Abstract
Introduction and hypothesis
There has been a trend toward the use of ultra-lightweight mesh types for minimally invasive sacrocolpopexy. We hypothesized that ultra-lightweight mesh would have a greater proportion of composite anatomical pelvic organ prolapse recurrence than lightweight mesh.
Methods
Retrospective cohort study of minimally invasive sacrocolpopexies at two academic institutions from 2009 to 2016. Our primary outcome was composite anatomical prolapse recurrence, defined as prolapse beyond the hymen or retreatment with pessary or surgery, compared between ultra-lightweight (≤21 g/m2 [range 19–21]) and lightweight (>21 g/m2 [range 35–50]) mesh types. We assessed time to prolapse recurrence using Kaplan–Meier and Cox regression.
Results
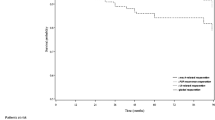
The cohort consisted of 1,272 laparoscopic (n = 530, 41.7%) and robotic-assisted sacrocolpopexies (n = 742, 58.4%). Lightweight mesh was used in 745 procedures (58.6%) and ultra-lightweight mesh in 527 (41.4%). The lightweight mesh had longer median follow-up than the ultra-lightweight group (344 [IQR 50–670] vs 143 days [IQR 44–379], p < 0.01). There was no difference in composite anatomical prolapse recurrence between lightweight and ultra-lightweight mesh (54 [7.2%] vs 35 [6.6%], p = 0.68). Ultra-lightweight mesh demonstrated a shorter time to prolapse recurrence (p < 0.01), which remained significant on multivariate Cox regression (HR 2.38 [95% CI 1.47–3.87]). The lightweight mesh had significantly more mesh complications (43 [5.8%] vs 7 [1.3%], p < 0.01).
Conclusions
Ultra-lightweight mesh for minimally invasive sacrocolpopexy was not associated with a higher proportion of composite anatomical prolapse recurrence; however, it was associated with a shorter time to recurrence. Longer follow-up is needed to assess the clinical importance of this finding, particularly given the trade-off of more complications with lightweight mesh.

Similar content being viewed by others
References
Kenton K, Mueller ER, Tarney C, Bresee C, Anger JT. One-year outcomes after minimally invasive sacrocolpopexy. Female Pelvic Med Reconstr Surg. 2016;22(5):382–4. https://doi.org/10.1097/SPV.0000000000000300.
Mueller MG, Jacobs KM, Mueller ER, Abernethy MG, Kenton KS. Outcomes in 450 women after minimally invasive abdominal sacrocolpopexy for pelvic organ prolapse. Female Pelvic Med Reconstr Surg. 2016;22(4):267–71. https://doi.org/10.1097/SPV.0000000000000269.
Paraiso MF, Jelovsek JE, Frick A, Chen CC, Barber MD. Laparoscopic compared with robotic sacrocolpopexy for vaginal prolapse: a randomized controlled trial. Obstet Gynecol. 2011;118(5):1005–13. https://doi.org/10.1097/AOG.0b013e318231537c.
Liang R, Knight K, Abramowitch S, Moalli PA. Exploring the basic science of prolapse meshes. Curr Opin Obstet Gynecol. 2016;28(5):413–9. https://doi.org/10.1097/GCO.0000000000000313.
Askew AL, Visco AG, Weidner AC, Truong T, Siddiqui NY, Bradley MS. Does mesh weight affect time to failure after robotic-assisted laparoscopic sacrocolpopexy? Female Pelvic Med Reconstr Surg. 2018;26(9):1. https://doi.org/10.1097/SPV.0000000000000632.
Culligan PJ, Lewis C, Priestley J, Mushonga N. Long-term outcomes of robotic-assisted laparoscopic sacrocolpopexy using lightweight Y-mesh. Female Pelvic Med Reconstr Surg. 2020;26(3):202–6. https://doi.org/10.1097/SPV.0000000000000788.
BostonScientific (2015) Upsylon Y-mesh comprehensive mesh specifications Table https://www.sicdsystem.com/content/dam/bostonscientific/uro-wh/portfolio-group/pelvic-floor-reconstruction/y-mesh/upsylon_y_mesh_competitive_comparison_chart.pdf. Accessed 20 October 2020
Barone WR, Moalli PA, Abramowitch SD (2016) Textile properties of synthetic prolapse mesh in response to uniaxial loading. Am J Obstet Gynecol 215 (3):326 e321–329. doi:https://doi.org/10.1016/j.ajog.2016.03.023
Brubaker L, Cundiff GW, Fine P, et al. Abdominal sacrocolpopexy with Burch colposuspension to reduce urinary stress incontinence. N Engl J Med. 2006;354(15):1557–66. https://doi.org/10.1056/NEJMoa054208.
Nygaard I, Brubaker L, Zyczynski HM, Cundiff G, Richter H, Gantz M, Fine P, Menefee S, Ridgeway B, Visco A, Warren LK, Zhang M, Meikle S. Long-term outcomes following abdominal sacrocolpopexy for pelvic organ prolapse. JAMA. 2013;309(19):2016–24. https://doi.org/10.1001/jama.2013.4919.
Anger JT, Mueller ER, Tarnay C, Smith B, Stroupe K, Rosenman A, Brubaker L, Bresee C, Kenton K. Robotic compared with laparoscopic sacrocolpopexy: a randomized controlled trial. Obstet Gynecol. 2014;123(1):5–12. https://doi.org/10.1097/AOG.0000000000000006.
Friedman T, Eslick GD, Dietz HP. Risk factors for prolapse recurrence: systematic review and meta-analysis. Int Urogynecol J. 2018;29(1):13–21. https://doi.org/10.1007/s00192-017-3475-4.
Turner L, Lavelle E, Lowder JL, Shepherd JP. The impact of obesity on intraoperative complications and prolapse recurrence after minimally invasive sacrocolpopexy. Female Pelvic Med Reconstr Surg. 2016;22(5):317–23. https://doi.org/10.1097/SPV.0000000000000278.
Vree FE, Cohen SL, Chavan N, Einarsson JI. The impact of surgeon volume on perioperative outcomes in hysterectomy. JSLS. 2014;18(2):174–81. https://doi.org/10.4293/108680813X13753907291594.
Author information
Authors and Affiliations
Contributions
L.E. Giugale: project development, data collection/management/analysis, manuscript writing; M.M. Hansbarger: project development, data collection, manuscript editing; A.L. Askew: project development, data collection, manuscript editing; A.G. Visco: project development, manuscript editing; J.P. Shepherd: project development, data collection, manuscript editing; M.S. Bradley: project development, data management, data analysis, manuscript writing.
Corresponding author
Ethics declarations
Conflicts of interest
Author Dr. Anthony Visco discloses stock ownership in NinoMed™. The remaining authors report no conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Giugale, L.E., Hansbarger, M.M., Askew, A.L. et al. Assessing pelvic organ prolapse recurrence after minimally invasive sacrocolpopexy: does mesh weight matter?. Int Urogynecol J 32, 2195–2201 (2021). https://doi.org/10.1007/s00192-021-04681-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-021-04681-6