Abstract
Introduction and hypothesis
The aim of this study was to compare the surgical results and the complications of absorbable suture (AS) versus permanent suture (PS) in sacrocolpopexy (SCP).
Methods
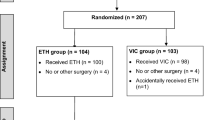
We systematically searched PubMed, Embase, ClinicalTrials.gov, and the Cochrane Library Central Register of Controlled Trials for articles in which researchers compared AS with PS in SCP. The primary outcomes were the surgical success rate and suture-related complications (suture exposure/erosion, mesh erosion, and suture removal). All analyses were performed with Review Manager 5.3.
Results
Four articles involving 689 patients were ultimately included. Our findings demonstrated that AS had similar surgical success rates to those of PS (OR=1.34; 95% CI, 0.60–2.96) and no significant differences in failure rates were noted between the two groups (OR=0.75; 95% CI, 0.34–1.66). Subgroup analyses in patients with anatomical failure revealed no significant differences in recurrent posterior prolapse (OR=0.33; 95% CI, 0.05–2.10) or in recurrent apical (OR=0.64; 95% CI, 0.03–13.66) or anterior prolapse (OR=0.45; 95% CI, 0.13–1.57). However, the AS group were at a lower risk of suture exposure/erosion (OR=0.18; 95% CI, 0.06–0.58) and a lower suture removal rate (OR=0.14; 95% CI, 0.03–0.61) and retreatment (OR=0.36; 95% CI, 0.16–0.82), but the mesh erosion was not significantly different (OR=1.00; 95% CI, 0.49–2.08).
Conclusions
The data showed that AS had a similar success rate, less exposure/erosion, and were less likely to be removed and require retreatment than PS, which supported the notion that AS is as effective as PS but safer.




Similar content being viewed by others
References
Wu JM, Kawasaki A, Hundley AF, Dieter AA, Myers ER, Sung VW. Predicting the number of women who will undergo incontinence and prolapse surgery, 2010 to 2050. Am J Obstet Gynecol. 2011;205(3):230.e1–5.
Maher C, Feiner B, Baessler K, Schmid C. Surgical management of pelvic organ prolapse in women. Cochrane Database Syst Rev. 2013;(4):CD004014.
Padoa A, Shiber Y, Fligelman T, Tomashev R, Tsviban A, Smorgick N. Advanced cystocele is a risk factor for surgical failure after robotic-assisted laparoscopic sacrocolpopexy. J Minim Invasive Gynecol. 2022;29(3):409–15.
Arthure HG, Savage D. Uterine prolapse and prolapse of the vaginal vault treated by sacral hysteropexy. J Obstet Gynaecol Br Emp. 1957;64(3):355–60.
Geller EJ, Siddiqui NY, Wu JM, Visco AG. Short-term outcomes of robotic sacrocolpopexy compared with abdominal sacrocolpopexy. Obstet Gynecol. 2008;112(6):1201–6.
Nygaard I, Brubaker L, Zyczynski HM, Cundiff G, Richter H, Gantz M, et al. Long-term outcomes following abdominal sacrocolpopexy for pelvic organ prolapse. JAMA. 2013;309(19):2016–24.
Siddiqui NY, Grimes CL, Casiano ER, Abed HT, Jeppson PC, Olivera CK, et al. Mesh sacrocolpopexy compared with native tissue vaginal repair: a systematic review and meta-analysis. Obstet Gynecol. 2015;125(1):44–55.
Marinkovic SP. Will hysterectomy at the time of sacrocolpopexy increase the rate of polypropylene mesh erosion? Int Urogynecol J Pelvic Floor Dysfunct. 2008;19(2):199–203.
Tagliaferri V, Ruggieri S, Taccaliti C, Gentile C, Didonna T, D’Asta M, et al. Comparison of absorbable and permanent sutures for laparoscopic sacrocervicopexy: A randomized controlled trial. Acta Obstet Gynecol Scand. 2021;100(2):347–52.
Bretschneider CE, Kenton K, Geller EJ, Wu JM, Matthews CA. Pain after permanent versus delayed absorbable monofilament suture for vaginal graft attachment during minimally invasive total hysterectomy and sacrocolpopexy. Int Urogynecol J. 2020;31(10):2035–41.
Matthews CA, Geller EJ, Henley BR, Kenton K, Myers EM, Dieter AA, et al. Permanent compared with absorbable suture for vaginal mesh fixation during total hysterectomy and sacrocolpopexy: a randomized controlled trial. Obstet Gynecol. 2020;136(2):355–64.
Tan-Kim J, Menefee SA, Lippmann Q, Lukacz ES, Luber KM, Nager CW. A pilot study comparing anatomic failure after sacrocolpopexy with absorbable or permanent sutures for vaginal mesh attachment. Permanente J. 2014;18(4):40–4.
Powell CR, Tachibana I, Eckrich B, Rothenberg J, Hathaway J. Securing mesh with delayed absorbable suture does not increase risk of prolapse recurrence after robotic sacral colpopexy. J Endourol. 2021;35(6):944–9.
Reisenauer C, Andress J, Schoenfisch B, Huebner M, Brucker SY, Lippkowski A, et al. Absorbable versus non-absorbable sutures for vaginal mesh attachment during sacrocolpopexy: a randomized controlled trial. Int Urogynecol J. 2022;33(2):411–9.
Borahay MA, Oge T, Walsh TM, Patel PR, Rodriguez AM, Kilic GS. Outcomes of robotic sacrocolpopexy using barbed delayed absorbable sutures. J Minim Invasive Gynecol. 2014;21(3):412–6.
Culligan PJ, Murphy M, Blackwell L, Hammons G, Graham C, Heit MH. Long-term success of abdominal sacral colpopexy using synthetic mesh. Am J Obstet Gynecol. 2002;187(6):1473–80; discussion 81–2.
Toglia MR, Fagan MJ. Suture erosion rates and long-term surgical outcomes in patients undergoing sacrospinous ligament suspension with braided polyester suture. Am J Obstet Gynecol. 2008;198(5):600.e1–4.
Maher CF, Feiner B, DeCuyper EM, Nichlos CJ, Hickey KV, O’Rourke P. Laparoscopic sacral colpopexy versus total vaginal mesh for vaginal vault prolapse: a randomized trial. Am J Obstet Gynecol. 2011;204(4):360.e1–7.
Tate SB, Blackwell L, Lorenz DJ, Steptoe MM, Culligan PJ. Randomized trial of fascia lata and polypropylene mesh for abdominal sacrocolpopexy: 5-year follow-up. Int Urogynecol J. 2011;22(2):137–43.
Rondini C, Braun H, Alvarez J, Urzúa MJ, Villegas R, Wenzel C, et al. High uterosacral vault suspension vs sacrocolpopexy for treating apical defects: a randomized controlled trial with twelve months follow-up. Int Urogynecol J. 2015;26(8):1131–8.
Noor N, Bastawros D, Florian-Rodriguez ME, Hobson D, Eto C, Lozo S, et al. Comparing minimally invasive sacrocolpopexy with vaginal uterosacral ligament suspension: a multicenter retrospective cohort study through the Fellows’ Pelvic Research Network. Urogynecology (Hagerstown). 2022;28(10):687–94.
Geller EJ, Bretschneider CE, Wu JM, Kenton K, Matthews CA. Sexual function after minimally invasive total hysterectomy and sacrocolpopexy. J Minim Invasive Gynecol. 2021;28(9):1603–9.
Acknowledgements
This study was supported by the National Key Research and Development Program of China (No. 2021YFC2009100), Natural Science Foundation of China (No.8177063), Huohua Project of Sichuan University (2018), and 1.3.5 project for disciplines of excellence, West China Hospital, Sichuan University (ZY2017310).
Author information
Authors and Affiliations
Contributions
Shuang Chen: conceptualization, methodology, data extraction, data analysis, writing original draft preparation; Yuhao Liu: data extraction, data analysis, writing original draft preparation; Liao Peng: data extraction, data analysis; Yuanzhuo Chen: discussion and data extraction; Hong Shen: discussion and data extraction; Deyi Luo: supervision.
Corresponding author
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chen, S., Liu, Y., Peng, L. et al. Comparative study of absorbable suture and permanent suture in sacrocolpopexy: a meta-analysis and systematic review. Int Urogynecol J 34, 993–1000 (2023). https://doi.org/10.1007/s00192-022-05427-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-022-05427-8