Abstract
Introduction and hypothesis
The objective was to investigate the effects of spinal stabilization exercises (SSEs) focusing on the pelvic floor with regard to urinary symptoms, pelvic floor muscle strength (PFMS), core stability, quality of life (QoL), and perception of subjective improvement (PSI) in women with overactive bladder (OAB).
Methods
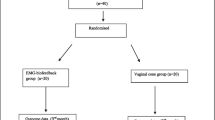
Patients were randomly divided into SSE (n=23) and control (n=24) groups. The SSE group received SSEs focusing on the pelvic floor for 3 days a week for 8 weeks and recommendation. The control group received only recommendation. Before (BT) and after treatment (AT), urinary symptoms were evaluated with Overactive Bladder Questionnaire-Version 8 (OAB-V8) and bladder diary. PFMS, core stability, and QoL were assessed using the Modified Oxford Scale (MOS), Sharman test, and King’s Health Questionnaire (KHQ) respectively. AT, PSI with a Likert-type scale, and compliance with recommendations using a visual analog scale were assessed.
Results
The OAB-V8 and the KHQ scores, the number of voids per day and voids per night decreased and the MOS and the Sharman scores increased in the SSE group (p<0.05). In the control group, the OAB-V8 and incontinence effect, social limitations, emotional state, and sleep sub-dimension scores related to KHQ decreased (p<0.05). The OAB-V8, role and physical limitations, emotional state, and sleep sub-dimension scores decreased more, and the MOS, the Sharman, the PSI, and the compliance with recommendations scores increased more in the SSE group than in the control group (p<0.05).
Conclusions
The SSEs focusing on the pelvic floor improved urinary symptoms, PFMS, core stability, QoL, and PSI. This exercise approach may be beneficial in the management of OAB.


Similar content being viewed by others
References
Haylen BT, de Ridder D, Freeman RM, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn. 2010;29:4–20. https://doi.org/10.1002/nau.20798.
Chuang YC, Liu SP, Lee KS, et al. Prevalence of overactive bladder in China, Taiwan and South Korea: results from a cross-sectional, population-based study. Low Urin Tract Symptoms. 2019;11:48–55. https://doi.org/10.1111/luts.12193.
Coyne KS, Sexton CC, Irwin DE, et al. The impact of overactive bladder, incontinence and other lower urinary tract symptoms on quality of life, work productivity, sexuality and emotional well-being in men and women: results from the EPIC study. BJU Int. 2008;101:1388–95.
Peyronnet B, Mironska E, Chapple C, et al. A comprehensive review of overactive bladder pathophysiology: on the way to tailored treatment. Eur Urol. 2019;75:988–1000. https://doi.org/10.1016/j.eururo.2019.02.038.
Shafik A, Shafik IA. Overactive bladder inhibition in response to pelvic floor muscle exercises. World J Urol. 2003;20:374–7. https://doi.org/10.1007/s00345-002-0309-9.
Çelenay ŞT, Karaaslan Y, Oskay K, et al. The relationship between pelvic floor muscle strength and bladder symptom severity and anxiety level in women with overactive bladder. TÜSBAD. 2018;1:1–7.
Panjabi MM. The stabilizing system of the spine. Part I. Function, dysfunction, adaptation, and enhancement. J Spinal Disord. 1992;5(4):383–9. https://doi.org/10.1097/00002517-199212000-00001.
Ashton-Miller JA, DeLancey JO. Functional anatomy of the female pelvic floor. Ann N Y Acad Sci. 2007;1101:266–96. https://doi.org/10.1196/annals.1389.034.
Prather H, Dugan S, Fitzgerald C, et al. Review of anatomy, evaluation, and treatment of musculoskeletal pelvic floor pain in women. PM R. 2009;1(4):346–58. https://doi.org/10.1016/j.pmrj.2009.01.003.
Nitti VW, Patel A, Karram M. Diagnosis and management of overactive bladder: a review. J Obstet Gynaecol Res. 2021;47(5):1654–65. https://doi.org/10.1111/jog.14708.
Burgio KL. Update on behavioral and physical therapies for incontinence and overactive bladder: the role of pelvic floor muscle training. Curr Urol Rep. 2013;14(5):457–64. https://doi.org/10.1007/s11934-013-0358-1.
Wang XQ, Zheng JJ, Yu ZW, et al. A meta-analysis of core stability exercise versus general exercise for chronic low back pain. PLoS One. 2012;7(12):e52082. https://doi.org/10.1371/journal.pone.0052082.
Nwodo OD, Ibikunle PO, Ogbonna NL, et al. Review of core stability exercise versus conventional exercise in the management of chronic low back pain. Afr Health Sci. 2022;22(4):148–67. https://doi.org/10.4314/ahs.v22i4.19.
Akuthota V, Ferreiro A, Moore T, et al. Core stability exercise principles. Curr Sports Med Rep. 2008;7:39–44. https://doi.org/10.1097/01.CSMR.0000308663.
Yu CY, Yu TY, Chen YW, et al. Core stabilization exercise in prenatal and postnatal women with urinary incontinence: a systematic review and meta-analysis of randomized controlled trials. Am J Phys Med Rehabil. 2023; https://doi.org/10.1097/PHM.0000000000002260.
Ghaderi F, Mohammadi K, Sasan RA, et al. Effects of stabilization exercises focusing on pelvic floor muscles on low back pain and urinary incontinence in women. Urology. 2016;93:50–4. https://doi.org/10.1016/j.urology.2016.03.034.
Khorasani F, Ghaderi F, Bastani P, et al. The effects of home-based stabilization exercises focusing on the pelvic floor on postnatal stress urinary incontinence and low back pain: a randomized controlled trial. Int Urogynecol J. 2020;31:2301–7. https://doi.org/10.1007/s00192-020-04284-7.
Nipa SI, Sriboonreung T, Paungmali A, et al. The effects of pelvic floor muscle exercise combined with core stability exercise on women with stress urinary incontinence following the treatment of nonspecific chronic low back pain. Adv Urol. 2022;2022:2051374. https://doi.org/10.1155/2022/2051374.
Kavalci Kol B, Oskay K, Toprak Celenay S. Comparison of lumbopelvic stability, low back pain and well-being of women who have overactive bladder syndrome to asymptomatic controls: cut-off points. Somatosens Mot Res. 2021;38(4):259–66. https://doi.org/10.1080/08990220.2021.
Tarcan T, Mangır N, Özgür MÖ, et al. OAB-V8 Aşırı aktif mesane sorgulama formu validasyon çalışması. Üroloji Bülteni. 2012;21:113–6.
Bright E, Cotterill N, Drake M, et al. Developing and validating the international consultation on incontinence questionnaire bladder diary. Eur Urol. 2014;66(2):294–300. https://doi.org/10.1016/j.eururo.2014.02.057.
Laycock J, Jerwood D. Pelvic floor muscle assessment: the PERFECT scheme. Physiotherapy. 2001;87:631–42. https://doi.org/10.1016/S0031-9406(05)61108-X.
Stanton R, Reaburn PR, Humphries B. The effect of short-term Swiss ball training on core stability and running economy. J Strength Cond Res. 2004;18(3):522–8. https://doi.org/10.1519/1533-4287(2004)18<522:TEOSSB>2.0.CO;2.
Kaya S, Akbayrak T, Celenay ST, et al. Reliability and validity of the Turkish King’s Health Questionnaire in women with urinary incontinence. Int Urogynecol J. 2015;12:1853–9. https://doi.org/10.1007/s00192-015-2786-6.
Korkut Z, Turen Demir E, Toprak Celenay S. Effects of interferential current stimulation in women with pelvic organ prolapse: a prospective randomized sham-controlled study. Int Urogynecol J. 2023;34:279–89.
Toprak Celenay S, Ozer Kaya D. Effects of spinal stabilization exercises in women with benign joint hypermobility syndrome: a randomized controlled trial. Rheumatol Int. 2017;37(9):1461–8. https://doi.org/10.1007/s00296-017-3713-6.
De Souza Abreu N, de Castro Villas Boas B, Netto JMB, et al. Dynamic lumbopelvic stabilization for treatment of stress urinary incontinence in women: controlled and randomized clinical trial. Neurourol Urodyn. 2017;36(8):2160–8. https://doi.org/10.1002/nau.23261.
Vesentini G, El Dib R, Righesso LAR, et al. Pelvic floor and abdominal muscle cocontraction in women with and without pelvic floor dysfunction: a systematic review and meta-analysis. Clinics (Sao Paulo). 2019;74:e1319. https://doi.org/10.6061/clinics/2019/e1319.
Hall AM, Ferreira PH, Maher CG, et al. The influence of the therapist-patient relationship on treatment outcome in physical rehabilitation: a systematic review. Phys Ther. 2010;90(8):1099–110. https://doi.org/10.2522/ptj.20090245.
Acknowledgement
The authors thank Melike Mese Buran for taking the exercise pictures.
Author information
Authors and Affiliations
Contributions
S. Toprak Celenay: project development, data collection, data analysis and interpretation, and manuscript writing/editing; Z. Korkut: data collection, data analysis and interpretation, and manuscript writing/editing; S.B. Bulbul: data collection, data analysis and interpretation, and manuscript writing/editing, H. Altay: data collection, data analysis and interpretation, and manuscript writing/editing; K. Oskay: data collection, and manuscript writing/editing.
Corresponding author
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Celenay, S.T., Korkut, Z., Bulbul, S.B. et al. Effects of spinal stabilization exercises focusing on the pelvic floor in women with overactive bladder. Int Urogynecol J 34, 2959–2967 (2023). https://doi.org/10.1007/s00192-023-05638-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-023-05638-7