Abstract
Introduction and hypothesis
The objective was to identify the associations between metabolic syndrome (MS) and stress urinary incontinence (SUI) in women and to provide an evidence base for clinical practice.
Methods
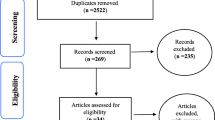
A meta-analysis of cohort, case–control, and cross-sectional studies about the association between MS and SUI was performed using databases including PubMed, Cochrane Library, Web of Science, Embase, China National Knowledge Infrastructure (CNKI), China Biology Medicine disc (CBMdisc), Wanfang Database (WanFang Data), and VIP database (VIP). The time limit was from the commencement of each database to 1 November 2020. Two researchers independently screened literature, extracted data, and assessed the risk of bias. RevMan 5.3 software was used for statistical analysis. The dichotomous variables were presented as the risk ratio (odds ratio, OR) and 95% CI as the effect indicators.
Results
Six studies were included in the meta-analysis, with a total sample size of 3,678 cases. The results showed that the risk for SUI in women with MS was three times those without MS (OR = 3.41, 95% CI 2.01, 5.77, p <0.00001), and the difference was statistically significant. The results of subgroup analysis showed that MS was significantly associated with SUI in the subgroups of pre- and postmenopausal women (OR = 2.46, 95% CI 1.63, 3.73, p < 0.00001), and in the subgroups of other types of women (OR = 3.41, 95% CI 2.01, 5.77, p = 0.0003), and the differences were statistically significant.
Conclusions
Metabolic syndrome is associated with SUI in women and increases its risk.




Similar content being viewed by others
References
Abrams P, Andersson KE, Birder L, Brubaker L, Cardozo L, Chapple C, et al. Fourth International Consultation on Incontinence Recommendations of the International Scientific Committee: evaluation and treatment of urinary incontinence, pelvic organ prolapse, and fecal incontinence. Neurourol Urodyn. 2010;29(1):213–40. https://doi.org/10.1002/nau.20870.
Zhu L, Sun Z. Update of guideline on the diagnosis and treatment of female stress urinary incontinence (2017). Chin J Obstet Gynecol. 2017;52(5):289–93. https://doi.org/10.3760/cma.j.issn.0529-567X.2017.05.001.
Pan J, Xu L, Lv J, Sha J, Zhang L, Bo J, et al. Epidemiological study on stress urinary incontinence in 2410 women in Shanghai. J Shanghai Jiaotong Univ Med Sci. 2012;32(4):419-422. https://doi.org/10.3969/j.issn.1674-8115.2012.04.011
Huan H, Lyu J, Zhu S, Jiang S, Li N. Survey on knowledge of stress urinary incontinence in postpartum women in Shanghai Meilong district. Chin J Gen Pract. 2018;17(3):181–5. https://doi.org/10.3760/cma.j.issn.1671-7368.2018.03.004.
Punthakee Z, Goldenberg R, Katz P. Definition, classification and diagnosis of diabetes, prediabetes and metabolic syndrome. Can J Diabetes. 2018;42(Suppl 1):S10–5. https://doi.org/10.1016/j.jcjd.2017.10.003.
Kolodynska G, Zalewski M, Rozek PK. Urinary incontinence in post-menopausal women-causes, symptoms, treatment. Prz Menopauzalny. 2019;18(1):46–50. https://doi.org/10.5114/pm.2019.84157_rfseq1.
Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–5. https://doi.org/10.1007/s10654-010-9491-z.
Rostom A, Dubé C, Cranney A, Saloojee N, Sy R, Garritty C, et al. Appendix D. Quality assessment forms. In: Celiac disease. Evidence Report/Technology Assessment No. 104. (Prepared by the University of Ottawa Evidence-based Practice Center, under Contract No. 290-02-0021.) AHRQ Publication No. 04-E029-2. Rockville, MD: Agency for Healthcare Research and Quality. September 2004.
Kim YH, Kim JJ, Kim SM, Choi Y, Jeon MJ. Association between metabolic syndrome and pelvic floor dysfunction in middle-aged to older Korean women. Am J Obstet Gynecol. 2011;205(1):71.e1–8. https://doi.org/10.1016/j.ajog.2011.02.047.
Otunctemur A, Dursun M, Ozbek E, Sahin S, Besiroglu H, Koklu I, et al. Impact of metabolic syndrome on stress urinary incontinence in pre- and postmenopausal women. Int Urol Nephrol. 2014;46(8):1501–5. https://doi.org/10.1007/s11255-014-0680-7.
Ströher RLM, Sartori MGF, Takano CC, de Araújo MP, Girão MJBC. Metabolic syndrome in women with and without stress urinary incontinence. Int Urogynecol J. 2020;31(1):173–9. https://doi.org/10.1007/s00192-019-03880-6.
Gleicher S, Byler T, Ginzburg N. Association between stress urinary incontinence and the components of metabolic syndrome among females 20–59 years. Urology. 2020;11(145):100–5. https://doi.org/10.1016/j.urology.2020.07.028.
Candoso B, Meneses MJ, Alves MG, Sousa M, Oliveira PF. Molecular aspects of collagenolysis associated with stress urinary incontinence in women with urethral hypermobility vs intrinsic sphincter deficiency. Neurourol Urodyn. 2019;38(6):1533–9. https://doi.org/10.1002/nau.24026.
Campeau L, Gorbachinsky I, Badlani GH, Andersson KE. Pelvic floor disorders: linking genetic risk factors to biochemical changes. BJU Int. 2011;108(8):1240–7. https://doi.org/10.1111/j.1464-410X.2011.10385.x.
Knuuti E, Kauppila S, Kotila V, Risteli J, Nissi R. Genitourinary prolapse and joint hypermobility are associated with altered type I and III collagen metabolism. Arch Gynecol Obstet. 2011;283(5):1081–5. https://doi.org/10.1007/s00404-010-1518-x.
Weinberg AE, Leppert JT, Elliott CS. Biochemical measures of diabetes are not independent predictors of urinary incontinence in women. J Urol. 2015;194(6):1668–74. https://doi.org/10.1016/j.juro.2015.06.074.
Watanabe J, Kotani K. Metabolic syndrome for cardiovascular disease morbidity and mortality among general Japanese people: a mini review. Vasc Health Risk Manag. 2020;16:149–55. https://doi.org/10.2147/VHRM.S245829.
Tai HC, Chung SD, Ho CH, Tai T-Y, Yang WS, Tseng C-H, et al. Metabolic syndrome components worsen lower urinary tract symptoms in women with type 2 diabetes. J Clin Endocrinol Metab. 2010;95(3):1143–50. https://doi.org/10.1210/jc.2009-1492.
Funding
This study was funded by a Special research project of the National Clinical Research Base of Traditional Chinese Medicine in 2019 (grant number JDZX201920).
Author information
Authors and Affiliations
Contributions
H. Huang: project development, data collection, manuscript writing; X. Han and Q. Liu: data collection, manuscript writing; J. Xue and Z. Yu: assessed the risk of bias; S. Miao: checked the information extracted from the data and the results of the risk assessment.
Corresponding author
Ethics declarations
Conflicts of interest
None.
Study registration
This systematic review is register with PROSPERO (CRD42021231965).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Huang, H., Han, X., Liu, Q. et al. Associations between metabolic syndrome and female stress urinary incontinence: a meta-analysis. Int Urogynecol J 33, 2073–2079 (2022). https://doi.org/10.1007/s00192-021-05025-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-021-05025-0