Abstract
Introduction and hypothesis
The objective was to determine whether the rate of adnexal surgery varies by route of hysterectomy in women over the age of 65 undergoing hysterectomy for prolapse. We hypothesized that women undergoing vaginal hysterectomy would be less likely to undergo bilateral salpingo-oophorectomy (BSO) at the time of their hysterectomy for prolapse.
Methods
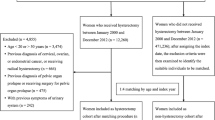
This was a cross-sectional analysis using the National Inpatient Sample (NIS) database. Our primary outcome was concomitant adnexal surgery performed at the time of hysterectomy, classified into five groups: BSO, unilateral salpingo-oophorectomy (USO), bilateral salpingectomy (BS), other adnexal surgery, and no adnexal surgery. The study sample included women aged 65 years and older who underwent hysterectomy between 1 January 2009 and 31 December 2014 and with a diagnosis of genital prolapse.
Results
Of the 91,292 patients over the age of 65 who underwent a hysterectomy for prolapse, the majority of hysterectomies were vaginal (69%), followed by abdominal (13%), laparoscopic (11%), and robotic (7%). The number of women having a hysterectomy and undergoing a BSO was much lower for vaginal than for other hysterectomy types; 20.3% of women undergoing vaginal hysterectomies had a BSO, compared with 79.2% in abdominal, 81.8% in laparoscopic, and 73.8% in robotic-assisted procedures. Women who received vaginal hysterectomies were five times as likely (RR: 5.02, 95% CI: 4.70–5.35) to have no concomitant adnexal procedure compared with other routes of hysterectomy.
Conclusions
Women over the age of 65 undergoing hysterectomy for prolapse are significantly less likely to have adnexal surgery if undergoing hysterectomy via vaginal route compared with the other routes.



Similar content being viewed by others
References
Gambone JC, Reiter RC, Lench JB. Quality assurance indicators and short-term outcome of hysterectomy. Obstet Gynecol. 1990;76(5 Pt 1):841–5.
Committee on Gynecologic Practice. Committee opinion no 701: choosing the route of hysterectomy for benign disease. Obstet Gynecol. 2017;129(6):e155–9. https://doi.org/10.1097/AOG.0000000000002112.
ACOG. ACOG practice bulletin no. 89. Elective and risk-reducing salpingo-oophorectomy. Obstet Gynecol. 2008;111(1):231–41. https://doi.org/10.1097/01.AOG.0000291580.39618.cb.
Ballard LA, Walters MD. Transvaginal mobilization and removal of ovaries and fallopian tubes after vaginal hysterectomy. Obstet Gynecol. 1996;87(1):35–9. https://doi.org/10.1016/0029-7844(95)00346-0.
Davies A, O’Connor H, Magos AL. A prospective study to evaluate oophorectomy at the time of vaginal hysterectomy. Br J Obstet Gynaecol. 1996;103(9):915–20. https://doi.org/10.1111/j.1471-0528.1996.tb09912.x.
Sheth SS. The place of oophorectomy at vaginal hysterectomy. Br J Obstet Gynaecol. 1991;98(7):662–6. https://doi.org/10.1111/j.1471-0528.1991.tb13452.x.
Dain L, Abramov Y. Factors affecting the feasibility of bilateral salpingo-oophorectomy during vaginal hysterectomy for uterine prolapse. Aust N Z J Obstet Gynaecol. 2011;51(4):307–9. https://doi.org/10.1111/j.1479-828X.2011.01323.x.
Karp NE, Fenner DE, Burgunder-Zdravkovski L, Morgan DM. Removal of normal ovaries in women under age 51 at the time of hysterectomy. Am J Obstet Gynecol. 2015;213(5):716.e1–6. https://doi.org/10.1016/j.ajog.2015.05.062.
Mikhail E, Salemi JL, Mogos MF, Hart S, Salihu HM, Imudia AN. National trends of adnexal surgeries at the time of hysterectomy for benign indication, United States, 1998–2011. Am J Obstet Gynecol. 2015;213(5):713 e711–3. https://doi.org/10.1016/j.ajog.2015.04.031.
Houchens R, Ross D, Elixhauser A. Using the HCUP national inpatient sample to estimate trends. HCUP methods series report # 2006-05 online. U.S. agency for healthcare research and quality. 2015. http://www.hcup-us.ahrq.gov/reports/methods/methods.jsp. Accessed 4 January 2016.
Houchens R, Ross D, Elixhauser A, Jiang J. Nationwide Inpatient Sample (NIS) redesign final report. 2014. HCUP NIS related reports online. 4 April 2014. U.S. Agency for healthcare research and quality. 2014. http://www.hcup-us.ahrq.gov/db/nation/nis/nisrelatedreports.jsp. Accessed 8 September 2018.
Zou G. A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702–6. https://doi.org/10.1093/aje/kwh090.
Robert M, Cenaiko D, Sepandj J, Iwanicki S. Success and complications of salpingectomy at the time of vaginal hysterectomy. J Minim Invasive Gynecol. 2015;22(5):864–9. https://doi.org/10.1016/j.jmig.2015.04.012.
Karp DR, Mukati M, Smith AL, Suciu G, Aguilar VC, Davila GW. Predictors of successful salpingo-oophorectomy at the time of vaginal hysterectomy. J Minim Invasive Gynecol. 2012;19(1):58–62. https://doi.org/10.1016/j.jmig.2011.09.008.
Antosh DD, High R, Brown HW, Oliphant SS, Abed H, Philip N, et al. Feasibility of prophylactic salpingectomy during vaginal hysterectomy. Am J Obstet Gynecol. 2017;217(5):605.e1–5. https://doi.org/10.1016/j.ajog.2017.07.017.
Author information
Authors and Affiliations
Contributions
K.A. Greene: protocol development, data collection, data analysis, manuscript preparation; A.M. Wyman: protocol development, manuscript preparation; N. Tamhane: protocol development, data collection, manuscript preparation; J.P. Tanner: protocol development, data collection, data analysis, manuscript preparation; R.M. Bassaly: manuscript preparation; J.L. Salemi: protocol development, data collection, data analysis, manuscript preparation.
Corresponding author
Ethics declarations
Conflicts of interest
The authors have no conflicts of interest to declare regarding the publication of this paper. The content is solely the responsibility of the authors and does not necessarily represent the official views of the University of South Florida or Baylor College of Medicine. The publicly available database used in this study is de-identified; therefore, this study was deemed exempt by the Institutional Review Board of Baylor College of Medicine.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Greene, K.A., Wyman, A.M., Tamhane, N. et al. Adnexal surgery at the time of hysterectomy in women 65 years and older undergoing hysterectomy for prolapse: do practice trends differ by route of surgery?. Int Urogynecol J 32, 2185–2193 (2021). https://doi.org/10.1007/s00192-020-04663-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-020-04663-0