Abstract
Introduction and hypothesis
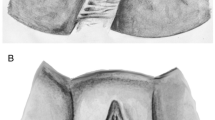
The International Continence Society recommends vaginal palpation as a method for assessing pelvic floor muscle (PFM) function. Our aim was to analyze the agreement between preferences of examiner and participants according to unidigital and bidigital vaginal palpation during PFM assessment. The second aim was to investigate qualitatively women’s perception of vaginal palpation.
Methods
Maximal voluntary contractions (MVCs) were requested during both types of vaginal palpation and were classified by the Modified Oxford Scale (MOS). Examiner and participants answered if they had preferences regarding vaginal palpation. Women answered qualitatively what they felt during the assessment. Cohen’s linear kappa (κ) evaluated the agreement after allocation of the women with a weaker and stronger MVC and qualitative analysis was performed by transcription considering age range (18–35; 36–59; ≥60 years).
Results
Agreement was almost zero for women with weaker and stronger MVC at unidigital (κ = 0.06 and κ = −0.12) and bidigital vaginal palpation (κ = 0.008 and κ = 0.005). Participants associated bidigital palpation with more perception and an easier way of contracting the PFMs. Women between 36 and 59 years associated unidigital palpation with a harder but comfortable way of contracting the PFMs. Subjects aged ≥60 years associated bidigital palpation with an uncomfortable, harder way of contracting PFM, with less space into the vagina.
Conclusions
Agreement between preferences was almost zero neither between women with a weaker and stronger PFM contraction, nor between the types of vaginal palpation. Bidigital palpation increased women’s perception, made the contraction easier, and was associated with less space in the vaginal canal and less comfort.


Similar content being viewed by others
References
Knuttgen HG, Kraemer WJ (1987). Terminology and measurement in exercise performance. J Strength Cond Res 1(1):1–10.
Messelink B, Benson T, Berghmans B, et al. Standardization of terminology of pelvic floor muscle function and dysfunction: report from the pelvic floor clinical assessment group of the International Continence Society. Neurourol Urodyn. 2005;24:374–80. https://doi.org/10.1002/nau.20144.
Deegan EG, Stothers L, Kavanagh A, Macnab AJ. Quantification of pelvic floor muscle strength in female urinary incontinence: a systematic review and comparison of contemporary methodologies. Neurourol Urodyn. 2018;37:33–45. https://doi.org/10.1002/nau.23285.
Ferreira CHJ, Barbosa PB, de Souza FO, et al. Inter-rater reliability study of the modified Oxford grading scale and the Peritron manometer. Physiotherapy. 2011;97:132–8. https://doi.org/10.1016/j.physio.2010.06.007.
Devreese A, Staes F, De Weerdt W, et al. Clinical evaluation of pelvic floor muscle function in continent and incontinent women. Neurourol Urodyn. 2004;23:190–7. https://doi.org/10.1002/nau.20018.
Laycock J, Jerwood D. Pelvic floor muscle assessment: the PERFECT scheme. Physiotherapy. 2001;87:631–42. https://doi.org/10.1016/S0031-9406(05)61108-X.
Silva JB, Sato TO, Rocha APR, Driusso P. Comparative intra- and inter-rater reliability of maximal voluntary contraction with unidigital and bidigital vaginal palpation and construct validity with Peritron manometer. Neurourol Urodyn. 2019;39:721–31. https://doi.org/10.1002/nau.24263.
Silva JB, Oliveira Sato T, Rocha APR, Driusso P. Inter- and intrarater reliability of unidigital and bidigital vaginal palpation to evaluation of maximal voluntary contraction of pelvic floor muscles considering risk factors and dysfunctions. Neurourol Urodyn. 2020;40(1):348-357. https://doi.org/10.1002/nau.24566.
Bø K, Sherburn M. Evaluation of female pelvic-floor muscle function and strength. Phys Ther. 2005;85(3):269-82. https://doi.org/10.1093/ptj/85.3.269.
Da Silva JB, de Godoi Fernandes JG, Caracciolo BR, et al. Reliability of the PERFECT scheme assessed by unidigital and bidigital vaginal palpation. Int Urogynecol J. 2021. https://doi.org/10.1007/s00192-020-04629-2.
Nilsagård Y, Westerdahl E, Forsberg A. Engagement in performing clinical physiotherapy research: perspectives from leaders and physiotherapists. Physiother Res Int. 2019;24:e1767. https://doi.org/10.1002/pri.1767.
Cantor AB. Sample-size calculations for Cohen’s kappa. Psychol Methods. 1996;1:150–3.
Barnhart KT, Izquierdo A, Pretorius ES, et al. Baseline dimensions of the human vagina. Hum Reprod. 2006;21:1618–22. https://doi.org/10.1093/humrep/del022.
Alperin M, Cook M, Tuttle LJ, et al. Impact of vaginal parity and aging on the architectural design of pelvic floor muscles. Am J Obstet Gynecol. 2016;215:312.e1–9. https://doi.org/10.1016/j.ajog.2016.02.033.
Alperin M, Feola A, Duerr R, et al. Pregnancy- and delivery-induced biomechanical changes in rat vagina persist postpartum. Int Urogynecol J. 2010;21:1169–74. https://doi.org/10.1007/s00192-010-1149-6.
Dietz HP, Scoti F, Subramaniam N, et al. Impact of subsequent pregnancies on pelvic floor functional anatomy. Int Urogynecol J. 2018;29:1517–22. https://doi.org/10.1007/s00192-018-3567-9.
Bø K, Stien R. Needle EMG registration of striated urethral wall and pelvic floor muscle activity patterns during cough, Valsalva, abdominal, hip adductor, and gluteal muscle contractions in nulliparous healthy females. Neurourol Urodyn. 1994;13:35–41. https://doi.org/10.1002/nau.1930130106.
Faubion SS, Sood R, Kapoor E. Genitourinary syndrome of menopause: management strategies for the clinician. Mayo Clin Proc. 2017;92:1842–9. https://doi.org/10.1016/j.mayocp.2017.08.019.
North American Menopause Society. Management of symptomatic vulvovaginal atrophy: 2013 Position statement of the North American Menopause Society. Menopause 2013;20:888–902. https://doi.org/10.1097/GME.0b013e3182a122c2.
Uechi N, Fernandes ACNL, Bø K, et al. Do women have an accurate perception of their pelvic floor muscle contraction? A cross-sectional study. Neurourol Urodyn. 2020;39:361–6. https://doi.org/10.1002/nau.24214.
Funding
This study was funded by in part by Coordenação de Aperfeiçoamento de Pessoal de Ensino Superior (CAPES); Finance Code 0001.
Author information
Authors and Affiliations
Contributions
JBS: substantial contributions to conception and design, drafting and revising the article critically for important intellectual content, final approval of the version to be published; APRR: substantial contributions to conception and design, drafting and revising the article critically for important intellectual content, final approval of the version to be published; TOS: substantial contributions to conception and design, drafting and revising the article critically for important intellectual content, final approval of the version to be published; PD: substantial contributions to conception and design, drafting and revising the article critically for important intellectual content; 3) Final approval of the version to be published.
Corresponding author
Ethics declarations
Ethical approval
This study was approved by the Ethics and Research Committee of the Federal University of São Carlos (CAAE: 51999415.9.0000.5504).
Conflicts of interest
The authors declare that there are no conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
da Silva, J.B., Rocha, A.P.R., Sato, T.d.O. et al. Is there agreement between the preference of examiner and women for unidigital and bidigital vaginal palpation? A qualitative study. Int Urogynecol J 32, 3293–3299 (2021). https://doi.org/10.1007/s00192-021-04935-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-021-04935-3