Abstract
Introduction and hypothesis
Pelvic organ prolapse (POP) is a common gynecological disease caused by defects in pelvic support tissue that manifests as the descent of the pelvic organs, significantly impacting patient quality of life. Transvaginal mesh (TVM) is an effective treatment (Grade A). However, postoperative pain in the groin and medial thigh is very common. Although the use of mesh for transvaginal POP repair has been prohibited or the indications for such use have been extensively limited in many places, it is still an alternative in some countries. Therefore, the safety of the use of mesh still needs to be discussed. The current research on postoperative pain has mainly focused on management. The pathophysiology is unclear.
Methods
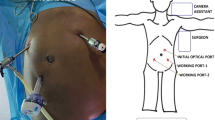
In this study, anterior TVM surgery was performed on ten frozen cadavers. The obturator area was carefully dissected. We explored the relative position of the polypropylene mesh to the internal segment of the obturator nerve in the obturator canal.
Results
Four out of 20 obturator explorations were insufficient to allow conclusions to be drawn. We observed a small branch of the obturator nerve, which is a new anatomical finding that we named the obturator externus muscle branch. This structure terminated in the external obturator muscle in 6 out of the 16 successfully dissected obturator areas. The mean distance between the superficial mesh arm and this nerve branch was 7.5 mm. The mean distance between the deep mesh arm and the closest nerve branch was 5.5 mm.
Conclusion
The path of the obturator externus muscle branch of the obturator nerve ran close to the mesh arm. It may provide a clinical anatomical basis explaining the observed postoperative pain.



Similar content being viewed by others
References
Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J. 2010;21:5–26. https://doi.org/10.1007/s00192-009-0976-9.
Gao Y, Zhao Z, Yang Y, Zhang M, Wu J, Miao Y. Diagnostic value of pelvic floor ultrasonography for diagnosis of pelvic organ prolapse: a systematic review. Int Urogynecol J. 2020;31(1):15–33. https://doi.org/10.1007/s00192-019-04066-w.
Siddiqui NY, Gregory WT, Handa VL, DeLancey JOL, Richter HE, Moalli P, et al. American Urogynecologic Society prolapse consensus conference summary report. Female Pelvic Med Reconstr Surg. 2018;24(4):260–3. https://doi.org/10.1097/spv.0000000000000533.
Madhu C, Swift S, Moloney-Geany S, Drake MJ. How to use the pelvic organ prolapse quantification (POP-Q) system? Neurourol Urodyn. 2018;37(S6):S39–s43. https://doi.org/10.1002/nau.23740.
Ugianskiene A, Davila GW, Su TH. FIGO review of statements on use of synthetic mesh for pelvic organ prolapse and stress urinary incontinence. Int J Gynaecol Obstet. 2019;147(2):147–55. https://doi.org/10.1002/ijgo.12932.
Kasyan G, Abramyan K, Popov AA, Gvozdev M, Pushkar D. Mesh-related and intraoperative complications of pelvic organ prolapse repair. Cent European J Urol. 2014;67(3):296–301. https://doi.org/10.5173/ceju.2014.03.art17.
Heneghan CJ, Goldacre B, Onakpoya I, Aronson JK, Jefferson T, Pluddemann A, et al. Trials of transvaginal mesh devices for pelvic organ prolapse: a systematic database review of the US FDA approval process. BMJ Open. 2017;7(12):e017125. https://doi.org/10.1136/bmjopen-2017-017125.
Illston JD, Garris JB, Richter HE, Wheeler TL 2nd. Pain scores and exposure rates after polypropylene mesh for pelvic organ prolapse. South Med J. 2015;108(12):715–21. https://doi.org/10.14423/smj.0000000000000377.
Falconer C, Altman D, Poutakidis G, Rahkola-Soisalo P, Mikkola T, Morcos E. Long-term outcomes of pelvic organ prolapse repair using a mesh-capturing device when comparing single- versus multicenter use. Arch Gynecol Obstet. 2021;303(1):135–42. https://doi.org/10.1007/s00404-020-05764-3.
Rogowski A, Bienkowski P, Tosiak A, Jerzak M, Mierzejewski P, Baranowski W. Mesh retraction correlates with vaginal pain and overactive bladder symptoms after anterior vaginal mesh repair. Int Urogynecol J. 2013;24(12):2087–92. https://doi.org/10.1007/s00192-013-2131-x.
Sartore A, Zennaro F, Banco R. An unusual long-term complication of transobturator polypropylene mesh. Arch Gynecol Obstet. 2014;290(6):1273–4. https://doi.org/10.1007/s00404-014-3368-4.
Gyang AN, Feranec JB, Patel RC, Lamvu GM. Managing chronic pelvic pain following reconstructive pelvic surgery with transvaginal mesh. Int Urogynecol J. 2014;25(3):313–8. https://doi.org/10.1007/s00192-013-2256-y.
Marcus-Braun N, Bourret A, von Theobald P. Persistent pelvic pain following transvaginal mesh surgery: a cause for mesh removal. Eur J Obstet Gynecol Reprod Biol. 2012;162(2):224–8. https://doi.org/10.1016/j.ejogrb.2012.03.002.
Kowalik CR, Lakeman MME, Oryszczyn JE, Roovers J. Reviewing patients following mesh repair; the benefits. Gynecol Obstet Investig. 2017;82(6):575–81. https://doi.org/10.1159/000454925.
Wang W, Zhu L, Wei B, Lang J. An anatomical comparison of two minimally invasive pelvic reconstructive surgeries using fresh female cadavers. Chin Med J. 2014;127(8):1510–6.
Costantini R, Affaitati G, Fabrizio A, Giamberardino MA. Controlling pain in the post-operative setting. Int J Clin Pharmacol Ther. 2011;49(2):116–27. https://doi.org/10.5414/cp201401.
Iwanaga J, Ishak B, Yilmaz E, von Glinski A, Gielecki J, Dumont AS, et al. Anatomic study of the bifurcation of the obturator nerve: application to more precise surgical/procedural localization. World Neurosurg. 2020;140:e23–6. https://doi.org/10.1016/j.wneu.2020.03.113.
Acknowledgments
We thank Prof. Naili Wang (Peking Union Medical College) for his help with anatomy.
Funding
This study was funded by the State Key Program of National Natural Science Foundation of China (grant number No. 81830043).
Author information
Authors and Affiliations
Contributions
L Zhu: Project development, data collection, manuscript writing and editing.
L Zhang and Z Zhao: Data collection, data analysis, manuscript writing and editing.
J Chen and Y Ma: Data collection, protocol development.
G Zhang: Protocol development.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhang, L., Zhao, Z., Chen, J. et al. Path-related pain after implantation of anterior transvaginal mesh: perspective from anatomical study. Int Urogynecol J 33, 2551–2556 (2022). https://doi.org/10.1007/s00192-021-04924-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-021-04924-6