Abstract
Introduction and hypothesis
Both urogynecologic surgeries and transdermal scopolamine (TDS) patches are independently associated with postoperative urinary retention (POUR). It is unclear if the risk of POUR increases when these interventions are used in combination. This systematic review and meta-analysis aim to synthesize current evidence to optimize clinical management and outcomes for patients undergoing urogynecologic procedures.
Methods
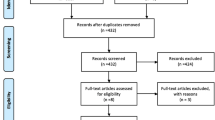
This systematic review was conducted in concordance with the PRISMA 2020 guidelines. MEDLINE, ClinicalTrials.gov, and Cochrane Library were searched. Publications were filtered by inclusion and exclusion criteria. Inclusion criteria required: (1) preoperative or perioperative application of TDS, (2) surgery indicated for stress urinary incontinence and/or pelvic organ prolapse, (3) results given for postoperative voiding trials, and (4) were available in English. Exclusion criteria included: (1) oral or parenteral formulations of scopolamine, (2) administration of alternative preoperative antiemetics, and (3) use of combination antiemetic therapy. Quality was assessed using the Joanna Briggs Institute Checklist. Publication bias was evaluated via the ROBINS-I assessment tool, and Egger regression and Begg and Mazumumdar rank correlation tests. A meta-analysis was conducted using Meta-Essentials Excel Workbook.
Results
Four publications were identified which complied with inclusion and exclusion criteria. Included studies comprised 752 patients (237 experimental group, 515 control group). All were retrospective cohort studies conducted via chart review in America. Meta-analysis revealed a risk ratio (RR) of 2.35 with a confidence interval (CI) of 0.61 to 9.07, indicating a positive association between TDS and POUR, but without statistical significance.
Conclusions
Current evidence suggests that TDS application may be associated with increased risk of POUR following urogynecologic procedures. While research on this topic is greatly limited, this systematic review and meta-analysis highlights that alternative antiemetic therapy may be necessary for patients undergoing such interventions in effort to limit the risk of POUR.

Similar content being viewed by others
References
Wu JM, Gandhi MP, Shah AD, Shah JY, Fulton RG, Weidner AC. Trends in inpatient urinary incontinence surgery in the USA, 1998–2007. Int Urogynecol J. 2011;22(11):1437–43.
Fialkow MF, Newton KM, Lentz GM, Weiss NS. Lifetime risk of surgical management for pelvic organ prolapse or urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19(3):437–40.
Shah AD, Kohli N, Rajan SS, Hoyte L. The age distribution, rates, and types of surgery for pelvic organ prolapse in the USA. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19(3):421–8.
Barr SA, Thomas A, Potter S, Melick CF, Gavard JA, McLennan MT. Incidence of successful voiding and predictors of early voiding dysfunction after retropubic sling. Int Urogynecol J. 2016;27(8):1209–14.
Geller EJ. Prevention and management of postoperative urinary retention after urogynecologic surgery. Int J Womens Health. 2014;6:829–38.
Geller EJ. Prevention and management of postoperative urinary retention after urogynecologic surgery. Int J Womens Health. 2014;6:829–38. https://doi.org/10.2147/IJWH.S55383.
Kobak WH, Walters MD, Piedmonte MR. Determinants of voiding after three types of incontinence surgery: a multivariable analysis. Obstet Gynecol. 2001;97(1):86–91.
Foster RT Sr, Borawski KM, South MM, Weidner AC, Webster GD, Amundsen CL. A randomized, controlled trial evaluating 2 techniques of postoperative bladder testing after transvaginal surgery. Am J Obstet Gynecol. 2007;197(627):e1–e4.
Li ALK, Zajichek A, Kattan MW, Ji XK, Lo KA, Lee PE. Nomogram to predict risk of postoperative urinary retention in women undergoing pelvic reconstructive surgery. J Obstet Gynaecol Can. 2020;42(10):1203–10. https://doi.org/10.1016/j.jogc.2020.03.021.
Baldini G, Bagry H, Aprikian A, Carli F. Postoperative urinary retention: anesthetic and perioperative considerations. Anesthesiology. 2009;110(5):1139–57. https://doi.org/10.1097/ALN.0b013e31819f7aea.
Walter PJ, Dieter AA, Siddiqui NY, Weidner AC, Wu JM. Perioperative anticholinergic medications and risk of catheterization after urogynecologic surgery. Female Pelvic Med Reconstr Surg. 2014;20(3):163–7.
Wohlrab KJ, Erekson EA, Korbly NB, Drimbarean CD, Rardin CR, Sung VW. The association between regional anesthesia and acute postoperative urinary retention in women undergoing outpatient midurethral sling procedures. Am J Obstet Gynecol. 2009;200(5):571.e1–571.e5. https://doi.org/10.1016/j.ajog.2008.11.021.
Maheshwari D, Sierra T, Leung K, Hall C, Flynn M. Effect of pudendal blockade on bladder emptying after midurethral sling: a randomized controlled trial. Female Pelvic Med Reconstr Surg. 2021;27(2):e465–8. https://doi.org/10.1097/SPV.0000000000000963.
Wald HL, Ma A, Bratzler DW, Kramer AM. Indwelling urinary catheter use in the postoperative period: analysis of the national surgical infection prevention project data. Arch Surg. 2008;143(6):551–7.
Mueller ER, Brubaker L, Eckler K. Postoperative urinary retention in women. UpToDate (Wolkers Kluwer). 2021. https://www.uptodate.com/contents/postoperativeurinary-retention-in-women. Accessed on 8 Dec 2022.
Gan TJ, Diemunsch P, Habib AS, et al. Consensus guidelines for the management of postoperative nausea and vomiting [published correction appears in Anesth Analg. 2014 Mar;118(3):689] [published correction appears in Anesth Analg. 2015 Feb;120(2):494]. Anesth Analg. 2014;118(1):85–113. https://doi.org/10.1213/ANE.0000000000000002.
Shaikh SI, Nagarekha D, Hegade G, Marutheesh M. Postoperative nausea and vomiting: a simple yet complex problem. Anesth Essays Res. 2016;10(3):388–96. https://doi.org/10.4103/0259-1162.179310.
Apfel CC, Zhang K, George E, et al. Transdermal scopolamine for the prevention of postoperative nausea and vomiting: a systematic review and meta-analysis [published correction appears in Clin Ther. 2010 Dec;32(14):2502]. Clin Ther. 2010;32(12):1987–2002. https://doi.org/10.1016/j.clinthera.2010.11.014.
Einarsson JI, Audbergsson BO, Thorsteinsson A. Scopolamine for prevention of postoperative nausea in gynecologic laparoscopy, a randomized trial. J Minim Invasive Gynecol. 2008;15(1):26–31. https://doi.org/10.1016/j.jmig.2007.08.616.
Harnett MJ, O'Rourke N, Walsh M, Carabuena JM, Segal S. Transdermal scopolamine for prevention of intrathecal morphine-induced nausea and vomiting after cesarean delivery. Anesth Analg. 2007;105(3):764–9. https://doi.org/10.1213/01.ane.0000277494.30502.db.
Gan TJ, Belani KG, Bergese S, et al. Fourth consensus guidelines for the management of postoperative nausea and vomiting [published correction appears in Anesth Analg. 2020 Nov;131(5):e241]. Anesth Analg. 2020;131(2):411–48. https://doi.org/10.1213/ANE.0000000000004833.
Apfel CC, Zhang K, George E, Shi S, Jalota L, Hornuss C, Fero KE, Heidrich F, Pergolizzi JV, Cakmakkaya OS, Kranke P. Transdermal scopolamine for the prevention of postoperative nausea and vomiting: a systematic review and meta-analysis. Clin Ther. 2010;32(12):1987–2002. https://doi.org/10.1016/j.clinthera.2010.11.014.
Antor MA, Uribe AA, Erminy-Falcon N, Werner JG, Candiotti KA, Pergolizzi JV, Bergese SD. The effect of transdermal scopolamine for the prevention of postoperative nausea and vomiting. Front Pharmacol. 2014;5:1–8.
Kassel L, Nelson M, Shine J, Jones LR, Kassel C. Scopolamine use in the perioperative patient: a systematic review. AORN J. 2018;108(3):287–95. https://doi.org/10.1002/aorn.12336.
Bowman JJ, Edwards CC 2nd, Dean C, Park J, Edwards CC Sr. Incidence and risk factors for postoperative urinary retention following lumbar spine fusion. Clin Spine Surg. 2021;34(7):E397–402. https://doi.org/10.1097/BSD.0000000000001202.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. https://doi.org/10.1126/bmjn71.
Aromataris E, Fernandez R, Godfrey C, Holly C, Kahlil H, Tungpunkom P. Summarizing systematic reviews: methodological development, conduct and reporting of an Umbrella review approach. Int J Evid Based Healthc. 2015;13(3):132–40.
Sterne JA, Hernán MA, Reeves BC, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919. https://doi.org/10.1136/bmj.i4919.
Dessie SG, Hacker MR, Apostolis C, Boundy EO, Modest AM, Jones SM, Rosenblatt PL. Effect of scopolamine patch use on postoperative voiding function after transobturator slings. Female Pelvic Med Reconstr Surg. 2016;22(3):136–9.
Katz EG, Stensland KD, Alazem K, MacLachlan LS. The role of perioperative medications in urinary retention following midurethral sling. Neurourol Urodyn. 2020;39(8):2455–62.
Propst K, O’Sullivan DM, Tulikangas PK. Transdermal scopolamine and acute postoperative urinary retention in pelvic reconstructive surgery. Female Pelvic Med Reconstr Surg. 2016;22(5):328–31.
Courtepatte A, Kelly M, Minassian VA. The effect of preoperative scopolamine patch use on postoperative urinary retention in urogynecologic surgeries. Int Urogynecol J. 2022. https://doi.org/10.1007/s00192-022-05165-x. Advance online publication.
Suurmond R, van Rhee H, Hak T. Introduction, comparison and validation of meta-essentials: a free and simple tool for meta-analysis. Res Synth Methods. 2017;8(4):537–53.
Meta-Essentials: workbooks for meta-analysis. Erasmus Research Institute of Management. n.d. https://www.erim.eur.nl/research-support/meta-essentials/.
Author information
Authors and Affiliations
Contributions
Nick W. Lanpher participated in (a) analysis and interpretation of the data, (b) drafting the article and revising it critically for important intellectual content, and (c) approves of the final version. Emma M. Schnittka participated in (a) conception and design, analysis and interpretation of the data, (b) drafting the article, and (c) approval of the final version. All authors have participated in (a) conception and design, (b) revising the manuscript for important intellectual content, and (c) approval of the final version.
Corresponding author
Ethics declarations
Conflicts of Interest
None.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
PROSPERO Registration ID
CRD42022354877.
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lanpher, N.W., Schnittka, E.M. & Haggag, A. Transdermal scopolamine and urinary retention following urogynecologic surgery: a systematic review and meta-analysis. Int Urogynecol J 34, 1689–1696 (2023). https://doi.org/10.1007/s00192-023-05467-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-023-05467-8