Abstract
Introduction and hypothesis
Studies on non-obstetric urogenital fistulas (NOUGFs) provide limited information on predictive outcome factors. This study was aimed at specifying and analyzing the risk factors for long-term anatomical and functional results.
Methods
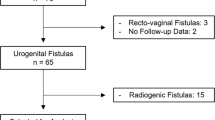
A cross-sectional study of surgical repair for non-obstetric urogenital fistula was performed. From 2012 to 2020, a total of 479 patients with urogenital fistulas were treated in two tertiary centers. Patients with isolated ureteral fistulas and rectal injuries were excluded. For evaluation of the long-term results, patients with vesicovaginal and urethrovaginal fistulas with at least 12 months of follow-up were identified and contacted by phone and/or examined in the clinic. The anatomical outcome was assessed by resolution of symptoms and/or clinical examination. The Urinary Distress Inventory (UDI-6) was used for the functional outcomes.
Results
Overall, 425 patients were studied (mean age was 49.8; BMI 27.5; mean fistula size 1.4 cm, mean follow-up was 12 months). Vesicovaginal fistula affected 73% of patients. Hysterectomy without radiation was the most common etiology (66.3%), followed by hysterectomy with subsequent radiation (16%) and pelvic radiotherapy (12.2%). The transvaginal approach was used in 54.4%, abdominal in 12.4%, transvesical in 22.4%, and a combined approach in 10.8%. The successful closure rate was 92.9% for primary cases, 71.6% for secondary cases, and 66.7% for radiation fistulas. A high risk for relapse was found for NOUGFs with ureteral involvement (RR 2.5; 95% CI 1.3–4.5; p = 0.003), radiation fistulas (RR 2.1; 95% CI 1.3–3.5, p = 0.003); and combined radiation and hysterectomy cases (RR 2.9; 95% CI 1.8–4.6; p = 0.0001). In multifactorial analysis, fistula size >3.0 cm, pelvic radiation, and previous vaginal surgeries were associated with a higher risk for failure or lower urinary symptoms.
Conclusions
Factors for successful NOUGF closure are fistula size less than 3.0 cm, absence of pelvic radiation, and previous vaginal surgeries.



Similar content being viewed by others
References
Wall LL. Obstetric vesicovaginal fistula as an international public health problem. Lancet. 2006;368:1201–9.
Danso K, Martey J, Wall L, Elkins T. The epidemiology of genitourinary fistulae in Kumasi, Ghana, 1977–1992. Int Urogynecol J Pelvic Floor Dysfunct. 1996;7(3):117–20.
Harkki-Siren P, Sjoberg J, Tiitinen A. Urinary tract injuries after hysterectomy. Obstet Gynecol. 1998;92:113–8.
Cromwell D, Hilton P. Retrospective cohort study on patterns of care and outcomes of surgical treatment for lower urinary-genital tract fistula among English National Health Service hospitals between 2000 and 2009. BJU Int. 2013;111:E257–62.
Pushkar DY, Dyakov VV, Kosko JW, Kasyan GR. Management of urethrovaginal fistulas. Eur Urol. 2006;50:1000–5.
Bernis L. Obstetric fistula: guiding principles for clinical management and programme development, a new WHO guideline. Int J Gynaecol Obstet. 2007;99(Suppl 1):S117–21.
Goh JT. A new classification for female genital tract fistula. Aust N Z J Obstet Gynaecol. 2004;44(6):502–4. https://doi.org/10.1111/j.1479-828X.2004.00315.x.
Beardmore-Gray A, Pakzad M, Hamid R, Ockrim J, Greenwell T. Does the Goh classification predict the outcome of vesico-vaginal fistula repair in the developed world? Int Urogynecol J. 2017;28(6):937–40. https://doi.org/10.1007/s00192-016-3186-2.
Cromwell D, Hilton P. Retrospective cohort study on patterns of care and outcomes of surgical treatment for lower urinary–genital tract fistula among English National Health Service hospitals between 2000 and 2009. BJU Int. 2012;111(4 Pt B):E257–62.
Browning A. Risk factors for developing residual urinary incontinence after obstetric fistula repair. BJOG. 2006;113:482–5.
Hillary CJ, Osman NI, Hilton P, Chapple CR. The aetiology, treatment, and outcome of urogenital fistulae managed in well- and low-resourced countries: a systematic review. Eur Urol. 2016;70(3):478–92. https://doi.org/10.1016/j.eururo.2016.02.015.
Uebersax JS, Wyman FF, Shumaker SA, et al. Short forms to assess life quality and symptom distress for urinary incontinence in women: the incontinence impact questionnaire and urogenital distress inventory. Neurourol Urodyn. 1995;14:131.
Bodner-Adler B, Hanzal E, Pablik E, Koelbl H, Bodner K. Management of vesicovaginal fistulas (VVFs) in women following benign gynaecologic surgery: a systematic review and meta-analysis. PLoS One. 2017;12(2):e0171554. https://doi.org/10.1371/journal.pone.0171554.
El-Azab AS, Abolella HA, Farouk M. Update on vesicovaginal fistula: a systematic review. Arab J Urol. 2019;17(1):61–8. https://doi.org/10.1080/2090598X.2019.1590033.
Waaldijk K. Surgical classification of obstetric fistulas. Int J Gynecol Obstet. 1995;49:161–3. https://doi.org/10.1016/0020-7292(95)02350-L.
Ockrim JL, Greenwell TJ, Foley CL, Wood DN, Shah PJ. A tertiary experience of vesico-vaginal and urethro-vaginal fistula repair: factors predicting success. BJU Int. 2009;103(8):1122–6. https://doi.org/10.1111/j.1464-410X.2008.08237.x.
Eilber KS, Kavaler E, Rodriguez LV, Rosenblum N, Raz S. Ten-year experience with transvaginal vesicovaginal fistula repair using tissue interposition. J Urol. 2003;169:1033–6.
Pushkar DY, Dyakov VV, Kasyan GR. Management of radiation-induced vesicovaginal fistula. Eur Urol. 2009;55:131–8.
Grewal M, Pakzad MH, Hamid R, Ockrim JL, Greenwell TJ. The medium- to long-term functional outcomes of women who have had successful anatomical closure of vesicovaginal fistulae. Urol Ann. 2019;11(3):247–51. https://doi.org/10.4103/UA.UA_56_18.
Lee D, Dillon BE, Lemack GE, Zimmern PE. Long-term functional outcomes following non-radiated vesicovaginal repair. J Urol. 2014;191:120–4.
Dolan LM, Dixon WE, Hilton P. Urinary symptoms and quality of life in women following urogenital fistula repair: a long-term follow-up study. BJOG. 2008;115(12):1570–4.
Stewart WF, Van Rooyen JB, Cundiff GW, Abrams P, Herzog AR, Corey R, et al. Prevalence and burden of overactive bladder in the United States. World J Urol. 2003;20(6):327–36.
Wennberg AL, Molander U, Fall M, Edlund C, Peeker R, Milsom I. A longitudinal population-based survey of urinary incontinence, overactive bladder, and other lower urinary tract symptoms in women. Eur Urol. 2009;55(4):783–91. https://doi.org/10.1016/j.eururo.2009.01.007.
Milsom I, Abrams P, Cardozo L, Roberts RG, Thüroff J, Wein AJ. How widespread are the symptoms of an overactive bladder and how are they managed? A population-based prevalence study. BJU Int. 2001;87(9):760–6.
Milsom I. Lower urinary tract symptoms in women. Curr Opin Urol. 2009;19(4):337–41.
Author information
Authors and Affiliations
Contributions
Dmitry Pushkar: project development, manuscript editing; George Kasyan: project development, data collection, manuscript writing; Rustam Sheripbaev: data collection; Sukrat Mukhtarov: data collection; Lyudmila Tikhonova: data collection, statistical analysis.
Corresponding author
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pushkar, D., Kasyan, G., Sheripbaev, R. et al. Anatomical and functional outcomes of non-obstetric urogenital fistula repair. Int Urogynecol J 33, 3221–3229 (2022). https://doi.org/10.1007/s00192-021-05073-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-021-05073-6