Abstract
Introduction and Hypothesis
Continuation of using a pessary for the treatment of pelvic organ prolapse (POP) is important for improving symptoms but the data on long-term compliance is very limited. Therefore, we conducted this study aimed at evaluating the compliance of patients in the long-term use of a pessary.
Methods
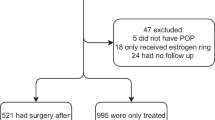
The medical records of women with symptomatic POP were retrospectively reviewed to recruit cases opting for pessary use. The inclusion criteria were women who had a successful pessary fitting and completed at least 5 years of follow-up. Exclusion criteria were pregnancy, death during the follow-up period, and loss to follow-up. Demographic data, pelvic organ prolapse stage, associated symptoms, type and size of pessary, and reason for discontinuation were reviewed.
Results
A total of 261 patients opted for pessary use. Of them, 88.9% (231 out of 261) were successful in initial pessary fitting and 54 were excluded for various reasons. The remaining 178 patients were available for analysis. The continuation rate of self-care pessary at the 5-year follow-up was 53.93% (96). The discontinuation rate was 46.07% (82). The main reasons for discontinuation were desire for surgery (39.1%) and discomfort (31.7%). The highest rate of discontinuation (46.63%) was found in the 1st year of follow-up. The significant risk factors of discontinuation included digitation symptoms on univariate analysis and prior hysterectomy on multivariate analysis, with an odds ratio (95% CI) of 5.98 (1.56–22.88).
Conclusions
Among Thai women, the adherence to self-care pessary in symptomatic pelvic organ prolapse at the 5-year follow-up was 53.93%. The main reason for discontinuation was a prior hysterectomy.


Similar content being viewed by others
Data Availability
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
References
Hendrix SL, Clark A, Nygaard I, Aragaki A, Barnabei V, McTiernan A. Pelvic organ prolapse in the Women’s Health Initiative: gravity and gravidity. Am J Obstet Gynecol. 2002;186(6):1160–6. https://doi.org/10.1067/mob.2002.123819.
Pelvic Organ Prolapse: ACOG Practice Bulletin, Number 214. Obstet Gynecol. 2019;134(5):e126–42. https://doi.org/10.1097/AOG.0000000000003519.
Zeiger BB, da Silva CS, Del Roy CA, da Silva TT, Hwang SM, Auge APF. Vaginal pessary in advanced pelvic organ prolapse: impact on quality of life. Int Urogynecol J. 2022;33(7):2013–20. https://doi.org/10.1007/s00192-021-05002-7.
Aimjirakul K, Pumtako M, Manonai J. Quality of life after treatment for pelvic organ prolapse: vaginal pessary versus surgery. Int J Womens Health. 2023;15:1017–25. https://doi.org/10.2147/IJWH.S406048.
Sansone S, Sze C, Eidelberg A, et al. Role of pessaries in the treatment of pelvic organ prolapse: a systematic review and meta-analysis. Obstet Gynecol. 2022;140(4):613–22. https://doi.org/10.1097/AOG.0000000000004931.
Chien CW, Lo TS, Tseng LH, Lin YH, Hsieh WC, Lee SJ. Long-term outcomes of self-management Gellhorn pessary for symptomatic pelvic organ prolapse. Female Pelvic Med Reconstr Surg. 2020;26(11):e47–53. https://doi.org/10.1097/SPV.0000000000000770.
Koch M, Carlin G, Lange S, Umek W, Krall C, Bodner-Adler B. Long-term adherence to pessary use in women with pelvic organ prolapse: a retrospective cohort study. Maturitas. 2023;178:107828. https://doi.org/10.1016/j.maturitas.2023.107828.
Manchana T. Long-term continuations rate of ring pessary use for symptomatic pelvic organ prolapse. Arch Gynecol Obstet. 2024. https://doi.org/10.1007/s00404-023-07299-9.
Van der Vaart LR, Vollebregt A, Milani AL, et al. Effect of pessary vs surgery on patient-reported improvement in patients with symptomatic pelvic organ prolapse: a randomized clinical trial. JAMA. 2022;328(23):2312–23. https://doi.org/10.1001/jama.2022.22385.
Hagen S, Kearney R, Goodman K, et al. Clinical effectiveness of vaginal pessary self-management vs clinic-based care for pelvic organ prolapse (TOPSY): a randomised controlled superiority trial. EClinicalMedicine. 2023;66:102326. https://doi.org/10.1016/j.eclinm.2023.102326.
Stairs J, Gujral P, Ehlebracht A, van Diepen A, Clancy AA. Women’s attitudes towards pessary self-care: a qualitative study. Int Urogynecol J. 2023;34(8):1899–906. https://doi.org/10.1007/s00192-023-05472-x.
Brown CA, Pradhan A, Pandeva I. Current trends in pessary management of vaginal prolapse: a multidisciplinary survey of UK practice. Int Urogynecol J. 2021;32(4):1015–22. https://doi.org/10.1007/s00192-020-04537-5.
Harvey MA, Lemieux MC, Robert M, Schulz JA. Guideline No. 411: vaginal pessary use. J Obstet Gynaecol Can. 2021;43(2):255–66.e1. https://doi.org/10.1016/j.jogc.2020.11.013.
Geoffrion R, Zhang T, Lee T, Cundiff GW. Clinical characteristics associated with unsuccessful pessary fitting outcomes. Female Pelvic Med Reconstr Surg. 2013;19(6):339–45. https://doi.org/10.1097/SPV.0b013e3182a26174.
Niigaki DI, Silva RSP, Bortolini MAT, Fitz FF, Castro RA. Predictors for long-term adherence to vaginal pessary in pelvic organ prolapse: a prospective study. Int Urogynecol J. 2022;33(11):3237–46. https://doi.org/10.1007/s00192-022-05133-5.
Hsieh MF, Tsai HW, Liou WS, et al. Long-term compliance of vaginal pessaries: does stress urinary incontinence matter? Medicine (Baltimore). 2019;98(14):e15063. https://doi.org/10.1097/MD.0000000000015063.
Author information
Authors and Affiliations
Contributions
N.C.: project development, data collection, manuscript writing/editing; S.S.: project development, data collection, data analysis, manuscript writing/editing; C.P.: project development, manuscript writing/editing; T.T.: data analysis, manuscript writing/editing; Y.R.: data collection.
Corresponding author
Ethics declarations
Conflicts of Interest
None.
Additional information
Handling Editor: Rufus Cartwright
Editor in Chief: Maria A. Bortolini
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Charoenloet, N., Srisukho, S., Phongnarisorn, C. et al. Long-Term Compliance of Self-Care Pessary in Symptomatic Pelvic Organ Prolapse. Int Urogynecol J (2024). https://doi.org/10.1007/s00192-024-05806-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00192-024-05806-3