Abstract
Introduction and hypothesis
There are few studies examining patient risk factors for postoperative complications following midurethral sling (MUS) placement for stress urinary incontinence (SUI). The objective of this study was to describe 30-day postoperative complications after MUS using the National Surgical Quality Improvement Program database. Secondary objectives included rates of readmission and patient factors associated with postoperative complications and readmissions following MUS.
Methods
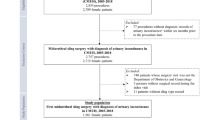
We identified 16,491 women who underwent MUS for SUI between 2014 and 2018. American Society of Anesthesia (ASA) classification, medical comorbidities, readmission, reoperation, and 30-day postoperative complications were extracted. Outcomes included the 30-day postoperative complications, readmission, and reoperations. Descriptive statistics, univariate analyses, and multivariate logistic regression were used.
Results
The majority of patients were white (66.9%) and had an ASA classification II (60.9%). Postoperative complications occurred in 4.2% of patients; 1.5% required readmission and 1.0% required reoperation. The most common complication was urinary tract infection (3.4%). Using multivariate logistic regression, older age, i.e., ≥80 years of age, was associated with increased odds of complication (aOR 1.77, 95%CI 1.14–2.72) and readmission (aOR 3.84, 95%CI 1.76–8.66). ASA class III and IV were associated with increased odds of complications (aOR 1.55, 95%CI 1.13–2.14, and aOR 3.06, 95% CI 1.48–5.86 respectively) and readmissions. Women of Asian, American Indian or Alaska Native, and Native Hawaiian or Pacific Islander descent (“other”) were associated with increased postoperative complications (aOR 1.51, 95%CI 1.07–2.07).
Conclusion
Postoperative complications following MUS are rare. Factors associated with complications following MUS for SUI include age, ASA class, and women of “other” race.
Similar content being viewed by others
References
Melville JL, Katon W, Delaney K, Newton K. Urinary incontinence in US women: a population-based study. Arch Intern Med. 2005;165(5):537–42. https://doi.org/10.1001/archinte.165.5.537.
Garely AD, Noor N. Diagnosis and surgical treatment of stress urinary incontinence. Obstet Gynecol. 2014;124(5):1011–27.
Labrie J, Berghmans BLCM, Fischer K, et al. Surgery versus physiotherapy for stress urinary incontinence. N Engl J Med. 2013;369(12):1124–33. https://doi.org/10.1056/NEJMoa1210627.
Richardson ML, Sokol ER. A cost-effectiveness analysis of conservative versus surgical management for the initial treatment of stress urinary incontinence. Am J Obstet Gynecol 2014;211(5):565.e1–6. https://doi.org/10.1016/j.ajog.2014.07.006.
American College of Obstetricians and Gynecologists. ACOG Practice Bulletin No. 155: urinary incontinence in women. Obstet Gynecol. 2015;126(5):e66–e81.
U.S. Food and Drug Administration. Considerations about surgical mesh for SUI. Available at: https://www.fda.gov/MedicalDevices/ProductsandMedicalProcedures/ImplantsandProsthetics/UroGynSurgicalMesh/ucm345219.htm. Accessed 27 Apr 2020.
Jonsson Funk M, Levin PJ, Wu JM. Trends in the surgical management of stress urinary incontinence. Obstet Gynecol. 2012;119(4):845–51. https://doi.org/10.1097/AOG.0b013e31824b2e3e.
Ford AA, Rogerson L, Cody JD, Aluko P, Ogah JA. Mid-urethral sling operations for stress urinary incontinence in women. Cochrane Database Syst Rev. 2017;7:CD006375. https://doi.org/10.1002/14651858.CD006375.pub4.
FDA Safety Communication. Update on serious complications associated with transvaginal placement of surgical mesh for pelvic organ prolapse. Issued on July 13, 2011. Available at: http://www.fda.gov/medicaldevices/safety/alertsandnotices/ucm262435.htm. Accessed 20 Apr 2020.
Trabuco EC, Linder BJ, Klingele CJ, Blandon RE, Occhino JA, Weaver AL, McGree ME, Gebhart JB. Two-year results of Burch compared with midurethral sling with sacrocolpopexy: a randomized controlled trial. Obstet Gynecol. 2018;131(1):31–8. https://doi.org/10.1097/aog.0000000000002415.
Schimpf MO, Rahn DD, Wheeler TL, et al.. Sling surgery for stress urinary incontinence in women: a systematic review and metaanalysis. Am J Obstet Gynecol 2014;211(1):71.e1–71.e27. https://doi.org/10.1016/j.ajog.2014.01.030.
Dmochowski RR, Blaivas JM, Gormley EA, et al. Update of AUA guideline on the surgical management of female stress urinary incontinence. J Urol. 2010;183(5):1906–14. https://doi.org/10.1016/j.juro.2010.02.2369.
Propst K, O'Sullivan DM, Tulikangas PK. Suburethral sling procedures in the United States: complications, readmission, and reoperation. Int Urogynecol J. 2017;28(10):1463–7. https://doi.org/10.1007/s00192-017-3293-8.
Hokenstad ED, Glasgow AE, Habermann EB, Occhino JA. Readmission and reoperation after midurethral sling. Int Urogynecol J. 2018;29(9):1367–70. https://doi.org/10.1007/s00192-017-3551-9.
Doganay M, Cavkaytar S, Kokanali MK, Ozer I, Aksakal OS, Erkaya S. Risk factors for postoperative urinary tract infection following midurethral sling procedures. Eur J Obstet Gynecol Reprod Biol. 2017;211:74–7. https://doi.org/10.1016/j.ejogrb.2017.02.006.
ACS National Surgical Quality Improvement Program. (ACS NSQIP): American College of Surgeons. Available at: https://www.facs.org/quality-programs/acs-nsqip/hub.e. Accessed 9 Feb 2020.
ACS National Surgical Quality Improvement Program Partipiant Use Data File. (ACS NSQIP PUF): American College of Surgeons. Available at: https://www.facs.org/quality-programs/acs-nsqip/participant-use. Accessed 9 Feb 2020.
Chapman GC, Sheyn D, Slopnick EA, Hijaz AK, Mahajan ST, Mangel J, El-Nashar SA. Perioperative safety of surgery for pelvic organ prolapse in elderly and frail patients. Obstet Gynecol. 2020;135(3):599–608. https://doi.org/10.1097/aog.0000000000003682.
Berger AA, Tan-Kim J, Menefee SA. Long-term risk of reoperation after synthetic mesh midurethral sling surgery for stress urinary incontinence. Obstet Gynecol. 2019;134(5):1047–55. https://doi.org/10.1097/aog.0000000000003526.
Bretschneider CE, Robinson B, Geller EJ, Wu JM. The effect of age on postoperative morbidity in women undergoing urogynecologic surgery. Female Pelvic Med Reconstr Surg. 2015;21(4):236–40. https://doi.org/10.1097/spv.0000000000000150.
Sung VW, Weitzen S, Sokol ER, Rardin CR, Myers DL. Effect of patient age on increasing morbidity and mortality following urogynecologic surgery. Am J Obstet Gynecol. 2006;194(5):1411–7. https://doi.org/10.1016/j.ajog.2006.01.050.
Gandhi J, Chen A, Dagur G, Suh Y, Smith N, Cali B, Khan SA. Genitourinary syndrome of menopause: an overview of clinical manifestations, pathophysiology, etiology, evaluation, and management. Am J Obstet Gynecol. 2016;215(6):704–11. https://doi.org/10.1016/j.ajog.2016.07.045.
Rowe TA, Juthani-Mehta M. Urinary tract infection in older adults. Aging Health. 2013;9(5):519–28. https://doi.org/10.2217/ahe.13.38.
Erekson EA, Yip SO, Ciarleglio MM, Fried TR. Postoperative complications after gynecologic surgery. Obstet Gynecol. 2011;118(4):785–93. https://doi.org/10.1097/AOG.0b013e31822dac5d.
Myles PS, Iacono GA, Hunt JO, Fletcher H, Morris J, McIlroy D, Fritschi L. Risk of respiratory complications and wound infection in patients undergoing ambulatory surgery: smokers versus nonsmokers. Anesthesiology. 2002;97(4):842–7. https://doi.org/10.1097/00000542-200210000-00015.
Sorensen LT, Karlsmark T, Gottrup F. Abstinence from smoking reduces incisional wound infection: a randomized controlled trial. Ann Surg. 2003;238(1):1–5. https://doi.org/10.1097/01.Sla.0000074980.39700.31.
Rogers RG, Lebküchner U, Kammerer-Doak DN, Thompson PK, Walters MD, Nygaard IE. Obesity and retropubic surgery for stress incontinence: is there really an increased risk of intraoperative complications? Am J Obstet Gynecol. 2006;195(6):1794–8. https://doi.org/10.1016/j.ajog.2006.07.012.
Pratt TS, Hudson CO, Northington GM, Greene KA. Obesity and perioperative complications in pelvic reconstructive surgery in 2013: analysis of the National Inpatient Sample. Female Pelvic Med Reconstr Surg. 2018;24(1):51–5.
Chen CCG, Collins SA, Rodgers AK, Paraiso MFR, Walters MD, Barber MD (2007) Perioperative complications in obese women vs normal-weight women who undergo vaginal surgery. Am J Obstet Gynecol 197(1):98.e1–98.e8. https://doi.org/10.1016/j.ajog.2007.03.055.
Dallas KB, Sohlberg EM, Elliott CS, Rogo-Gupta L, Enemchukwu E. Racial and socioeconomic disparities in short-term urethral sling surgical outcomes. Urology. 2017;110:70–5. https://doi.org/10.1016/j.urology.2017.08.021.
Muffly TM, Weterings R, Barber MD, Steinberg AC. Discrepancies in the female pelvic medicine and reconstructive surgeon workforce. Female Pelvic Med Reconstr Surg. 2015;21(2):99–105. https://doi.org/10.1097/spv.0000000000000143.
Richter HE, Albo ME, Zyczynski HM, et al. Retropubic versus transobturator midurethral slings for stress incontinence. N Engl J Med. 2010;362(22):2066–76. https://doi.org/10.1056/NEJMoa0912658.
Deffieux X, Thubert T, de Tayrac R, Fernandez H, Letouzey V. Long-term follow-up of persistent vaginal polypropylene mesh exposure for transvaginally placed mesh procedures. Int Urogynecol J. 2012;23(10):1387–90. https://doi.org/10.1007/s00192-012-1741-z.
Author information
Authors and Affiliations
Contributions
M.L. Bonus: manuscript writing, editing, data analysis; D. Luchristt: editing, data analysis; O. Brown: editing; S. Collins: editing; K. Kenton: editing; C.E. Bretschneider: manuscript writing, editing, data analysis.
Corresponding author
Ethics declarations
Conflicts of interest
Dr. Kenton was on the strategic advisory board for Boston Scientific and is an expert witness for Ethicon. All other authors have no conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bonus, M.L., Luchristt, D., Brown, O. et al. Predictors of postoperative complications from stress urinary incontinence procedures: a NSQIP database study. Int Urogynecol J 33, 2291–2297 (2022). https://doi.org/10.1007/s00192-021-05047-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-021-05047-8