Abstract
Introduction and hypothesis
Anterior sacrospinous hysteropexy (SSH) was popularized by transvaginal mesh kits. Following mesh-kit market withdrawal, we hypothesized similar efficacy through native-tissue reattachment of the pubocervical fascia with fixation of the anterior cervix to the sacrospinous ligament. Few analyses for anterior native-tissue versus mesh-augmented SSH exist.
Methods
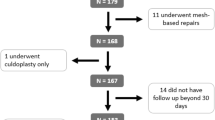
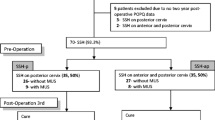
A retrospective analysis of women who underwent transvaginal anterior SSH between 01 January 2016 and 31 December 2022 was performed. Women who underwent a mesh-augmented (Uphold Lite Vaginal Support System™) versus native-tissue repair were compared. Composite success was defined as no bulge symptoms, no retreatment, and no recurrence beyond the hymen with apex nondescended > one third of the total vaginal length. Descriptive and bivariate statistics were obtained as indicated.
Results
Of 223 women screened, inclusion criteria were met by 124 (40 mesh-augmented; 84 native-tissue). There was no difference in pre-operative characteristics between groups. Composite success was demonstrated in 95.2% of women with a median follow-up of 224 days (range: 30–988). Two women in the mesh-augmented group reported bulge symptoms and underwent re-treatment with a pessary. Four women in the native-tissue group reported bulge symptoms; 3 underwent re-treatment (2 pessary, 1 surgery). There were no differences in composite success rates between groups (p=0.954). There were additionally no differences in intra-operative (p=0.752) or post-operative (p=0.292) complication rates between the groups. There were no mesh-related complications, including exposure or chronic pelvic pain.
Conclusions
Ninety-five percent of women achieved surgical success and the use of mesh augmentation did not confer added benefit in terms of efficacy or complications when compared with native tissue. Further long-term data are needed to continue our assessment of native-tissue anterior SSH.

Similar content being viewed by others
References
Hefni M, El-Toukhy T, Bhaumik J, Katsimanis E. Sacrospinous cervicocolpopexy with uterine conservation for uterovaginal prolapse in elderly women: an evolving concept. Am J Obstet Gynecol. 2003;188(3):645–50.
van Brummen HJ, van de Pol G, Aalders CI, Heintz AP, van der Vaart CH. Sacrospinous hysteropexy compared to vaginal hysterectomy as primary surgical treatment for a descensus uteri: effects on urinary symptoms. Int Urogynecol J Pelvic Floor Dysfunct. 2003;14(5):350–5.
Dietz V, van der Vaart CH, van der Graaf Y, Heintz P, Schraffordt Koops SE. One-year follow-up after sacrospinous hysteropexy and vaginal hysterectomy for uterine descent: a randomized study. Int Urogynecol J. 2010;21(2):209–16.
Al-Badr A, Perveen K, Al-Shaikh G. Evaluation of sacrospinous hysteropexy vs. uterosacral suspension for the treatment of uterine prolapse: a retrospective assessment. Low Urin Tract Symptoms. 2017;9(1):33–7.
Husby KR, Larsen MD, Lose G, Klarskov N. Surgical treatment of primary uterine prolapse: a comparison of vaginal native tissue surgical techniques. Int Urogynecol J. 2019;30(11):1887–93.
Maher C, Feiner B, Baessler K, Schmid C. Surgical management of pelvic organ prolapse in women. Cochrane Database Syst Rev. 2013;2013(4):CD004014.
Bradley S, Gutman RE, Richter LA. Hysteropexy: an option for the repair of pelvic organ prolapse. Curr Urol Rep. 2018;19(2):15.
Nager CW, Visco AG, Richter HE, et al. Effect of vaginal mesh hysteropexy vs vaginal hysterectomy with uterosacral ligament suspension on treatment failure in women with uterovaginal prolapse: a randomized clinical trial. JAMA. 2019;322(11):1054–65.
Gutman RE, Rardin CR, Sokol ER, et al. Vaginal and laparoscopic mesh hysteropexy for uterovaginal prolapse: a parallel cohort study. Am J Obstet Gynecol. 2017;216(1):38.e1–11.
Nager CW. Database updates and resulting changes in data in study of vaginal mesh hysteropexy vs vaginal hysterectomy. JAMA. 2021;325(7):695–6.
Theofanides MC, Onyeji I, Matulay J, Sui W, James M, Chung DE. Safety of mesh for vaginal cystocele repair: analysis of national patient characteristics and complications. J Urol. 2017;198(3):632–7.
Bowen ST, Abramowitch SD, Lockhart M, et al. Vaginal angulation after vaginal hysterectomy with uterosacral ligament suspension or vaginal mesh hysteropexy: investigating the role of vaginal configuration in anatomic failure of apical prolapse repair. Female Pelvic Med Reconstr Surg. 2020;26(10S):S4–5.
Plair A, Dutta R, Overholt TL, Matthews C. Short-term outcomes of sacrospinous hysteropexy through an anterior approach. Int Urogynecol J. 2021;32(6):1555–63.
Rosenthal R, Hoffman H, Clavien PA, Bucher HC, Dell-Kuster S. Definition and classification of intraoperative complications (CLASSIC): Delphi study and pilot evaluation. World J Surg. 2015;39(7):1663–71.
Clavien PA, Barkun J, Oliveira ML, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250(2):187–96.
Jirschele K, Seitz M, Zhou Y, Rosenblatt P, Culligan P, Sand P. A multicenter, prospective trial to evaluate mesh-augmented sacrospinous hysteropexy for uterovaginal prolapse. Int Urogynecol J. 2015;26(5):743–8.
Vu MK, Letko J, Jirschele K, et al. Minimal mesh repair for apical and anterior prolapse: initial anatomical and subjective outcomes. Int Urogynecol J. 2012;23(12):1753–61.
Detollenaere RJ, Boon J, Stekelenberg J, et al. Sacrospinous hysteropexy versus vaginal hysterectomy with suspension of the uterosacral ligaments in women with uterine prolapse stage 2 or higher: multicentre randomised non-inferiority trial. BMJ. 2015;351:h3717.
Lo TS, Pue LB, Hung TH, Wu PY, Tan YL. Long-term outcome of native tissue reconstructive vaginal surgery for advanced pelvic organ prolapse at 86 months: hysterectomy versus hysteropexy. J Obstet Gynaecol Res. 2015;41(7):1099–107.
Kapoor S, Sivanesan K, Robertson JA, Veerasingham M, Kapoor V. Sacrospinous hysteropexy: review and meta-analysis of outcomes. Int Urogynecol J. 2017;28(9):1285–94.
Hoke TP, Tan-Kim J, Richter HE. Evidence-based review of vaginal native tissue hysteropexy for uterovaginal prolapse. Obstet Gynecol Surv. 2019;74(7):429–35.
Funding
No funding was obtained or utilized for the completion of this study.
Author information
Authors and Affiliations
Contributions
T.L. Overholt: project development, data collection, statistical analysis, manuscript writing; L. Velet: project development, data collection, manuscript writing; M. Xu: data collection, manuscript writing; R. Dutta: project development, manuscript editing; C.A. Matthews: project development, manuscript editing.
Corresponding author
Ethics declarations
Conflicts of interest and disclosures
There are no conflicts of interest or disclosures regarding the completion of this study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Overholt, T.L., Velet, L., Xu, M. et al. Anterior approach sacrospinous hysteropexy: native tissue compared with mesh-augmented repair for primary uterovaginal prolapse management. Int Urogynecol J 34, 2603–2609 (2023). https://doi.org/10.1007/s00192-023-05589-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-023-05589-z