Abstract
Introduction and hypothesis
Women seeking treatment for pelvic floor disorders (PFD) may have a high prevalence of frailty, which could potentially impact the risks of treatment. The present study was aimed to assess the prevalence of frailty in patients with PFD and additionally to compare post-treatment complications between frail and non-frail patients.
Methods
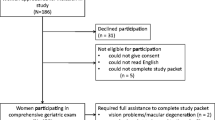
This is a prospective observational study conducted in a single secondary referral centre for PFD. Women with PFD and aged ≥ 65 years were eligible for inclusion. Frailty was classified using a validated screening tool, the Groningen Frailty Indicator (GFI). The primary outcome was to determine the prevalence of frailty in elderly women with symptoms of pelvic floor disorders. Secondary outcomes were clinical outcomes after treatment between frail and non-frail patients.
Results
A total of 263 women were included. The prevalence of frailty was 54.4% (143 women, 95% CI 48.1–60.5) in the studied group of patients. Frail patients had more comorbidities and used more medication compared to non-frail patients. Non-frail patients were more often surgically treated than frail patients. No differences were found in the incidence of postoperative complications.
Conclusions
Our study shows a high prevalence of frailty in elderly women with symptoms of PFD. Further research is required to investigate whether these frail patients face an increased risk of complications and poor clinical outcomes after treatment for PFD.

Similar content being viewed by others
Abbreviations
- PFD:
-
Pelvic floor dysfunction
- GFI:
-
Groningen Frailty Indicator
References
Erekson EA, Fried TR, Martin DK, Rutherford TJ, Strohbehn K, Bynum JP. Frailty, cognitive impairment, and functional disability in older women with female pelvic floor dysfunction. Int Urogynecol J. 2015;26(6):823–30. https://doi.org/10.1007/s00192-014-2596-2.
Gibson W, Athanasopoulos A, Goldman H, Madersbacher H, Newman D, Spinks J, et al. Are we shortchanging frail older people when it comes to the pharmacological treatment of urgency urinary incontinence? Int J Clin Pract. 2014;68:1165–73. https://doi.org/10.1111/ijcp.12447.
Hewitt J, Long S, Carter B, Bach S, McCarthy K, Clegg A. The prevalence of frailty and its association with clinical outcomes in general surgery: a systematic review and meta-analysis. Age Ageing. 2018;47(6):793–800. https://doi.org/10.1093/ageing/afy110.
Hewitt J, Moug SJ, Middleton M, Chakrabarti M, Stechman MJ, McCarthy K. Prevalence of frailty and its association with mortality in general surgery. Am J Surg. 2015;209:254–9. https://doi.org/10.1016/j.amjsurg.2014.05.022.
Goeteyn J, Evans LA, De Cleyn S, Fauconnier S, Damen C, Hewitt J, et al. Frailty as a predictor of mortality in the elderly emergency general surgery patient. Acta Chir Belg. 2017;117:370–5. https://doi.org/10.1080/00015458.2017.1337339.
Anayi AC, Orkaby AR, Sakthivel D, Endo Y, Varon D, Roh D, et al. Impact of frailty on outcomes in surgical patients: a systematic review and meta-analysis. Am J Surg. 2019;218(2):393–400. https://doi.org/10.1016/j.amjsurg.2018.11.020.
Robinson TN, Wallace JI, Wu DS, Wiktor A, Pointer LF, Pfister SM, et al. Accumulated frailty characteristics predict postoperative discharge institutionalisation in the geriatric patient. J Am Coll Surg. 2011;213(1):37–44. https://doi.org/10.1016/j.jamcollsurg.2011.01.056.
Robinson TN, Raeburn CD, Tran ZV, Angles EM, Brenner LA, Moss M. Postoperative delirium in the elderly: risk factors and outcomes. Ann Surg. 2009;249(1):173–8. https://doi.org/10.1097/SLA.0b013e31818e4776.
Erekson EA, Yip SO, Ciarleglio MM, Fried TR. Postoperative complications after gynecologic surgery. Obstet Gynecol. 2011;118(4):785–93. https://doi.org/10.1097/AOG.0b013e31822dac5d.
Smith FJ, Holman CD, Moorin RE, Tsokos N. Lifetime risk of undergoing surgery for pelvic organ prolapse. Obstet Gynecol. 2010;116(5):1096–100. https://doi.org/10.1097/AOG.0b013e3181f73729.
Samuelsson E, Odeberg J, Stenzelius K, Molander U, Hammarström M, Franzen K, et al. Effect of pharmacological treatment for urinary incontinence in the elderly and frail elderly: a systematic review. Geriatr Gerontol Int. 2015;15:521–34. https://doi.org/10.1111/ggi.12451.
Zeno A, Alvarez P, Yazdany T. A systematic review of frailty assessments in women with pelvic floor disorders: are we following the American College of Surgeons National Surgical Quality Improvement Program/American Geriatric Society guidelines? Female Pelvic Med Reconstr Surg. 2018;24(2):135–41. https://doi.org/10.1097/SPV.0000000000000508.
Shinnick JK, Raker CA, Sung V. Provider miscategorisation of frailty in an outpatient urogynecologic population. Int Urogynecol J. 2020;31(8):1529–35. https://doi.org/10.1007/s00192-019-04095-5.
Schuurmans H, Steverink N, Lindenberg S, Frieswijk N, Slaets JP. Old or frail: what tells us more? J Gerontol A Biol Sci Med Sci. 2004;59(9):M962–5. https://doi.org/10.1093/gerona/59.9.m962.
Steverink N, Slaets JPJ, Schuurmans H, van Lis M. Measuring frailty: development and testing of the Groningen frailty indicator (GFI). Gerontologist. 2001;41:236–7.
Drubbel I, Bleijenberg N, Kranenburg G, Eijkemans RJ, Schuurmans MJ, de Wit NJ, et al. Identifying frailty: do the frailty index and Groningen frailty Indicator cover different clinical perspectives? A cross-sectional study. BMC Fam Pract. 2013;14:64. https://doi.org/10.1186/1471-2296-14-64.
Berardelli M, De Rango F, Morelli M, Corsonello A, Mazzei B, Mari V, et al. Urinary incontinence in the elderly and in the oldest old: correlation with frailty and mortality. Rejuvenation Res. 2013;16(3):206–11. https://doi.org/10.1089/rej.2013.1417.
Chen X, Mao G, Leng SX. Frailty syndrome: an overview. Clin Interv Aging. 2014;9:433–41. https://doi.org/10.2147/CIA.S45300.
Chong E, Chan M, Lim WS, Ding YY. Frailty predicts incident urinary incontinence among hospitalized older adults-a 1-year prospective cohort study. J Am Med Dir Assoc. 2018;9(5):422–7. https://doi.org/10.1016/j.jamda.2017.12.103.
Vetrano DL, Palmer KM, Galluzzo L, Giampaoli S, Marengoni A, Bernabei R, et al. Hypertension and frailty: a systematic review and meta-analysis. BMJ Open. 2018;8(12):e024406. https://doi.org/10.1136/bmjopen-2018-024406.
Acknowledgements
The authors thank Sara Baart and Joost van Rosmalen for their supporting roles in the data analysis and Riëlla Bambelt for managing data.
Author information
Authors and Affiliations
Contributions
K de Jong: Data analysis, Data management, Manuscript writing and editing.
MY van der Vlist: Project development, Protocol writing, Data collection, Manuscript editing.
DMJ Oom: Project development, Protocol editing, Manuscript editing.
Corresponding author
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
de Jong, K., van der Vlist, M.Y. & Oom, D.M.J. The prevalence of frailty and post-treatment outcomes in elderly women with pelvic floor disorders. Int Urogynecol J 32, 3001–3006 (2021). https://doi.org/10.1007/s00192-021-04682-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-021-04682-5