Abstract
Introduction and hypothesis
The objective was to evaluate the efficacy and safety of vaginal electrical stimulation (VES) as an alternative or adjunct treatment for overactive bladder (OAB) syndrome in women.
Methods
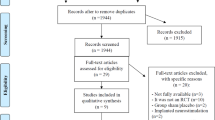
Five English-language databases and four Chinese-language databases were searched to identify relevant studies. Studies comparing VES (VES alone or VES plus other interventions) with other interventions (medicines, bladder training, or PFMT) were included. Voiding diary, quality of life (QoL), and adverse events were extracted from the included studies for comparison.
Results
Seven trials with 601 patients in total were reviewed. The results showed that when compared with other interventions, VES alone significantly improved urgency episodes (p = 0.0008) and voiding frequency (p = 0.01), but did not significantly reduce nocturia (p = 0.85), urinary incontinence episodes (p = 0.90) and number of pads (p = 0.87). When VES plus other interventions was compared with other interventions, the former significantly improved voiding frequency (p < 0.00001), nocturia (p < 0.00001), and number of pads (p = 0.03), but it did not significantly reduce urinary incontinence episodes (p = 0.24). Both VES alone (p < 0.00001) and VES plus other interventions (p = 0.003) showed significant benefit on QoL.
Conclusions
This study demonstrated that VES alone decreased urgency episodes and QoL better than other therapies. Although VES alone reduced voiding frequency better and VES plus other therapies decreased nocturia, number of pads, urgency episodes, and QoL better than other therapies, the results should be interpreted with caution for clinical practice because some of the RCTs included were of low quality and because of the small number of studies included.




Similar content being viewed by others
References
Haylen BT, de Ridder D, Freeman RM, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J. 2010;21(1):5–26.
Abrams P, Andersson KE, Birder L, et al. Fourth International Consultation on Incontinence Recommendations of the International Scientific Committee: evaluation and treatment of urinary incontinence, pelvic organ prolapse, and fecal incontinence. Neurourol Urodyn. 2010;29(1):213–40.
Coyne KS, Sexton CC, Kopp ZS, Ebel-Bitoun C, Milsom I, Chapple C. The impact of overactive bladder on mental health, work productivity and health-related quality of life in the UK and Sweden: results from EpiLUTS. BJU Int. 2011;108(9):1459–71.
Milsom I, Kaplan SA, Coyne KS, Sexton CC, Kopp ZS. Effect of bothersome overactive bladder symptoms on health-related quality of life, anxiety, depression, and treatment seeking in the United States: results from EpiLUTS. Urology. 2012;80(1):90–6.
Milsom I, Abrams P, Cardozo L, Roberts RG, Thuroff J, Wein AJ. How widespread are the symptoms of an overactive bladder and how are they managed? A population-based prevalence study. BJU Int. 2001;87(9):760–6.
Abrams P, Kelleher CJ, Kerr LA, Rogers RG. Overactive bladder significantly affects quality of life. Am J Manag Care. 2000;6(11 Suppl):S580–90.
Scarneciu I, Lupu S, Bratu OG, et al. Overactive bladder: a review and update. Exp Ther Med. 2021;22(6):1444.
Chen LC, Kuo HC. Pathophysiology of refractory overactive bladder. Low Urin Tract Symptoms. 2019;11(4):177–81.
D'Souza AO, Smith MJ, Miller LA, Doyle J, Ariely R. Persistence, adherence, and switch rates among extended-release and immediate-release overactive bladder medications in a regional managed care plan. J Manag Care Pharm. 2008;14(3):291–301.
Suehs BT, Caplan EO, Hayden J, Ng DB, Gaddy RR. The relationship between anticholinergic exposure and falls, fractures, and mortality in patients with overactive bladder. Drugs Aging. 2019;36(10):957–67.
Gormley EA, Lightner DJ, Faraday M, Vasavada SP. Diagnosis and treatment of overactive bladder (non-neurogenic) in adults: AUA/SUFU guideline amendment. J Urol. 2015;193(5):1572–80.
Stewart F, Gameiro LF, El DR, Gameiro MO, Kapoor A, Amaro JL. Electrical stimulation with non-implanted electrodes for overactive bladder in adults. Cochrane Database Syst Rev. 2016;12(12):D10098.
Lightner DJ, Gomelsky A, Souter L, Vasavada SP. Diagnosis and treatment of overactive bladder (non-neurogenic) in adults: AUA/SUFU guideline amendment 2019. J Urol. 2019;202(3):558–63.
Gupta P, Ehlert MJ, Sirls LT, Peters KM. Percutaneous tibial nerve stimulation and sacral neuromodulation: an update. Curr Urol Rep. 2015;16(2):4.
Meng L, Tian Z, Zhang Y, et al. Sacral neuromodulation for overactive bladder using the InterStim and BetterStim systems. Sci Rep. 2022;12(1):22299.
Chene G, Mansoor A, Jacquetin B, et al. Female urinary incontinence and intravaginal electrical stimulation: an observational prospective study. Eur J Obstet Gynecol Reprod Biol. 2013;170(1):275–80.
Messelink EJ. The overactive bladder and the role of the pelvic floor muscles. BJU Int. 1999;83(Suppl 2):31–5.
Firinci S, Yildiz N, Alkan H, Aybek Z. Which combination is most effective in women with idiopathic overactive bladder, including bladder training, biofeedback, and electrical stimulation? A prospective randomized controlled trial. Neurourol Urodyn. 2020;39(8):2498–508.
Ozdedeli S, Karapolat H, Akkoc Y. Comparison of intravaginal electrical stimulation and trospium hydrochloride in women with overactive bladder syndrome: a randomized controlled study. Clin Rehabil. 2010;24(4):342–51.
Shamseer L, Moher D, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ. 2015;350:g7647.
Guyatt GH, Oxman AD, Vist GE, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336(7650):924–6.
Luo D, Wan X, Liu J, Tong T. Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range. Stat Methods Med Res. 2018;27(6):1785–805.
Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014;14:135.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–60.
Wetterslev J, Jakobsen JC, Gluud C. Trial sequential analysis in systematic reviews with meta-analysis. BMC Med Res Methodol. 2017;17(1):39.
Casans-Frances R, Roberto-Alcacer AT, Gomez-Rios MA, Calvo-Vecino JM. The importance of trial sequential analysis in the evaluation of the results of a meta-analysis. Minerva Anestesiol. 2019;85(4):342–3.
Yildiz N, Alkan H, Sarsan A. Efficacy of intravaginal electrical stimulation added to bladder training in women with idiopathic overactive bladder: a prospective randomized controlled trial. Int Braz J Urol. 2021;47(6):1150–9.
Abdelbary AM, El-Dessoukey AA, Massoud AM, et al. Combined vaginal pelvic floor electrical stimulation (PFS) and local vaginal estrogen for treatment of overactive bladder (OAB) in perimenopausal females. Randomized Controlled Trial (RCT). Urology. 2015;86(3):482–6.
Wang AC, Chen MC, Kuo WY, Lin YH, Wang YC, Lo TS. Urgency-free time interval as primary endpoint for evaluating the outcome of a randomized OAB treatment. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20(7):819–25.
Arruda RM, Castro RA, Sousa GC, Sartori MG, Baracat EC, Girao MJ. Prospective randomized comparison of oxybutynin, functional electrostimulation, and pelvic floor training for treatment of detrusor overactivity in women. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19(8):1055–61.
Wang AC, Chih SY, Chen MC. Comparison of electric stimulation and oxybutynin chloride in management of overactive bladder with special reference to urinary urgency: a randomized placebo-controlled trial. Urology. 2006;68(5):999–1004.
Vrijens D, Marcelissen T, Drossaerts J, et al. Self-consciousness/awareness and bladder sensations: comparative study of overactive bladder patients and healthy volunteers. Low Urin Tract Symptoms. 2019;11(1):3–7.
Herrewegh A, Vrijens D, Marcelissen T, van Koeveringe GA. Bladder sensations in male and female overactive bladder patients compared to healthy volunteers: a sensation-related bladder diary evaluation. Scand J Urol. 2019;53(4):255–60.
Chapple C. Pathophysiology of the lower urinary tract and CNS. Can Urol Assoc J. 2011;5(5 Suppl 2):S126–7.
La Rosa VL, Platania A, Ciebiera M, et al. A comparison of sacral neuromodulation vs. transvaginal electrical stimulation for the treatment of refractory overactive bladder: the impact on quality of life, body image, sexual function, and emotional well-being. Prz Menopauzalny. 2019;18(2):89–93.
Bacchi AGF, Milhem HJ, Souza DCFH, Chada BE, Casarotto RA, Alves GFE. Is the addition of vaginal electrical stimulation to transcutaneous tibial nerve electrical stimulation more effective for overactive bladder treatment? A randomized controlled trial. Actas Urol Esp (Engl Ed). 2021;45(1):64–72.
Wang AC, Wang YY, Chen MC. Single-blind, randomized trial of pelvic floor muscle training, biofeedback-assisted pelvic floor muscle training, and electrical stimulation in the management of overactive bladder. Urology. 2004;63(1):61–6.
Bhide AA, Tailor V, Fernando R, Khullar V, Digesu GA. Posterior tibial nerve stimulation for overactive bladder-techniques and efficacy. Int Urogynecol J. 2020;31(5):865–70.
Burgio KL, Kraus SR, Johnson TN, et al. Effectiveness of combined behavioral and drug therapy for overactive bladder symptoms in men: a randomized clinical trial. JAMA Intern Med. 2020;180(3):411–9.
Burgio KL, Goode PS, Locher JL, et al. Behavioral training with and without biofeedback in the treatment of urge incontinence in older women: a randomized controlled trial. JAMA. 2002;288(18):2293–9.
Madhuvrata P, Cody JD, Ellis G, Herbison GP, Hay-Smith EJ. Which anticholinergic drug for overactive bladder symptoms in adults. Cochrane Database Syst Rev. 2012;1:D5429.
Leron E, Weintraub AY, Mastrolia SA, Schwarzman P. Overactive bladder syndrome: evaluation and management. Curr Urol. 2018;11(3):117–25.
Wang Y, Shi C, Wang J, Shi G. Efficacy of Yun-type pelvic floor optimal training therapy and PFMT on middle aged women with mild to moderate overactive bladder: a randomized controlled trial. Ann Transl Med. 2022;10(14):796.
Wadensten T, Nystrom E, Franzen K, Lindam A, Wasteson E, Samuelsson E. A mobile app for self-management of urgency and mixed urinary incontinence in women: randomized controlled trial. J Med Internet Res. 2021;23(4):e19439.
Scaldazza CV, Morosetti C, Giampieretti R, Lorenzetti R, Baroni M. Percutaneous tibial nerve stimulation versus electrical stimulation with pelvic floor muscle training for overactive bladder syndrome in women: results of a randomized controlled study. Int Braz J Urol. 2017;43(1):121–6.
Yildiz N, Ozlu A. Factors predicting the treatment success of bladder training for urgency urinary incontinence. Neurourol Urodyn. 2022;41(8):1809–16.
Vouri SM, Kebodeaux CD, Stranges PM, Teshome BF. Adverse events and treatment discontinuations of antimuscarinics for the treatment of overactive bladder in older adults: a systematic review and meta-analysis. Arch Gerontol Geriatr. 2017;69:77–96.
Booth J, Connelly L, Dickson S, Duncan F, Lawrence M. The effectiveness of transcutaneous tibial nerve stimulation (TTNS) for adults with overactive bladder syndrome: a systematic review. Neurourol Urodyn. 2018;37(2):528–41.
Bartoli S, Aguzzi G, Tarricone R. Impact on quality of life of urinary incontinence and overactive bladder: a systematic literature review. Urology. 2010;75(3):491–500.
Coyne KS, Sexton CC, Irwin DE, Kopp ZS, Kelleher CJ, Milsom I. The impact of overactive bladder, incontinence and other lower urinary tract symptoms on quality of life, work productivity, sexuality and emotional well-being in men and women: results from the EPIC study. BJU Int. 2008;101(11):1388–95.
Funding
The research reported in this publication was supported by the Guangdong Provincial Department of Education Guangdong University Research Platform and Project (No. 2019KZDZX1041), Guangdong Basic and Applied Basic Research Fund Committee, Regional Joint Fund-Key Project (2019B1515120040), Guangdong Provincial Bureau of Traditional Chinese Medicine project (No. 20211171), Guangdong Provincial Bureau of Traditional Chinese Medicine project (No. 20215004), and Guangdong Hospital of Traditional Chinese Medicine Academic School inheritance Studio construction project (No. [2013]233).
Author information
Authors and Affiliations
Contributions
X.Z.: conceptualization and methodology; D.W. and Q.D.: data curation and statistical analysis; J.H. and Y.F.: writing the original draft preparation; J.Y.: writing, reviewing, and provided funding for editorial support. All authors contributed to the article.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOCX 1567 kb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Huang, J., Fan, Y., Wang, D. et al. Efficacy and safety of vaginal electrical stimulation as an alternative or adjunct treatment for overactive bladder syndrome in women: a meta-analysis of randomized controlled trials. Int Urogynecol J 34, 2345–2357 (2023). https://doi.org/10.1007/s00192-023-05546-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-023-05546-w