Abstract
Introduction and hypothesis
The objective was to assess whether telemedicine-based follow-up is equivalent to office-based follow-up in the early postoperative period after routine synthetic midurethral sling placement.
Methods
This is a prospective, international, multi-institutional, randomized controlled trial. Patients undergoing synthetic midurethral sling placement were randomized to 3-week postoperative telemedicine versus office-based follow-up. The primary outcome was the rate of unplanned events. Secondary outcomes included patient satisfaction, crossover from telemedicine to office-based follow-up, and compliance with 3- to 5-month office follow-up.
Results
We included 238 patients (telemedicine: 121 vs office: 117). No differences in demographics or medical comorbidities were noted between the study groups (p = 0.09–1.0). No differences were noted in unplanned events: hospital admission, emergency department visit, or unplanned office visit or call (14% vs 12.9%, p = 0.85) or complications (9.9% vs 8.6%, p = 0.82). Both groups were equally “very satisfied” with their surgical outcomes (71.1% vs 69%, p = 0.2). Telemedicine patients were more compliant with 3- to 5-month office follow-up (90.1% vs 79.3%, p = 0.04).
Conclusions
After synthetic midurethral sling placement, telemedicine follow-up is a safe patient communication option in the early postoperative period. Telemedicine patients reported no difference in satisfaction compared with office-based follow-up but had greater compliance with 3- to 5-month follow-up.
Similar content being viewed by others
Introduction
The synthetic midurethral sling (MUS) is one of the most common procedures performed and, arguably, one of the most widely studied stress urinary incontinence (SUI) interventions. Long-term data indicate that MUS is effective and has a low risk of complications [1]. The American Urological Association (AUA) guidelines for SUI dictate that physicians should communicate with the patient early in the postoperative period to screen for complications, and that the patient should be evaluated in-person within 6 months of surgery [1]. In a modern cohort of 396 patients who underwent a variety of female pelvic reconstructive surgeries, approximately 30% (125 out of 396) of patients had a postoperative complication, with the majority (66%) identified in the first few weeks after surgery [2]. Mueller and colleagues [2] thus indicated that the early postoperative visit may be the most important. Yet when a group in the UK looked retrospectively at those patients who specifically underwent MUS for primary SUI followed only by telemedicine, just 10% (28 out of 262) required conversion to office-based follow-up in the early postoperative period, indicating a low risk of missed complications with this method of follow-up [3].
Telemedicine is an evolving area of medicine that has the potential to reduce cost, travel time, wait times, while increasing patient satisfaction and maintaining the quality of care received [3, 4]. In the era of COVID-19 and variable restrictions on seeing patients in the office, telemedicine has gained an ever-increasing role in providing healthcare when in-person visits are not possible. It is being applied across specialties and in a wide range of settings. The technology utilized for telemedicine encounters can range from telephone-based interviews to video visits using mobile applications to remote controlled telemedicine robots [5,6,7]. Its use in lieu of a postoperative office-based visit has been shown to have excellent patient satisfaction with minimal complications following routine cholecystectomy or hernia repair [3, 4]. In patients specifically undergoing surgery for pelvic floor disorders, initial single-center prospective randomized data indicated that there was no difference in adverse effects or unplanned visits to primary care or the emergency room [8]. Thus, the purpose of this study is to evaluate in a prospective multi-institutional manner whether telemedicine postoperative follow-up is equivalent to office-based follow-up in the early postoperative period after routine synthetic MUS placement with regard to complications, unplanned events, and patient-reported satisfaction.
Materials and methods
This international, multi-institutional, randomized control trial was conducted at six centers in four countries (Brazil, China, Italy, and USA). Patients who were undergoing primary MUS placement for SUI or stress-predominant mixed urinary incontinence were prospectively recruited between January 2018 and May 2019. Exclusion criteria included: urgency-predominant mixed urinary incontinence, concomitant pelvic surgery, voiding dysfunction, chronic pain or urethral diverticulum. This study was approved by the Institutional Review Board at each institution; data use agreements to transfer information were also obtained.
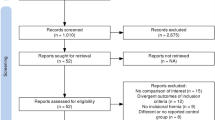
All patients received a synthetic MUS, performed in a same-day surgery setting by a urologist who was specialized in pelvic reconstructive surgery. Sling type, retropubic or transobturator, and product used were at the discretion of the surgeon. Patients were enrolled preoperatively; informed consent was obtained and patients were randomized 1:1 by coin flip to telemedicine-based follow-up (TBFU) or standard office-based follow-up (OBFU) for the short-term postoperative visit (Fig. 1). The coin flip is an accepted method of simple randomization for studies having over 200 subjects and was used for ease of standardization across multiple institutions and continents [9]. Blinding was not possible as participants needed to be informed for discharge planning. The patient’s perioperative course was otherwise unaltered from the standard at each institution. All patients received a well-being phone call within 2–4 days after surgery. The randomized short-term follow-up was performed between 2 and 6 weeks postoperatively. At this interval, patients in both groups answered a standard question set with a focused review of systems and symptom review, including assessment for any obstructive voiding symptoms or other known complications specific to MUS. The short-term follow-up visit, regardless of modality, was completed by the surgeon or the advanced practice provider (Physician Assistant or Nurse Practitioner) experienced in evaluating postoperative patients for the surgeon. TBFU could be completed through a telephone interview or a video visit through mobile application technology and was done using a standardized script (Appendix 1). OBFU group also underwent a focused physical examination, urinalysis, and ultrasound postvoid residual volume assessment, as part of the current standard for postoperative visits, per AUA guidelines [1], and followed a standardized script as well (Appendix 2).
Patients who had self-reported concerns about their recovery or reported clinically concerning symptoms on the well-being phone call or TBFU were referred at the discretion of the treating provider for urine analysis and/or office-based visit. These situations were reported as “unplanned events” if they occurred prior to follow-up or a “crossover” if the physician requested an office visit instead of the 2- to 6-week TBFU. Patient-requested crossover from TBFU to OBFU was also permitted. Regardless of the randomization group, postoperative office-based follow-up at 3–5 months was scheduled for all patients. At this visit patients completed a postoperative surgical satisfaction questionnaire (SSQ-8) and underwent a physical examination including postvoid residual evaluation [10]. The satisfaction survey had patients rate their level of satisfaction on a scale of “very unsatisfied” to “very satisfied” in areas of pain control, return to activities/work/exercise, surgical results, and follow-up [10].
The primary outcome included the rate of unplanned events postoperatively and the rate of complications detected, each based on follow-up type. Unplanned events were defined as interactions with healthcare providers outside expected follow-up within the first 30 days of surgery, which included phone calls, office or emergency room visits, or hospital admissions. Complications following MUS were defined as consequences that occurred anytime between the day of surgery and the final office follow-up including urinary retention requiring sling incision, mesh exposure, urinary tract infection (UTI), deep vein thrombosis (DVT), bleeding event such as hematoma formation, bowel or nerve injury. We hypothesized that TBFU would experience higher rates of unplanned phone calls, office visits, or emergency room visits owing to unaddressed concerns usually mitigated on an office visit that would not be detected with a TBFU. Secondary outcomes were patient-reported satisfaction, crossover from TBFU to OBFU at patient or physician request, and compliance with 3- to 5-month OBFU.
We calculated sample size with a power calculation based on two independent samples with dichotomous outcomes. We assume a higher rate of unplanned events in telemedicine (30%) versus office-based follow-up (15%). This is calculated by estimating a complication rate of 15% for lower urinary tract manipulation based on our own institutional data for both groups [10, 11]. We estimate an additional 10% incidence of unplanned office visits [3], and a 5% incidence of unplanned telephone follow-up for the telemedicine-based group. For 80% power and a 0.05 significance level, a sample size of 240 was calculated, with 120 assigned to each arm.
Statistical calculations were completed using SPSS® version 26 (IBM, Armonk, NY, USA). Descriptive statistics are presented as mean ± standard deviation (STD) or percentages for continuous and categorical variables respectively. Continuous variables were compared using the paired Student’s t test, and categorical variables with the Fisher’s exact test. Univariate, multivariate, and ordinal logistic regression analyses were used for telemedicine subgroup evaluation of satisfaction and crossover. For all comparisons, statistical significance was set at p < 0.05.
Results
In total, 243 patients were recruited and randomized. Five patients were excluded after enrollment: 4 owing to drop-out prior to the 2- to 6-week follow-up and 1 because of an incidental bladder mass discovered during the procedure. A total of 238 patients were included in the analysis, 121 in the TBFU group and 117 in the OBFU group. Twenty-seven patients were included from Italy, 22 from Brazil, 112 from China across two sites, and 77 from the USA across two sites. Patient demographics (Table 1) indicate that the groups were similar with regard to age, race, comorbidities, indication for surgery, and surgical history. Mean age was 56 years (SD: 11.6) and the cohort primarily consisted of Asian (49%) or non-Hispanic white (44.6%) patients. The majority of patients were undergoing MUS for SUI, 75% (179 out of 238), with the majority receiving retropubic MUS, 78% (187 out of 238).
The total number of postoperative complications detected was 9% (22 out of 238) with 90.9% (20 out of 22) of the complications consisting of postoperative urinary tract infections. The total number of patients that had an unplanned event was 13% (32 out of 238). The majority of those events were unplanned phone calls to the office. There was no significant difference in the complication rate or rate of unplanned events between the groups (Table 2). One patient in the telemedicine group underwent an additional operation for sling incision.
The majority of patients (86.5%; 206 out of 238) indicated that they were “satisfied” or “very satisfied” with the results of their surgery. Additionally, 85% (203 out of 238) were “satisfied” or “very satisfied” with their postoperative follow-up. Between groups, there was no significant difference in any category of the surgical satisfaction questionnaire (Table 3). A subset analysis of those patients “very satisfied” with follow-up in the TBFU group revealed that race, education level, and tobacco use were significant variables in univariate analysis. The rate of cross-over from TBFU to OBFU was 13.2% (16 out of 121). In a subset analysis, age and complication rate were significant predictors of crossover on both univariate and multivariate analysis (p = 0.04, OR: 3.31 (95% CI: 1.10–9.94), and p < 0.01, OR: 6.36 (95% CI: 1.72–23.5) respectively). Conclusions are limited because of the small sample size of the crossover group.
Both groups were highly compliant with follow-up. Compliance rates for the 2- to 6-week visit were 96.6% (117 out of 121) for TBFU compared with 96.5% (112 out of 116) for the OBFU. TBFU patients were more compliant with 3- to 5-month office-based follow-up: 90.1% (109 out of 121) vs 79.3% (92 out of 116; p = 0.03).
Discussion
This prospective, randomized control study demonstrates that incorporating telemedicine into short-term follow-up after MUS placement results in no difference to the rate of unplanned events or complications in the early postoperative period. The patient outcomes achieved are comparable with those of previously published literature, with a low complication rate (<10%), including a very low rate of postprocedure urinary retention (<1%) with short-term follow-up [12, 13]. Additionally, the high satisfaction rate with surgical results (>85%) is consistent with previous literature [14].
Given that the MUS complication rate is generally expected to be low, we aimed to capture the full scope of postoperative outcomes with the inclusion of unplanned events. We hypothesized that TBFU would have higher rates of unplanned events, but this was shown to be false. This argues that telemedicine delivers care of similar quality to office follow-up. We also had a limited number of patients cross over from TBFU to OBFU, which further supports our conclusion that equivalent care was delivered to both groups. Predictors of crossover were age and complications. We theorize that this may be related to the comfort level of older patients with technology and telemedicine in general. Additionally, patients who perceive that they are having a complication may feel that their concern is better resolved by an in-person visit.
Furthermore, patients in either study arm were found to be equally satisfied with their postoperative experience as well as the surgical outcome. In the TBFU group, nonwhite patients and those without a college-level education were more likely to respond “very satisfied” in their surveys. Given that within this sample, race correlates strongly with nationality, we suggest this finding to be a reflection of cultural differences compared with medical practice in different parts of the globe, particularly as it relates to patient expectations and the doctor–patient relationship. We also propose that a difference in patient expectations or health literacy may have influenced the differences between groups with regard to education level as well.
Given the scope and international design of our study, we were unable to accurately address the cost benefits of TBFU. However, there is a growing body of literature demonstrating that utilization of telemedicine is cost saving, time saving, and preferred by patients. S Ballester et al. have suggested that TBFU saves patients an average of 2.4 h and 124 driving miles to seek care at a tertiary referral center while freeing physician clinic hours [14, 15]. Others have associated telemedicine benefits with a cost-saving value of US$124 for initial visits [8] and have shown that when given the choice, the vast majority of patients (98%) chose telemedicine-based follow-up [15]. Given that the institutions involved in our study were also tertiary care centers, we assume that the patients and physicians have received a similar benefit. In fact, our perception of why TBFU increased the compliance with the 3- to 5-month office-based follow-up is related to time saved. We assume that patients are more willing to take the time to present to the office at this longer interval owing to their “saved time,” resulting from an earlier TBFU visit. Time saved can be related to many factors including hours requested off from work for the patient or their family members caring for them, transportation arrangements, travel time, and waiting to be seen in the office. Anecdotally, many patients randomized to the OBFU were disappointed that they were unable to have a TBFU.
The use of telephone follow-up for postoperative female pelvic surgery has been the subject of recently published prospective studies. Thompson et al. [8] prospectively randomized 100 patients who underwent pelvic surgery at a single institution to telephone vs OBFU for the 3-month postoperative visit. Thompson and colleagues [8] focused on patient satisfaction. Overall satisfaction was similar in the two groups, except with regard to surgeon communication—the telephone group was inferior. They hypothesized that this was due to the telephone follow-up being completed by a nurse instead of the surgeon. Balzarro et al. prospectively evaluated 215 SUI patients in a nonrandomized fashion with serial telephone follow-up and then with OBFU at approximately 1 year after MUS. They found a high concordance between telephone and OBFU, except for when distinguishing de novo urge incontinence from recurrent SUI; however, conclusions were limited by the fact that was no control group and that telephone follow-up was performed by residents [16]. Our study builds on this previous work, notably by directly comparing TBFU with the standard of care OBFU and evaluating objective as well as patient-reported outcomes.
Telemedicine has increasingly been used in the era of COVID-19 by many doctors and surgeons to provide quality care while maintaining proper safety precautions. Grimes et al. published guidelines in April 2020 outlining guidance and specifically mentioning the safety of TBFU in postoperative asymptomatic MUS patients [17]. This study adds to the existing literature supporting the use of telemedicine in this patient population.
The multi-institutional and international nature of this study is a strength that to our knowledge no previous prospective study in this area has achieved. Incorporating the practice standards of six institutions from four continents into one study allows the generalizability of our results to a more global setting. We also looked at both complications and satisfaction to fully understand the feasibility of applying TBFU to practice. There are limitations to this study as well. Although all attempts were made to capture outcomes of the patients involved in this study, it is possible that patients in these tertiary care hospitals received care at an outside hospital, which was not reported to the primary surgeon. Thus, we may be underestimating our unplanned events. Additionally, as this study took place at several institutions, we were not able to capture how many patients were invited to be part of this study and declined participation. Thus, the cohort may contain a selection bias, as patients who would not be comfortable with telemedicine likely declined participation. Overall, the large sample size and multi-institutional nature of the study make these conclusions generalizable to all practice types that perform MUS for SUI.
Conclusions
Following a synthetic MUS, TBFU is a safe and feasible option with which to follow-up with patients in the early postoperative period. Compared to traditional OBFU, TBFU portends no difference in complications or unplanned events. Patients were equally satisfied with both their postoperative experience and surgical outcome.
References
Koshiba K, Miki M, Terachi T, Uchida T. Treatment of benign prostatic hyperplasia. Tokyo: Springer; 2000.
Mueller MG, Elborno D, Davé BA, Leader-Cramer A, Lewicky-Gaupp C, Kenton K. Postoperative appointments: which ones count? Int Urogynecol J. 2016;27(12):1873–7. https://doi.org/10.1007/s00192-016-3052-2.
Jefferis H, Muriithi F, White B, Price N, Jackson S. Telephone follow-up after day case tension-free vaginal tape insertion. Int Urogynecol J. 2016;27(5):787–90.
Hwa K, Wren SM. Telehealth follow-up in lieu of postoperative clinic visit for ambulatory surgery: results of a pilot program. JAMA Surg. 2013;148(9):823–7.
Goss S, Stevens C. Making research matter: researching for change in the theory and practice of counselling and psychotherapy. London: Routledge; 2015.
Miller A, Rhee E, Gettman M, Spitz A. The current state of telemedicine in urology. Med Clin North Am. 2018;102(2):387–98. https://doi.org/10.1016/j.mcna.2017.10.014.
Jimènez Torres M, Beitl K, Hummel Jimènez J, Mayer H, Zehetmayer S, Umek W, et al. Benefit of a nurse-led telephone-based intervention prior to the first urogynecology outpatient visit: a randomized-controlled trial. Int Urogynecol J. 2020; https://doi.org/10.1007/s00192-020-04318-0.
Thompson JC, Cichowski SB, Rogers RG, Qeadan F, Zambrano J, Wenzl C, et al. Outpatient visits versus telephone interviews for postoperative care: a randomized controlled trial. Int Urogynecol J. 2019;30:1639–1646. https://doi.org/10.1007/s00192-019-03895-z.
Suresh K. An overview of randomization techniques: an unbiased assessment of outcome in clinical research. J Hum Reprod Sci. 2011;4(1):8–11.
Haff RE, Stoltzfus J, Lucente VR, Murphy M. The surgical satisfaction questionnaire (SSQ-8): a validated tool for assessment of patient satisfaction following surgery to correct prolapse and/or incontinence. J Minim Invasive Gynecol. 2011;18(6):S49–S50. https://doi.org/10.1097/WON.0000000000000548
Derisavifard S, Giusto L, Zahner P, Rueb J, Goldman HB. Safety of intradetrusor onabotulinumtoxinA (BTX-A) injection in the asymptomatic patient with a positive urine dip. Urology. 2020;135:38–43 https://doi.org/10.1016/j.urology.2019.09.030.
Nitti VW. Complications of midurethral slings and their management. Can Urol Assoc J. 2012;6(5 Suppl 2):S120–S122. https://doi.org/10.1016/j.urology.2019.09.030
Ford AA, Rogerson L, Cody JD, Aluko P, Ogah JA. Mid-urethral sling operations for stress urinary incontinence in women. Cochrane Database Syst Rev. 2017;7(7):CD006375. https://doi.org/10.1002/14651858.CD006375.pub4
Richter HE, Albo ME, Zyczynski HM, Kenton K, Norton PA, Sirls LT, et al. Retropubic versus transobturator midurethral slings for stress incontinence. N Engl J Med. 2010;362:2066–2076. https://doi.org/10.1056/nejmoa0912658.
Soegaard Ballester JM, Scott MF, Owei L, Neylan C, Hanson CW, Morris JB. Patient preference for time-saving telehealth postoperative visits after routine surgery in an urban setting. Surgery. 2018;163(4):672–679. https://doi.org/10.1016/j.surg.2017.08.015.
Balzarro M, Rubilotta E, Trabacchin N, Mancini V, Costantini E, Artibani W, et al. A prospective comparative study of the feasibility and reliability of telephone follow-up in female urology: the patient Home Office novel evaluation (PHONE) study. Urology. 2020;136:82-87. https://doi.org/10.1016/j.urology.2019.10.021.
Grimes CL, Balk EM, Crisp CC, Antosh DD, Murphy M, Halder GE, et al. A guide for urogynecologic patient care utilizing telemedicine during the COVID-19 pandemic: review of existing evidence. Int Urogynecol J. 2020;31(6):1063–1089.
Acknowledgements
Courtenay Moore MD, Cleveland Clinic, Cleveland, OH, USA (surgeon); Raymond Rackley MD, Cleveland Clinic, Cleveland, OH, USA (surgeon); Sandip Vasavada MD, Cleveland Clinic, Cleveland, OH, USA (surgeon); Kathleen Scott PA, Cleveland Clinic, Cleveland, OH, USA (patient recruitment and follow-up); Elizabeth Stark PA, Cleveland Clinic, Cleveland, OH, USA (patient recruitment and follow-up); Elodi Dielubanza MD, Cleveland Clinic, Cleveland, OH, USA (protocol development); Xu Lei PA, Renji Hospital, Shanghai, China (patient recruitment and follow-up); Fang Weilin MD, Renji Hospital, Shanghai, China (surgeon).
Author information
Authors and Affiliations
Contributions
L.L. Giusto: project development, data collection, data analysis, manuscript writing; S. Derisavifard: project development, data collection, data analysis, manuscript writing; P.M. Zahner: project development, data collection, data analysis, manuscript writing; J.J. Rueb: project development, data collection, data analysis, manuscript writing; L. Deyi: project development, data collection; L. Jiayi: project development, data collection; R. Moreira: project development, data collection; A. Gomelsky: project development, data collection; M. Balzarro: project development, data collection; H.B. Goldman: project development, data collection, data analysis, manuscript writing.
Corresponding author
Ethics declarations
Conflicts of interest
Laura L. Giusto, Samir Derisavifard, Patricia M. Zahner, Jessica J. Rueb, Luo Deyi, Li Jiayi, Fang Weilin, Raphael de Jesus Moreira, Alexander Gomelsky, Matteo Balzarro: NONE. Howard B. Goldman: Allergan, Medtronic, Laborie, Sacramed, Bluewind, Astellas, Boston Scientific, Bioness, Cook Myosite.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix 1
(2–6 weeks postoperatively) Phone or telemedicine follow–up provider data sheet
Date of surgery:
Date of call/telemedicine visit:
Visit type: telemedicine or phone call
Sling type (i.e., transobturator, retropubic):
Sling trade name:
Primary sling or revision?
Diagnosis: 1) stress urinary incontinence; 2) stress-predominant mixed urinary incontinence; 3) recurrent stress urinary incontinence.
Review of systems
(Circle all that apply)
-
1.
General: fever/malaise/weight loss/other
Details:
-
2.
Cardiovascular: chest pain/shortness of breath/palpitations/edema
Details:
-
3.
Respiratory: chronic cough/wheezing/shortness of breath/other
Details:
-
4.
Neurological: numbness/tingling/pain/other
Details:
-
5.
Gastrointestinal: constipation/diarrhea/fecal incontinence
Details:
Symptoms
-
1.
Stress urinary incontinence: 1) none; 2) minimal; 3) mild; 4) significant, but improved; 5) no improvement; 6) worse
-
2.
Urgency incontinence: 1) none; 2) minimal; 3) mild; 4) significant, but improved; 5) no improvement; 6) worse
-
3.
Urgency: 1) none; 2) minimal; 3) mild; 4) significant, but improved; 5) no improvement; 6) worse
-
4.
Frequency: 1) normal; 2) improved; 3) no change every ___ hours
-
5.
Nocturia: 1) normal; 2) improved; 3) no change; #voids/night:
-
6.
Force of stream: 1) the same; 2) better; 3) a little slower; 4) a lot slower. Strength of stream compared to preoperatively?________%
-
7.
Straining or pushing to void? Yes/no
-
8.
Incomplete emptying? Yes/no
-
9.
UTI before surgery? Yes/no; # in the last 12 months:
-
10.
UTI postoperatively? Yes/no; # since surgery:
Sexual activity
-
1.
Sexually active before surgery? Yes/no
Abstinence reason: 1) relationship status; 2) incontinence; 3) discomfort/pain; 4) partner dysfunction/issues
-
2.
Sexually active after surgery? Active/not active
If active:
Pain with intercourse? Yes/no
Better or worse or same compared with preoperatively?
Partner reports pain/scratching? Yes/no
Patient questions or concerns? (Specify)
Provider notes:
-
1.
Additional testing, medication change, or refill given? Yes/no If yes, specify:
-
2.
Patient or provider requests office-based follow-up? Yes/no
If yes, please provide reason:
Appendix 2
3–5 months universal office follow-up provider data collection form
Date of surgery:
Date of visit:
Surgeon:
Sling type (i.e., transobturator, retropubic):
Sling trade name:
Primary sling or revision?
Diagnosis: 1) stress urinary incontinence; 2) stress-predominant mixed urinary incontinence; 3) recurrent stress urinary incontinence
Review of systems
(Circle all that apply)
-
6.
General: fever/malaise/weight loss/other
Details:
-
7.
Cardiovascular: chest pain/shortness of breath/palpitations/edema
Details:
-
8.
Respiratory: chronic cough/wheezing/shortness of breath/other
Details:
-
9.
Neurological: numbness/tingling/pain/other
Details:
-
10.
Gastrointestinal: constipation/diarrhea/fecal incontinence
Details:
Symptoms
-
11.
Stress urinary incontinence: 1) none; 2) minimal; 3) mild; 4) significant, but improved; 5) no improvement; 6) worse
-
12.
Urgency incontinence: 1) none; 2) minimal; 3) mild; 4) significant, but improved; 5) no improvement; 6) worse
-
13.
Urgency: 1) none; 2) minimal; 3) mild; 4) significant, but improved; 5) no improvement; 6) worse
-
14.
Frequency: 1) normal; 2) improved; 3) no change; every ___ hours
-
15.
Nocturia: 1) normal; 2) improved; 3) no change; #voids/night:
-
16.
Force of stream: 1) the same; 2) better; 3) a little slower; 4) a lot slower. Strength of stream compared with preoperatively? ___%
-
17.
Straining or pushing to void? Yes/No
-
18.
Incomplete emptying? Yes/No
-
19.
UTI before surgery? Yes/No. # in the last 12 months:
-
20.
UTI postoperatively? Yes/No. # since surgery:
Sexual activity
-
1.
Sexually active before surgery? Yes/No
Abstinence reason: 1) relationship status; 2) incontinence; 3) discomfort/pain; 4) partner dysfunction/issues
-
2.
Sexually active after surgery? Active/not active
If active:
Pain with intercourse? Yes/ No
Better or worse or same compared with preoperatively?
Partner reports pain/scratching? Yes/No
Physical examination
Vital signs: BP__________ | Pulse _______ | Temperature _______ | Height_______ |Weight ________ | BMI _______.
General appearance:
Abdomen: soft/nontender/nondistended
Specify if abnormalities:
Neuro/psych: no signs of depression, anxiety, or agitation
Specify if abnormalities:
Extremities: no deformities, edema, clubbing or skin discoloration
Specify if abnormalities:
External genitalia: normal hair distribution, no lesions
Specify if abnormalities:
Vaginal wall: 1) well-healed; 2) healing
1) Mesh palpable; 2) mesh nonpalpable
1) Tender; 2) nontender
Comments:
Incisions: 1) prepubic; 2) inner thigh
1) Well-healed; 2) healing
1) Tender; 2) nontender
Comments:
Mesh extrusion: Yes/No
Comments:
Urethral tenderness: Yes/No
Testing:
Urinalysis:
Postvoid residual:___ mL

How satisfied are you with the follow-up you received postoperatively?
1) Very satisfied; 2) satisfied; 3) neutral; 4) unsatisfied; 5) very unsatisfied
Patient questions or concerns?
(Specify)
Provider notes:
-
3.
Additional testing, medication changes, or refills given? Yes/No; If yes, specify:
Rights and permissions
About this article
Cite this article
Giusto, L.L., Derisavifard, S., Zahner, P.M. et al. Telemedicine follow-up is safe and efficacious for synthetic midurethral slings: a randomized, multi-institutional control trial. Int Urogynecol J 33, 1007–1015 (2022). https://doi.org/10.1007/s00192-021-04767-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-021-04767-1