Abstract
Introduction and hypothesis
To identify preoperative level II/III MRI measures associated with long-term recurrence after native tissue prolapse repair.
Methods
Women who previously participated in pelvic floor research involving MRI prior to undergoing primary native tissue prolapse repair were recruited to return for repeat examination and MRI. Recurrence was defined by POP-Q (Ba/Bp > 0 or C > –4), repeat surgery, or pessary use. Preoperative MR images were used to perform five level II/III measurements including a new levator plate (LP) shape analysis at rest and maximal Valsalva. Principal component analysis (PCA) was used to evaluate LP shape variations. Principal component scores calculated for two independent shape variations were noted.
Results
Thirty-five women were included with a mean follow-up of 13.2 ± 3.3 years. Nineteen (54%) were in the success group. There were no statistical differences between success versus recurrence groups in demographic, clinical, or surgical characteristics. Women with recurrence had a larger preoperative resting levator hiatus [median 6.4 cm (IQR 5.7, 7.1) vs. 5.8 cm (IQR 5.3, 6.3), p = 0.03]. This measure was associated with increased odds of recurrence (OR 8.2, CI 1.4-48.9, p = 0.02). Using PCA, preoperative LP shape PC1 scores were different between success and recurrence groups (p = 0.02), with a more dorsally oriented LP shape associated with recurrence.
Conclusions
Larger preoperative levator hiatus at rest and a more dorsally oriented levator plate shape were associated with prolapse recurrence at long-term follow-up. For every 1 cm increase in preoperative resting levator hiatus, the odds of long-term prolapse recurrence increases 8-fold.





Similar content being viewed by others
Change history
22 September 2022
A Correction to this paper has been published: https://doi.org/10.1007/s00192-022-05369-1
References
Boyles SH, Weber AM, Meyn L. Procedures for pelvic organ prolapse in the United States, 1979-1997. Am J Obstet Gynecol. 2003;188(1):108–15. https://doi.org/10.1067/mob.2003.101.
Wu JM, Kawasaki A, Hundley AF, Dieter AA, Myers ER, Sung VW. Predicting the number of women who will undergo incontinence and prolapse surgery, 2010 to 2050. Am J Obstet Gynecol. 2011;205(3):230 e231–5. https://doi.org/10.1016/j.ajog.2011.03.046.
Larson KA, Smith T, Berger MB, Abernethy M, Mead S, Fenner DE, et al. Long-term patient satisfaction with Michigan four-wall sacrospinous ligament suspension for prolapse. Obstet Gynecol. 2013;122(5):967–75. https://doi.org/10.1097/AOG.0b013e3182a7f0d5.
Miedel A, Tegerstedt G, Morlin B, Hammarstrom M. A 5-year prospective follow-up study of vaginal surgery for pelvic organ prolapse. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19(12):1593–601. https://doi.org/10.1007/s00192-008-0702-z.
Fialkow MF, Newton KM, Weiss NS. Incidence of recurrent pelvic organ prolapse 10 years following primary surgical management: a retrospective cohort study. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19(11):1483–7. https://doi.org/10.1007/s00192-008-0678-8.
Abdel-Fattah M, Familusi A, Fielding S, Ford J, Bhattacharya S. Primary and repeat surgical treatment for female pelvic organ prolapse and incontinence in parous women in the UK: a register linkage study. BMJ Open. 2011;1(2):e000206. https://doi.org/10.1136/bmjopen-2011-000206.
Olsen AL, Smith VJ, Bergstrom JO, Colling JC, Clark AL. Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol. 1997;89(4):501–6. https://doi.org/10.1016/S0029-7844(97)00058-6.
Nygaard I, Brubaker L, Zyczynski HM, Cundiff G, Richter H, Gantz M, et al. Long-term outcomes following abdominal sacrocolpopexy for pelvic organ prolapse. JAMA. 2013;309(19):2016–24. https://doi.org/10.1001/jama.2013.4919.
Friedman T, Eslick GD, Dietz HP. Risk factors for prolapse recurrence: systematic review and meta-analysis. Int Urogynecol J. 2018;29(1):13–21. https://doi.org/10.1007/s00192-017-3475-4.
Vergeldt TF, van Kuijk SM, Notten KJ, Kluivers KB, Weemhoff M. Anatomical cystocele recurrence: development and internal validation of a prediction model. Obstet Gynecol. 2016;127(2):341–7. https://doi.org/10.1097/AOG.0000000000001272.
Weemhoff M, Shek KL, Dietz HP. Effects of age on levator function and morphometry of the levator hiatus in women with pelvic floor disorders. Int Urogynecol J. 2010;21(9):1137–42. https://doi.org/10.1007/s00192-010-1150-0.
Vaughan MH, Siddiqui NY, Newcomb LK, Weidner AC, Kawasaki A, Visco AG, et al. Surgical alteration of genital hiatus size and anatomic failure after vaginal vault suspension. Obstet Gynecol. 2018;131(6):1137–44. https://doi.org/10.1097/AOG.0000000000002593.
Berger MB, Kolenic GE, Fenner DE, Morgan DM, DeLancey JOL. Structural, functional, and symptomatic differences between women with rectocele versus cystocele and normal support. Am J Obstet Gynecol. 2018;218(5):510 e511–8. https://doi.org/10.1016/j.ajog.2018.01.033.
Bump RC, Mattiasson A, Bo K, Brubaker LP, DeLancey JO, Klarskov P, et al. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol. 1996;175(1):10–7.
Trowbridge ER, Fultz NH, Patel DA, DeLancey JO, Fenner DE. Distribution of pelvic organ support measures in a population-based sample of middle-aged, community-dwelling African American and white women in southeastern Michigan. Am J Obstet Gynecol. 2008;198(5):548 e541–6. https://doi.org/10.1016/j.ajog.2008.01.054.
Larson KA, Hsu Y, Chen L, Ashton-Miller JA, DeLancey JO. Magnetic resonance imaging-based three-dimensional model of anterior vaginal wall position at rest and maximal strain in women with and without prolapse. Int Urogynecol J. 2010;21(9):1103–9. https://doi.org/10.1007/s00192-010-1161-x.
Hsu Y, Summers A, Hussain HK, Guire KE, Delancey JO. Levator plate angle in women with pelvic organ prolapse compared to women with normal support using dynamic MR imaging. Am J Obstet Gynecol. 2006;194(5):1427–33. https://doi.org/10.1016/j.ajog.2006.01.055.
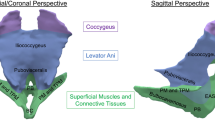
Huebner M, DeLancey JOL. Levels of pelvic floor support: what do they look like on magnetic resonance imaging? Int Urogynecol J. 2019;30(9):1593–5. https://doi.org/10.1007/s00192-019-03986-x.
Reiner CS, Williamson T, Winklehner T, Lisse S, Fink D, DeLancey JOL, et al. The 3D pelvic inclination correction system (PICS): a universally applicable coordinate system for isovolumetric imaging measurements, tested in women with pelvic organ prolapse (POP). Comput Med Imaging Graph. 2017;59:28–37. https://doi.org/10.1016/j.compmedimag.2017.05.005.
Rasband W. ImageJ. Bethesda: National Institute of Mental Health; 1997.
Berger MB, Morgan DM, DeLancey JO. Levator ani defect scores and pelvic organ prolapse: is there a threshold effect? Int Urogynecol J. 2014;25(10):1375–9. https://doi.org/10.1007/s00192-014-2388-8.
Betschart C, Chen L, Ashton-Miller JA, Delancey JO. On pelvic reference lines and the MR evaluation of genital prolapse: a proposal for standardization using the pelvic inclination correction system. Int Urogynecol J. 2013;24(9):1421–8. https://doi.org/10.1007/s00192-013-2100-4.
Hotelling H. Analysis of complex statistical variables into principal components. J Educ Psychol. 1933;24(6):417–41. https://doi.org/10.1037/h0071325.
DeLancey JO, Morgan DM, Fenner DE, Kearney R, Guire K, Miller JM, et al. Comparison of levator ani muscle defects and function in women with and without pelvic organ prolapse. Obstet Gynecol. 2007;109(2 Pt 1):295–302. https://doi.org/10.1097/01.AOG.0000250901.57095.ba.
Bradley MS, Askew AL, Vaughan MH, Kawasaki A, Visco AG. Robotic-assisted sacrocolpopexy: early postoperative outcomes after surgical reduction of enlarged genital hiatus. Am J Obstet Gynecol. 2018;218(5):514 e511–8. https://doi.org/10.1016/j.ajog.2018.01.046.
Vakili B, Zheng YT, Loesch H, Echols KT, Franco N, Chesson RR. Levator contraction strength and genital hiatus as risk factors for recurrent pelvic organ prolapse. Am J Obstet Gynecol. 2005;192(5):1592–8. https://doi.org/10.1016/j.ajog.2004.11.022.
Medina CA, Candiotti K, Takacs P. Wide genital hiatus is a risk factor for recurrence following anterior vaginal repair. Int J Gynaecol Obstet. 2008;101(2):184–7. https://doi.org/10.1016/j.ijgo.2007.11.008.
Vergeldt TF, Notten KJ, Weemhoff M, van Kuijk SM, Mulder FE, Beets-Tan RG, et al. Levator hiatal area as a risk factor for cystocele recurrence after surgery: a prospective study. BJOG. 2015;122(8):1130–7. https://doi.org/10.1111/1471-0528.13340.
Rodrigo N, Wong V, Shek KL, Martin A, Dietz HP. The use of 3-dimensional ultrasound of the pelvic floor to predict recurrence risk after pelvic reconstructive surgery. Aust N Z J Obstet Gynaecol. 2014;54(3):206–11. https://doi.org/10.1111/ajo.12171.
Wyman AM, Rodrigues AA Jr, Hahn L, Greene KA, Bassaly R, Hart S, et al. Estimated levator ani subtended volume: a novel assay for predicting surgical failure after uterosacral ligament suspension. Am J Obstet Gynecol. 2016;214(5):611 e611–6. https://doi.org/10.1016/j.ajog.2015.11.005.
Swenson CW, Masteling M, DeLancey JO, Nandikanti L, Schmidt P, Chen L. Aging effects on pelvic floor support: a pilot study comparing young versus older nulliparous women. Int Urogynecol J. 2020;31(3):535–43. https://doi.org/10.1007/s00192-019-04063-z.
Sammarco AG, Nandikanti L, Kobernik EK, Xie B, Jankowski A, Swenson CW, et al. Interactions among pelvic organ protrusion, levator ani descent, and hiatal enlargement in women with and without prolapse. Am J Obstet Gynecol. 2017;217(5):614 e611–7. https://doi.org/10.1016/j.ajog.2017.07.007.
Andrew BP, Shek KL, Chantarasorn V, Dietz HP. Enlargement of the levator hiatus in female pelvic organ prolapse: cause or effect? Aust N Z J Obstet Gynaecol. 2013;53(1):74–8. https://doi.org/10.1111/ajo.12026.
Funding
CWS received research support from the National Institutes of Health, grants #R03 HD096189 and #K12 HD065257. LC received research support from the National Institute of Health, grant #R21 HD079908. The original studies from which the MRIs were obtained were funded by the National Institutes of Health, grants #R01 HD038665 and #R01 HD044406.
Author information
Authors and Affiliations
Contributions
P Schmidt: data collection or management, data analysis, manuscript writing/editing.
L Chen: protocol/project development, data collection or management, data analysis, manuscript writing/editing.
JO DeLancey: protocol/project development, data collection or management, data analysis, manuscript writing/editing.
CW Swenson: protocol/project development, data collection or management, data analysis, manuscript writing/editing.
Corresponding author
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Schmidt, P., Chen, L., DeLancey, J.O. et al. Preoperative level II/III MRI measures predicting long-term prolapse recurrence after native tissue repair. Int Urogynecol J 33, 133–141 (2022). https://doi.org/10.1007/s00192-021-04854-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-021-04854-3