstract
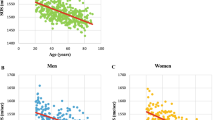
Fifty-one patients with surgically proven primary hyperparathyroidism (PHPT), 11 males and 40 females, mean age±SD: 55.9±14.1 years, and 58 age- and sex-matched normal subjects were studied. The femoral and L2–L4 bone mineral density (BMD; Hologic QDR 4500 C), as well as quantitative ultrasonometry (QUS; DBM-Sonic 1200) of the phalanges of both hands were measured in patients and controls. QUS measurements included amplitude-dependent speed of sound (AD-SoS), and other parameters derived from the graphic trace: signal dynamics (Sdy), first wave amplitude (FWA), bone transmission time (BTT) and ultrasound bone profile index (UBPI). Patients with PHPT showed significantly lower dual energy X-ray densitometry (DXA) values and QUS parameters compared to controls (lumbar spine Z-score: controls: −0.16±1.12, PHPT: −0.70±1.14, P=0.016 ; femoral neck Z-score: controls: −0.28±1.74, PHPT: −1±1.01, P=0.013 ; total femur Z-score: controls: −0.33±1.12, PHPT: −1.01±0.95, P=0.0013; AD-SoS Z-score: controls: −0.89±1.22, PHPT: −1.97±1.78, P=0.0003; FWA Z-score: controls: 0.36±1, PHPT: 0.62±0.85, P<0.0001; BTT Z-score: controls: 0.04±1.03, PHPT: −0.45±1.37, P=0.044; UBPI Z-score: controls: −0.02±1.01, PHPT: −0.68±1.05, P=0.002; SDy (mV/μs2): controls: −295±256, PHPT: −498±306, P=0.0003). In male patients, BMD values measured on the lumbar spine and femoral regions were similar to those found in male controls, while QUS values were significantly lower (lumbar spine Z-score: controls: −1.05±1.41, PHPT: −1.75±1.21, P=0.21; femoral neck Z-score: controls: −0.37±1.84, PHPT: −1.11±1.14, P=0.27; total femur Z-score: controls: −0.16±1.59, PHPT: −1.02±1.20, P=0.168; AD-SoS Z-score: controls: −0.52±1.58, PHPT: −1.57±1.77, P=0.149; FWA Z-score: controls: 0.67±1.01, PHPT: −0.74±0.79, P=0.0016; BTT Z-score: controls: 1.22±0.83, PHPT: 0.75±1.51, P=0.478; UBPI Z-score: controls: 0.56±0.94, PHPT: −0.47±1.10, P=0.025; SDy (mV/μs2): controls: −167±230, PHPT: −485±307, P=0.01). Women with PHPT were further divided into two subgroups: premenopause (n=11) and postmenopause (n=29). The premenopausal women with PHPT showed significantly lower DXA values than those of the premenopausal control ones, but similar QUS parameters (lumbar spine Z-score: controls: 0.12±0.66, PHPT: −0.59±0.85, P=0.03; femoral neck Z-score: controls: 0.06±2.85, PHPT: −1.48±1.05, P=0.11; total femur Z-score: controls: −0.51±0.97, PHPT: −1.48±0.63, P=0.009; AD-SoS Z-score: controls: 0.78±0.89, PHPT: −1.26±1.88, P=0.42; FWA Z-score: controls: 1.14±0.77, PHPT: 0.12±0.80, P=0.007; BTT Z-score: controls: 0.13±0.60, PHPT: 0.25±1.15, P=0.757; UBPI Z-score: controls: 0.73±0.49, PHPT: 0.24±0.96, P=0.15; SDy (mV/μs2): controls: −118±123, PHPT: −271±301, P=0.106). The postmenopausal women with PHPT showed both DXA and QUS parameters significantly lower than those found in the postmenopausal controls (lumbar spine Z-score: controls: 0.09±0.96, PHPT: −0.31±0.96, P=0.004; femoral neck Z-score: controls: −0.38±1.01, PHPT: −0.76±0.91, P=0.14; total femur Z-score: controls: −0.33±0.97, PHPT: −0.81±0.92, P=0.057; AD-SoS Z-score: controls: −1.08±1.17, PHPT: −2.38±1.68, P=0.31; FWA Z-score: controls: −0.013±0.81, PHPT: −0.86±0.74, P=0.0009; BTT Z-score: controls: −0.58±0.68, PHPT: −1.13±0.93, P=0.016; UBPI Z-score: controls: −0.62±0.83, PHPT: −1.11±0.82, P=0.034; SDy (mV/μs2): controls: −419±242, PHPT: -589±269, P=0.012). The relative risk of osteopenia was significantly increased in PHPT patients at several measurement sites. There was a highly significant correlation between spine and femoral BMD and QUS parameters, while PTH serum levels did not correlate with any of the densitometric variables. In conclusion, QUS parameters would seem to be able to distinguish patients with PHPT from normal controls in male subjects and in postmenopausal women, but not in premenopausal women. This would suggest that the higher estrogen levels in premenopausal patients might preserve the bone from significant structural changes. This may also suggest that hyperparathyroidism, in addition to the reduction of bone mineral content, can cause an alteration of bone structure with an additional increase in fracture risk in postmenopausal women. Furthermore, the alterations in QUS parameters in patients who do not show significant changes in DXA measurements suggest an involvement of bone that is independent of mineral content and may be helpful for selecting candidates for surgery, according to NIH criteria.

Similar content being viewed by others
References
Christiansen P (2001) The skeleton in primary hyperparathyroidism: a review focusing on bone remodeling, structure, mass, and fracture. APMIS Suppl 102:1–52
Chappard C, Houillier P, Paillard M (2001) Bone status in primary hyperparathyroidism. Joint Bone Spine 68:112–119
Syed Z, Khan A (2000) Skeletal effects of primary hyperparathyroidism. Endocr Pract 6:385–388
Kosowicz J, Baszko-Blaszyk D, Horst-Sikorska W, Baumann-Antczak A (1999) [Bone mineral density in primary hyperparathyroidism]. Pol Arch Med Wewn 101:131–138
Dempster DW, Parisien M, Silverberg SJ et al. (1999) On the mechanism of cancellous bone preservation in postmenopausal women with mild primary hyperparathyroidism. J Clin Endocrinol Metab 84:1562–1566
Mazzuoli GF, D'Erasmo E, Pisani D (1998) Primary hyperparathyroidism and osteoporosis. Aging (Milano) 10:225–231
Boechat MI, Westra SJ, Van Dop C, Kaufman F, Gilsanz V, Roe TF (1996) Decreased cortical and increased cancellous bone in two children with primary hyperparathyroidism. Metabolism 45:76–81
Vogel M, Hahn M, Delling G (1995) Trabecular bone structure in patients with primary hyperparathyroidism. Virchows Arch 426:127–134
NIH Consensus Development Panel on Osteoporosis Prevention, Diagnosis, and Therapy (2001) Osteoporosis prevention, diagnosis, and therapy. JAMA 285:785–795
Wuster C, Heilmann P, Pereira-Lima J, Schlegel J, Anstatt K, Soballa T (1998) Quantitative ultrasonometry (QUS) for the evaluation of osteoporosis risk: reference data for various measurement sites, limitations and application possibilities. Exp Clin Endocrinol Diabetes 106:277–288
Wuster C (1998) [Measuring bone density with ultrasound—ready for general practice?]. Zentralbl Gynakol 120:257–261
Morita R, Yamamoto I, Takada M et al. (1998) [Recent development and clinical application of bone mineral measurements]. Nippon Rinsho 56:1458–1463
Dubois EF, van den Bergh JP, Smals AG, van de Meerendonk CW, Zwinderman AH, Schweitzer DH (2001) Comparison of quantitative ultrasound parameters with dual energy X-ray absorptiometry in pre- and postmenopausal women. Neth J Med 58:62–70
van Rijn RR, van dS, I, Lequin MH et al. (2000) Tibial quantitative ultrasound versus whole-body and lumbar spine DXA in a Dutch paediatric and adolescent population. Invest Radiol 35:548–552
He YQ, Fan B, Hans D et al. (2000) Assessment of a new quantitative ultrasound calcaneus measurement: precision and discrimination of hip fractures in elderly women compared with dual X-ray absorptiometry. Osteoporos Int 11:354–360
Knapp KM, Blake GM, Spector TD, Fogelman I (2001) Multisite quantitative ultrasound: precision, age- and menopause-related changes, fracture discrimination, and T-score equivalence with dual-energy X-ray absorptiometry. Osteoporosis Int 12:456–464
Nicholson PH, Muller R, Cheng XG et al. (2001) Quantitative ultrasound and trabecular architecture in the human calcaneus. J Bone Miner Res 16:1886–1892
Njeh CF, Fuerst T, Diessel E, Genant HK (2001) Is quantitative ultrasound dependent on bone structure? A reflection. Osteoporos Int 12:1–15
Karlsson MK, Duan Y, Ahlborg H, Obrant KJ, Johnell O, Seeman E (2001) Age, gender, and fragility fractures are associated with differences in quantitative ultrasound independent of bone mineral density. Bone 28:118–122
van den Bergh JP, van Lenthe GH, Hermus AR, Corstens FH, Smals AG, Huiskes R (2000) Speed of sound reflects Young's modulus as assessed by microstructural finite element analysis. Bone 26:519–524
Hans D, Wu C, Njeh CF et al. (1999) Ultrasound velocity of trabecular cubes reflects mainly bone density and elasticity. Calcif Tissue Int 64:18–23
Peel NFA, Spittlehouse AJ, Bax DE, Eastell R (1994) Bone mineral density of the hand in rheumatoid arthritis. Arthr Rheum 37:983–991
Wuster C, Albanese C, De Aloysio D et al. (2000) Phalangeal osteosonogrammetry study: age-related changes, diagnostic sensitivity, and discrimination power. The Phalangeal Osteosonogrammetry Study Group. J Bone Miner Res 15:1603–1614
Khan A, Bilezikian J (2000) Primary hyperparathyroidism: pathophysiology and impact on bone. CMAJ 163:184–187
Uchiyama T, Tanizawa T, Ito A, Endo N, Takahashi HE (1999) Microstructure of the trabecula and cortex of iliac bone in primary hyperparathyroidism patients determined using histomorphometry and node-strut analysis. J Bone Miner Metab 17:283–288
Duan Y, De L, V, Seeman E (1999) Parathyroid hormone deficiency and excess: similar effects on trabecular bone but differing effects on cortical bone. J Clin Endocrinol Metab 84:718–722
Dobnig H, Turner RT (1997) The effects of programmed administration of human parathyroid hormone fragment (1–34) on bone histomorphometry and serum chemistry in rats. Endocrinology 138:4607–4612
van Doorn L, Lips P, Netelenbos JC, Hackeng WH (1993) Bone histomorphometry and serum concentrations of intact parathyroid hormone (PTH(1–84)) in patients with primary hyperparathyroidism. Bone Miner 23:233–242
Gonnelli S, Montagnani A, Cepollaro C et al. (2000) Quantitative ultrasound and bone mineral density in patients with primary hyperparathyroidism before and after surgical treatment. Osteoporos Int 11:255–260
Cortet B, Cortet C, Blanckaert F et al. (2000) Bone ultrasonometry and turnover markers in primary hyperparathyroidism. Calcif Tissue Int 66:11–15
Minisola S, Rosso R, Scarda A, Pacitti MT, Romagnoli E, Mazzuoli G (1995) Quantitative ultrasound assessment of bone in patients with primary hyperparathyroidism. Calcif Tissue Int 56:526–528
NIH (1990) Diagnosis and management of asymptomatic primary hyperparathyroidism. NIH Consensus Statement 8:1–18
Gambacciani M, Genazzani AR (2001) Hormone replacement therapy: the benefits in tailoring the regimen and dose. Maturitas 40:195–201
Delmas PD (1999) HRT in the prevention and treatment of osteoporosis. J Epidemiol Biostat 14:155–160
Riggs BL, Melton LJ III (2002) Bone turnover matters: the raloxifene treatment paradox of dramatic decreases in vertebral fractures without commensurate increases in bone density. J Bone Miner Res 7:11–14
Weigel RJ (2001) Nonoperative management of hyperparathyroidism: present and future. Curr Opin Oncol 13:33–38
Orr-Walker BJ, Evans MC, Clearwater JM, Horne A, Grey AB, Reid IR (2000) Effects of hormone replacement therapy on bone mineral density in postmenopausal women with primary hyperparathyroidism: four-year follow- up and comparison with healthy postmenopausal women. Arch Int Med 160:2161–2166
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Camozzi, V., Lumachi, F., Mantero, F. et al. Phalangeal quantitative ultrasound technology and dual energy X-ray densitometry in patients with primary hyperparathyroidism: influence of sex and menopausal status. Osteoporos Int 14, 602–608 (2003). https://doi.org/10.1007/s00198-003-1407-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-003-1407-2