Abstract
Objectives
The aim of this study was to determine when women are at risk for recurrent pelvic organ prolapse (POP).
Methods
From 2010 to 2018, all women with symptomatic prolapse, Pelvic Organ Prolapse Quantification (pop-Q) stage 2 in at least one compartment and prolapse surgery were included. The primary outcome measure was POP recurrence. Kaplan-Meier estimates were calculated, survival curves were created, and differences in survival curves were tested with log-rank test. Cox proportional hazard regression was used to investigate associations between recurrence and the number and type of involved compartment(s) and type of surgery.
Results
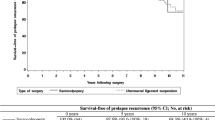
Forty-six (16.8%) out of 274 patients had POP recurrence during a mean follow-up time of 55 ± 32 months. The mean age was 64 ± 12 years. The hazard of recurrence increased the most in the first 2 years after POP surgery, flattened in years 3 and 4 and remained almost stable in the years thereafter, regardless of the site and number of involved compartment(s). The hazard of recurrence over time seemed the largest when all three compartments were involved. However, there was no statistically significant difference in recurrence between the numbers of (p = 0.65) or in the combination of involved compartments (p = 0.19). There was no difference in POP recurrence over time between prolapse repair with either sacrospinous ligament fixation or vaginal hysterectomy (p = 0.48).
Conclusions
Women are at the highest risk of POP recurrence in the first 2 years after POP surgery independent of the number or combination of involved compartment(s).




Similar content being viewed by others
References
Doaee M, Moradi-Lakeh M, Nourmohammadi A. Kazem Ravazi-Ratki S, Nojomi M. management of pelvic organ prolapse and quality of life: a systematic review and meta analysis. Int Urogynecol J. 2014;25:153–63.
Wu JM, Matthews CA, Conover MM, Pate V, Jonsson Funk M. Lifetime risk of stress urinary incontinence or pelvic organ prolapse surgery. Obstet Gynecol. 2014;123(6):1201–6.
Milani A, Damoiseaux A, Inthout J, Kluivers KB, Withagen MIJ. Long-term outcome of vaingal mesh or native tissue in recurrent proalpse: a randomized controlled trial. Int Urogynecol J. 2018;29:847–58.
Dietz HP, Hankins KJ. Wong v. The natural history of cystocele recurrence. Int Urogynecol J. 2014;25:1053–7.
Toozs-Hobson P, Freeman R, Barber M, et al. International Urogynecological Association; International Continence Society. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for reporting outcomes of surgical procedures for pelvic organ prolapse. Neurourol Urodyn. 2012;31(4):415–21.
Price N, Slack A, Jwarah E, Jackson S. The incidence of reoperation for surgically treated pelvic organ prolapse: an 11-year experience. Menopause Int. 2008;14:145–8.
Løwenstein E, Møller LA, Laigaard J, Gimbel H. Reopertation for pelvic organ prolapse: a Danish cohort study woth 15-20 years follow up. Int Urogynecol J. 2018;29:119–24.
Barber MD, Brubaker L, Nygard I, Wheeler IITL, Schaffer J, Chen Z. Spino C for the pelvic floor disorders network. Defining succes after surgery for pelvic organ prolapse. Obstet Gynecol. 2009;114(3):600–9.
Johnson P, Larson KA, Hsu Y, Fenner DE, Morgan D, DeLancy JOL. Self-reported natural history of recurrent prolapse among women presenting to a tertiary center. Int J Gynecol Obstet. 2013;120:53–6.
Pizarro-Berdichevsky J, Borazjani A, Pattilo A, Arellano M, Li J, Goldman HB. Natural history of pelvic organ prolapse in symptomatic patients actively seeking treatment. Int Urogynecol J. 2018;29:873–80.
Utomo E, Blok FB, Steensma AB, Korfage IJ. Validation of the pelvic floor distress inventory (PFDI-20) and pelvic floor impact questionnaire (PFIQ-7) in a Dutch population. Int Urogynecol J. 2014;25:531–44.
van der Vaart CH, de Leeuw JR, Roovers JP, Heintz AP. Measuring health-related quality of life in women with urogenital dysfunction: the urogenital distress inventory and incontinence impact questionnaire revisited. Neurourol Urodyn 2003;22(2):97–104.
Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J. 2010;21(1):5–26.
Haylen BT, Maher CF, Barber MD, Camargo S, Dandolu V, Digesu A, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic organ prolapse (POP). Int Urogynecol J. 2016;27(2):165–94.
Hall AF, Theofrastous JP, Cundiff GW, et al. Interobserver and intraobserver reliability of the proposed International Continence Society, Society of Gynecologic Surgeons, and American Urogynecologic Society pelvic organ prolapse classification system. Am J Obstet Gynecol. 1996;175:1467–70 discussion 1470–1.
Prolaps. NVOG richtlijn, 13 november 2014. www.richtlijndatasbase.nl
R version 3.6.3 (2020-02-29) -- "Holding the Windsock”. Copyright (C) 2020 The R Foundation for Statistical Computing.
Therneau T (2020). A Package for Survival Analysis in R_. R package version 3.1–11, URL: https://CRAN.R-project.org/package=survival.
Harrell Jr FE, with contributions from Charles Dupont, and et al. (2020). Hmisc: Harrell Miscellaneous. R package, version 4.3–1. https://CRAN.R-project.org/package=Hmisc
Bouliotis G, Billinham L. Crossing survival curves: alternatives to the log-rank test. Trials. 2011;12(Suppl 1):A137.
Vergeldt TFM, Weemhoff M, Inthout J, Kluivers KB. Risk factors for pelvic organ prolapse and its recurrence: a systematic review. Int J Urogynecol. 2015;26:1559–73.
Detollenaere RJ, den Boon J, Stekelenburg J, IntHout J, Vierhout ME, Kluivers KB, et al. Sacrospinous hysteropexy versus vaginal hysterectomy with suspension of the uterosacral ligaments in women with uterine prolapse stage 2 or higher: multicentre randomised non-inferiority trial. BMJ. 2015;351:h3717.
Schulten SFM, Detollenaere RJ, Stekenlenburg J, Inthout J, Kluivers KB, Eindhoven HWF. Sacrospinous hysteropexy versus vaginal hysterectomy with uterosacral ligament suspension in women with uterine prolapse stage 2 or higher: observational follow-up of a multicentre randomised trial. BMJ. 2019;366:l5149.
Maher C, Feiner B, Baessler K, Christmann-Schmid C, Haya N, Brown J. Surgery for women with apical vaginal prolapse. Cochrane Database Syst Rev. 2016;10:CD012376. https://doi.org/10.1002/14651858.CD012376.
Mowat A, Maher D, Baessler K, Christmann-Schmid C, Haya N, Maher C. Surgery for women with posterior compartment prolapse. Cochrane Database Syst Rev. 2018;3:CD012975.
Funding
The project was funded by Tergooi Academie. The Tergooi Academie had no role in the design, analysis, and interpretation of the results of this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Roos, E.J., Schuit, E. Timing of recurrence after surgery in pelvic organ prolapse. Int Urogynecol J 32, 2169–2176 (2021). https://doi.org/10.1007/s00192-021-04754-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-021-04754-6



