Abstract
Introduction and hypothesis
The objective was to systemically review the current literature on the association of gut, vaginal, and urinary dysbiosis in female patients with overactive bladder (OAB).
Methods
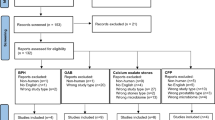
We performed a comprehensive literature search following the Preferred Reporting Items for Systematic Review and Meta-analysis (PRISMA) protocols for systematic reviews. In the EMBASE, CINAHL, and Medline databases, a search was conducted using key words such as “microbiome,” “microbiota,” “microflora,” “overactive bladder,” “urge,” “gut,” “vaginal.” Articles were screened using the online tool www.covidence.org. Two independent reviewers screened studies at each stage and resolved conflicts together. We excluded papers that discussed pediatric patients and animal studies. In total, 13 articles met this criterion, which included 6 abstracts.
Results
After identifying 817 unique references, 13 articles met the criteria for data extraction. Articles were published from 2017 to 2021. No study reported the same microbiota abundance, even in healthy individuals. Overall, there was a loss of bacterial diversity in OAB patients compared with controls. Additionally, the bacterial composition of the controls and OAB patients was not significantly different, especially if the urine was collected midstream. Overall, the composition of the microbiome is dependent on the specimen collection methodology, and the metagenomic sequencing technique utilized. OAB urine microbiome is more predisposed to alteration from the gut or vaginal influences than in controls.
Conclusions
Current evidence suggested a potential relationship among gut, vaginal, and urinary microbiome in OAB patients, but there are very limited studies.

Similar content being viewed by others
Abbreviations
- BPH:
-
Benign prostatic hyperplasia
- DO:
-
Detrusor overactivity
- EQUC:
-
Enhanced quantitative urine culture
- FMT:
-
Fecal microbiota transplantation
- LUTS:
-
Lower urinary tract symptoms
- MSU:
-
Midstream urine
- OAB:
-
Overactive bladder
- SCFAs:
-
Short-chain fatty acids
- TUC:
-
Transurethral catheterized urine
- UUI:
-
Urge urinary incontinence
References
Onukwugha E, Zuckerman IH, McNally D, et al. The total economic burden of overactive bladder in the United States: a disease-specific approach. Am J Manag Care. 2009;15(4 Suppl):S90–7.
Welk B, McArthur E. Increased risk of dementia among patients with overactive bladder treated with an anticholinergic medication compared to a beta-3 agonist: a population-based cohort study. BJU Int. 2020;126:183.
Welk B, Richardson K, Panicker JN. The cognitive effect of anticholinergics for patients with overactive bladder. Nat Rev Urol. 2021;18:686–700.
Peyronnet B, Mironska E, Chapple C, et al. A comprehensive review of overactive bladder pathophysiology: on the way to tailored treatment. Eur Urol. 2019;75:988.
Hilt EE, Mckinley K, Pearce MM, et al. Urine is not sterile: use of enhanced urine culture techniques to detect resident bacterial flora in the adult female bladder. J Clin Microbiol. 2014;52:871.
Curtiss N, Balachandran A, Krska L, et al. A case controlled study examining the bladder microbiome in women with overactive bladder (OAB) and healthy controls. Eur J Obstet Gynecol Reprod Biol. 2017;214:31.
Ouma WZ, Mejia-Guerra MK, Yilmaz A, et al. Important biological information uncovered in previously unaligned reads from chromatin immunoprecipitation experiments (ChIP-Seq). Sci Rep. 2015;5:8635.
Wu P, Chen Y, Zhao J, et al. Urinary microbiome and psychological factors in women with overactive bladder. Front Cell Infect Microbiol. 2017;7:488.
Gill K, Kang R, Sathiananthamoorthy S, et al. A blinded observational cohort study of the microbiological ecology associated with pyuria and overactive bladder symptoms. Int Urogynecol J. 2018;29:1493.
Magruder M, Edusei E, Zhang L, et al. Gut commensal microbiota and decreased risk for Enterobacteriaceae bacteriuria and urinary tract infection. Gut Microbes. 2020;12:1805281.
Okamoto T, Hatakeyama S, Imai A, et al. Altered gut microbiome associated with overactive bladder and daily urinary urgency. World J Urol. 2021;39:847.
Pearce MM, Hilt EE, Rosenfeld AB, et al. The female urinary microbiome: a comparison of women with and without urgency urinary incontinence. mBio. 2014;5:e01283.
Ammitzboll N, Bau BPJ, Bundgaard-Nielsen C, et al. Pre- and postmenopausal women have different core urinary microbiota. Sci Rep. 2021;11:2212.
Price TK, Hilt EE, Thomas-White K, et al. The urobiome of continent adult women: a cross-sectional study. BJOG. 2020;127:193.
Cohn J, Brown ET, Guo Y, et al. MP31-03 the relationship between the urinary microbiome and central sensitization in women with overactive bladder. J Urol. 2017;197:e398.
Carabotti M, Scirocco A, Maselli MA, et al. The gut-brain axis: interactions between enteric microbiota, central and enteric nervous systems. Ann Gastroenterol. 2015;28:203.
Ackerman AL, Tang J, Eilber K, et al. MP82-02 decreased urinary fungal burden and diversity in overactive bladder. J Urol. 2017;197:e1097.
Ackerman AL, Tang J, Eilber K, et al. MP82-18 shared alterations in urinary bacterial communities in patients with interstitial cystitis and overactive bladder. J Urol. 2017;197:e1104.
Pohl HG, Groah SL, Perez-Losada M, et al. The urine microbiome of healthy men and women differs by urine collection method. Int Neurourol J. 2020;24:41.
Dubourg G, Morand A, Mekhalif F, et al. Deciphering the urinary microbiota repertoire by culturomics reveals mostly anaerobic bacteria from the gut. Front Microbiol. 2020;11:513305.
Tan J, McKenzie C, Potamitis M, et al. The role of short-chain fatty acids in health and disease. Adv Immunol. 2014;121:91.
Thomas-White K, Taege S, Limeira R, et al. Vaginal estrogen therapy is associated with increased Lactobacillus in the urine of postmenopausal women with overactive bladder symptoms. Am J Obstet Gynecol. 2020;223:727.e1.
Veit-Rubin N, Mahboobani KS, Cartwright R et al. Relationship between the urinary, urothelial and vaginal microbiome in overactive bladder: https://www.ics.org/2018/abstract/1. Accessed 28 Aug 2021
Morand A, Cornu F, Dufour J-C et al. Human bacterial repertoire of the urinary tract: a potential paradigm shift. J Clin Microbiol. 2019;57:e00675-18.
Xue LJ, Yang XZ, Tong Q, et al. Fecal microbiota transplantation therapy for Parkinson's disease: a preliminary study. Medicine (Baltimore). 2020;99:e22035.
Madsen M, Kimer N, Bendtsen F, et al. Fecal microbiota transplantation in hepatic encephalopathy: a systematic review. Scand J Gastroenterol. 2021;56:560.
Goloshchapov OV, Olekhnovich EI, Sidorenko SV, et al. Long-term impact of fecal transplantation in healthy volunteers. BMC Microbiol. 2019;19:312.
Tariq R, Pardi DS, Tosh PK, et al. Fecal microbiota transplantation for recurrent Clostridium difficile infection reduces recurrent urinary tract infection frequency. Clin Infect Dis. 2017;65:1745.
Ballenghien M, Faivre N, Galtier N. Patterns of cross-contamination in a multispecies population genomic project: detection, quantification, impact, and solutions. BMC Biol. 2017;15:25.
Price TK, Wolff B, Halverson T, et al. Temporal dynamics of the adult female lower urinary tract microbiota. mBio. 2020;11:e00475-20.
Haylen BT, de Ridder D, Freeman RM, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn. 2010;29:4.
Wein AJ, Rovner ES. Definition and epidemiology of overactive bladder. Urology. 2002;60:7.
Ugarcina Perovic S, Ksiezarek M, Rocha J, et al. Time to change microbiological approach to overactive bladder. Eur Urol Suppl. 2019;18:e103.
Price T. A comparison of the female and male urinary microbiota in patients with and without lower urinary tract symptoms. 2017. 39th Annual American Urogynecologic Society (AUGS) Meeting, Providence, RI, USA.
Author information
Authors and Affiliations
Contributions
Study concept and design: Christina Sze, Mariel Pressler; acquisition of data: Christina Sze, Mariel Pressler; analysis and interpretation of data: none; drafting of the manuscript: Christina Sze, Mariel Pressler; critical revision of the manuscript for important intellectual content: Christina Sze, Mariel Pressler, John Richard Lee, Bilal Chughtai; supervision: Bilal Chughtai.
Corresponding author
Ethics declarations
Conflicts of interest
Christina Sze: none; Mariel Pressler: none; John Richard Lee: holds patent US-2020-0048713-A1 entitled “Methods of Detecting Cell-Free DNA in Biological Samples” and receives research support under an investigator-initiated research grant from BioFire Diagnostics, LLC; Bilal Chughtai: consultant for Allergan and Boston Scientific.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOCX 25 kb)
Rights and permissions
About this article
Cite this article
Sze, C., Pressler, M., Lee, J.R. et al. The gut, vaginal, and urine microbiome in overactive bladder: a systematic review. Int Urogynecol J 33, 1157–1164 (2022). https://doi.org/10.1007/s00192-022-05127-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-022-05127-3