Abstract
Introduction and hypothesis
The objective was to compare the clinical efficacy and safety of pharmacological interventions for interstitial cystitis and bladder pain syndrome (IC/BPS) with direct and indirect evidence from randomized trials.
Methods
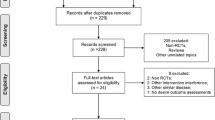
We searched PubMed, the Cochrane library, and EMBASE for randomized controlled trials (RCTs) that assessed the pharmacological therapies for IC/BPS. Primary efficacy outcomes included ICSI (O’Leary Sant Interstitial Cystitis Symptom Index), ICPI (O’Leary Sant Interstitial Cystitis Problem Index), 24-h micturition frequency, visual analog scale (VAS), and Likert score for pain. Safety outcomes are total adverse events (AEs, intravesical instillation, and others), gastrointestinal symptoms, headache, pain, and urinary symptoms. A systematic review and Bayesian network meta-analysis were performed.
Results
A total of 23 RCTs with 1,871 participants were identified. The ICSI was significantly reduced in the amitriptyline group (MD = −4.9, 95% CI: −9.0 to −0.76), the cyclosporine A group (MD = -7.9, 95% CI: −13.0 to −3.0) and the certolizumab pegol group (MD = −3.6, 95% CI:−6.5 to −0.63) compared with placebo group. Moreover, for ICPI, cyclosporine A showed superior benefit compared to placebo (MD = −7.6, 95% CI: −13 to −2.3). VAS score improved significantly in cyclosporine A group than pentosan polysulfate sodium (MD = 3.09, 95% CI: 0.13 to 6.07). None of the agents revealed a significant alleviation of 24-h micturition frequency. In terms of safety outcomes, the incidence rate on urinary symptoms for botulinum toxin A was the only variate higher than chondroitin sulfate (MD = −2.02, 95% CI: −4.99 to 0.66) and placebo (MD = −1.60, 95% CI:−3.83 to 0.17). No significant difference was found among the other treatments.
Conclusions
Cyclosporine A might be superior to other pharmacological treatments in efficacy. Amitriptyline and certolizumab pegol were capable of lowering the ICSI as well.









Similar content being viewed by others
References
Hanno P, Dmochowski R. Status of international consensus on interstitial cystitis/bladder pain syndrome/painful bladder syndrome: 2008 snapshot. Neurourol Urodyn. 2009;28(4):274–86. https://doi.org/10.1002/nau.20687.
Patnaik SS, Laganà AS, Vitale SG, Butticè S, Noventa M, Gizzo S, et al. Etiology, pathophysiology and biomarkers of interstitial cystitis/painful bladder syndrome. Arch Gynecol Obstet. 2017;295(6):1341–59. https://doi.org/10.1007/s00404-017-4364-2.
Hanno PM, Erickson D, Moldwin R, Faraday MM. Diagnosis and treatment of interstitial cystitis/bladder pain syndrome: AUA guideline amendment. J Urol. 2015;193(5):1545–53. https://doi.org/10.1016/j.juro.2015.01.086.
Malde S, Palmisani S, Al-Kaisy A, Sahai A. Guideline of guidelines: bladder pain syndrome. BJU Int. 2018;122(5):729–43. https://doi.org/10.1111/bju.14399.
Gülpınar Ö, Esen B, Kayış A, Gökçe Mİ, Süer E. Clinical comparison of intravesical hyaluronic acid and chondroitin sulfate therapies in the treatment of bladder pain syndrome/interstitial cystitis. Neurourol Urodyn. 2018;37(1):257–62. https://doi.org/10.1002/nau.23284.
Parsons CL, Zupkas P, Proctor J, Koziol J, Franklin A, Giesing D, et al. Alkalinized lidocaine and heparin provide immediate relief of pain and urgency in patients with interstitial cystitis. J Sex Med. 2012;9(1):207–12. https://doi.org/10.1111/j.1743-6109.2011.02542.x.
Henry RA, Morales A, Cahill CM. Beyond a simple anesthetic effect: lidocaine in the diagnosis and treatment of interstitial cystitis/bladder pain syndrome. Urology. 2015;85(5):1025–33. https://doi.org/10.1016/j.urology.2015.01.021.
Mayer R, Propert KJ, Peters KM, Payne CK, Zhang Y, Burks D, et al. A randomized controlled trial of intravesical bacillus Calmette–Guerin for treatment refractory interstitial cystitis. J Urol. 2005;173(4):1186–91. https://doi.org/10.1097/01.ju.0000152337.82806.e8.
Chuang Y-C, Kuo H-C. A prospective, multicenter, double-blind, randomized trial of bladder instillation of liposome formulation onabotulinumtoxinA for interstitial cystitis/bladder pain syndrome. J Urol. 2017;198(2):376–82. https://doi.org/10.1016/j.juro.2017.02.021.
Pinto RA, Costa D, Morgado A, Pereira P, Charrua A, Silva J, et al. Intratrigonal OnabotulinumtoxinA improves bladder symptoms and quality of life in patients with bladder pain syndrome/interstitial cystitis: a pilot, single center, randomized, double-blind, placebo controlled trial. J Urol. 2018;199(4):998-1003. https://doi.org/10.1016/j.juro.2017.10.018.
Kuo Y-C, Kuo H-C. O'Leary–Sant symptom index predicts the treatment outcome for OnabotulinumtoxinA injections for refractory interstitial cystitis/bladder pain syndrome. Toxins (Basel). 2015;7(8):2860–71. https://doi.org/10.3390/toxins7082860.
Foster HE Jr, Hanno PM, Nickel JC, Payne CK, Mayer RD, Burks DA, et al. Effect of amitriptyline on symptoms in treatment naïve patients with interstitial cystitis/painful bladder syndrome. J Urol. 2010;183(5):1853–8. https://doi.org/10.1016/j.juro.2009.12.106.
Al-Zahrani AA, Gajewski JB. Long-term efficacy and tolerability of pentosan polysulphate sodium in the treatment of bladder pain syndrome. Can Urol Assoc J. 2011;5(2):113–8. https://doi.org/10.5489/cuaj.10095.
Ogawa T, Ishizuka O, Ueda T, Tyagi P, Chancellor MB, Yoshimura N. Pharmacological management of interstitial cystitis/bladder pain syndrome and the role cyclosporine and other immunomodulating drugs play. Expert Rev Clin Pharmacol. 2018;11(5):495–505. https://doi.org/10.1080/17512433.2018.1457435.
Wyndaele JJJ, Riedl C, Taneja R, Lovász S, Ueda T, Cervigni M. GAG replenishment therapy for bladder pain syndrome/interstitial cystitis. Neurourol Urodyn. 2019;38(2):535–44. https://doi.org/10.1002/nau.23900.
Wammack R, Remzi M, Seitz C, Djavan B, Marberger M. Efficacy of oral doxepin and piroxicam treatment for interstitial cystitis. Eur Urol. 2002;41(6):596–600; discussion 601. https://doi.org/10.1016/s0302-2838(02)00174-4.
Lam KH, Yao G, Jin R. Diverse binding modes, same goal: the receptor recognition mechanism of botulinum neurotoxin. Prog Biophys Mol Biol. 2015;117(2–3):225–31. https://doi.org/10.1016/j.pbiomolbio.2015.02.004.
Zhang W, Deng X, Liu C, Wang X. Intravesical treatment for interstitial cystitis/painful bladder syndrome: a network meta-analysis. Int Urogynecol J. 2017;28(4):515–25. https://doi.org/10.1007/s00192-016-3079-4.
Matsuoka PK, Haddad JM, Pacetta AM, Baracat EC. Intravesical treatment of painful bladder syndrome: a systematic review and meta-analysis. Int Urogynecol J. 2012;23(9):1147–53. https://doi.org/10.1007/s00192-012-1686-2.
Guo C, Yang B, Gu W, Peng B, Xia S, Yang F, et al. Intravesical resiniferatoxin for the treatment of storage lower urinary tract symptoms in patients with either interstitial cystitis or detrusor overactivity: a meta-analysis. PLoS One. 2013;8(12):e82591. https://doi.org/10.1371/journal.pone.0082591.
Davis NF, Brady CM, Creagh T. Interstitial cystitis/painful bladder syndrome: epidemiology, pathophysiology and evidence-based treatment options. Eur J Obstet Gynecol Reprod Biol. 2014;175:30–7. https://doi.org/10.1016/j.ejogrb.2013.12.041.
Hanno PM, Landis JR, Matthews-Cook Y, Kusek J, Nyberg L Jr. The diagnosis of interstitial cystitis revisited: lessons learned from the National Institutes of Health interstitial cystitis database study. J Urol. 1999;161(2):553–7. https://doi.org/10.1016/s0022-5347(01)61948-7.
O'Leary MP, Sant GR, Fowler FJ Jr, Whitmore KE, Spolarich-Kroll J. The interstitial cystitis symptom index and problem index. Urology. 1997;49(5A Suppl):58–63. https://doi.org/10.1016/s0090-4295(99)80333-1.
Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. https://doi.org/10.1136/bmj.d5928.
Neupane B, Richer D, Bonner AJ, Kibret T, Beyene J. Network meta-analysis using R: a review of currently available automated packages. PLoS One. 2014;9(12):e115065. https://doi.org/10.1371/journal.pone.0115065.
van Ophoven A, Pokupic S, Heinecke A, Hertle L. A prospective, randomized, placebo controlled, double-blind study of amitriptyline for the treatment of interstitial cystitis. J Urol. 2004;172(2):533–6. https://doi.org/10.1097/01.ju.0000132388.54703.4d.
Chen H, Wang F, Chen W, Ye X, Zhou Q, Shao F, et al. Efficacy of daily low-dose sildenafil for treating interstitial cystitis: results of a randomized, double-blind, placebo-controlled trial—treatment of interstitial cystitis/painful bladder syndrome with low-dose sildenafil. Urology. 2014;84(1):51–6. https://doi.org/10.1016/j.urology.2014.02.050.
Bosch PC. A randomized, double-blind, placebo-controlled trial of Certolizumab Pegol in women with refractory interstitial cystitis/bladder pain syndrome. Eur Urol. 2018;74(5):623–30. https://doi.org/10.1016/j.eururo.2018.07.026.
Bosch PC. A randomized, double-blind, placebo controlled trial of adalimumab for interstitial cystitis/bladder pain syndrome. J Urol. 2014;191(1):77–82. https://doi.org/10.1016/j.juro.2013.06.038.
Wang H, Russell LJ, Kelly KM, Wang S, Thipphawong J. Fulranumab in patients with interstitial cystitis/bladder pain syndrome: observations from a randomized, double-blind, placebo-controlled study. BMC Urol. 2017;17(1):2. https://doi.org/10.1186/s12894-016-0193-z.
Evans RJ, Moldwin RM, Cossons N, Darekar A, Mills IW, Scholfield D. Proof of concept trial of tanezumab for the treatment of symptoms associated with interstitial cystitis. J Urol. 2011;185(5):1716–21. https://doi.org/10.1016/j.juro.2010.12.088.
Nickel JC, Egerdie B, Davis E, Evans R, Mackenzie L, Shrewsbury SB. A phase II study of the efficacy and safety of the novel Oral SHIP1 activator AQX-1125 in subjects with moderate to severe interstitial cystitis/bladder pain syndrome. J Urol. 2016;196(3):747–54. https://doi.org/10.1016/j.juro.2016.03.003.
Giannantoni A, Bini V, Dmochowski R, Hanno P, Nickel JC, Proietti S, et al. Contemporary management of the painful bladder: a systematic review. Eur Urol. 2012;61(1):29–53. https://doi.org/10.1016/j.eururo.2011.07.069.
Cervigni M, Sommariva M, Tenaglia R, Porru D, Ostardo E, Giammo A, et al. A randomized, open-label, multicenter study of the efficacy and safety of intravesical hyaluronic acid and chondroitin sulfate versus dimethyl sulfoxide in women with bladder pain syndrome/interstitial cystitis. Neurourol Urodyn. 2017;36(4):1178–86. https://doi.org/10.1002/nau.23091.
Davis EL, El Khoudary SR, Talbott EO, Davis J, Regan LJ. Safety and efficacy of the use of intravesical and oral pentosan polysulfate sodium for interstitial cystitis: A randomized double-blind clinical trial. J Urol. 2008;179(1):177–85.
Sairanen J, Tammela TL, Leppilahti M, Multanen M, Paananen I, Lehtoranta K, et al. Cyclosporine A and pentosan polysulfate sodium for the treatment of interstitial cystitis: a randomized comparative study. J Urol. 2005;174(6):2235–8. https://doi.org/10.1097/01.ju.0000181808.45786.84.
Nickel JC, Herschorn S, Whitmore KE, Forrest JB, Hu P, Friedman AJ, et al. Pentosan polysulfate sodium for treatment of interstitial cystitis/bladder pain syndrome: insights from a randomized, double-blind, placebo controlled study. J Urol. 2015;193(3):857–62. https://doi.org/10.1016/j.juro.2014.09.036.
Gülpınar Ö, Esen B, Kayış A, Gökçe Mİ, Süer E. Clinical comparison of intravesical hyaluronic acid and chondroitin sulfate therapies in the treatment of bladder pain syndrome/interstitial cystitis. Neurourol Urodyn. 2017;37(1):257–62.
El-Bahnasy AE, Farahat YA, El-Bendary M, et al. A randomized controlled trail of bacillus calmette-guerin and botulinum toxin-A for the treatment of refractory interstitial cystitis[J]. Urotoday Int J. 2008;02(1).
Nickel JC, Moldwin R, Lee S, Davis EL, Henry RA, Wyllie MJ. Intravesical alkalinized lidocaine (PSD597) offers sustained relief from symptoms of interstitial cystitis and painful bladder syndrome. BJU Int. 2009;103(7):910–8.
Manning J, Dwyer P, Rosamilia A, Colyvas K, Murray C, Fitzgerald E. A multicentre, prospective, randomised, double-blind study to measure the treatment effectiveness of abobotulinum A (AboBTXA) among women with refractory interstitial cystitis/bladder pain syndrome. Int Urogynecol J. 2014;25(5):593–9.
Nickel JC, Egerdie RB, Steinhoff G, Palmer B, Hanno P. A multicenter, randomized, double-blind, parallel group pilot evaluation of the efficacy and safety of intravesical sodium chondroitin sulfate versus vehicle control in patients with interstitial cystitis/painful bladder syndrome. Urology. 2010;76(4):804–9.
Irani D, Heidari M, Khezri AA. The efficacy and safety of intravesical Bacillus-Calmette-Guerin in the treatment of female patients with interstitial cystitis: a double-blinded prospective placebo controlled study. Urol J. 2004 Spring;1(2):90–3.
Propert KJ, Mayer R, Nickel JC, Payne CK, Peters KM, Teal V, et al. Followup of patients with interstitial cystitis responsive to treatment with intravesical bacillus calmette-guerin or placebo. J Urol. 2008;179(2):552–5.
Özkıdık M. Assessment of long-term intravesical hyaluronic acid, chondroitin sulfate and combination therapy for patients with bladder pain syndrome. Cent European J Urol. 2019;72:270–5. https://doi.org/10.5173/ceju.2019.0007.
Lin YH, Chiang BJ, Liao CH (2020) Mechanism of action of botulinum toxin a in treatment of functional urological disorders. Toxins (Basel) 12 (2):129. https://doi.org/10.3390/toxins12020129.
Kocatürk H, Atasoy N, Bedir F, Altay MS, Demirdöğen ŞO, Koç E, et al. Questionnaire-guided evaluation of the effectiveness of long-term intravesical 0.2% chondroitin sulfate therapy in interstitial cystitis. Int Urogynecol J. 2020. https://doi.org/10.1007/s00192-020-04245-0.
Scarneciu I, Bungau S, Lupu AM, Scarneciu CC, Bratu OG, Martha O, et al. Efficacy of instillation treatment with hyaluronic acid in relieving symptoms in patients with BPS/IC and uncomplicated recurrent urinary tract infections—long-term results of a multicenter study. Eur J Pharm Sci. 2019;139:105067. https://doi.org/10.1016/j.ejps.2019.105067.
Tirumuru S, Al-Kurdi D, Latthe P. Intravesical botulinum toxin a injections in the treatment of painful bladder syndrome/interstitial cystitis: a systematic review. Int Urogynecol J. 2010;21(10):1285–300. https://doi.org/10.1007/s00192-010-1162-9.
Crescenze IM, Tucky B, Li J, Moore C, Shoskes DA. Efficacy, side effects, and monitoring of Oral cyclosporine in interstitial cystitis-bladder pain syndrome. Urology. 2017;107:49–54. https://doi.org/10.1016/j.urology.2017.05.016.
Wang Z, Zhang L. Treatment effect of cyclosporine a in patients with painful bladder syndrome/interstitial cystitis: a systematic review. Exp Ther Med. 2016;12(1):445–50. https://doi.org/10.3892/etm.2016.3301.
Forrest JB, Payne CK, Erickson DR. Cyclosporine a for refractory interstitial cystitis/bladder pain syndrome: experience of 3 tertiary centers. J Urol. 2012;188(4):1186–91. https://doi.org/10.1016/j.juro.2012.06.023.
Giusto LL, Zahner PM, Shoskes DA. An evaluation of the pharmacotherapy for interstitial cystitis. Expert Opin Pharmacother. 2018;19(10):1097–108. https://doi.org/10.1080/14656566.2018.1491968.
Dijkmans B, Gerards A. Cyclosporin in rheumatoid arthritis: monitoring for adverse effects and clinically significant drug interactions. BioDrugs. 1998;10(6):437–45. https://doi.org/10.2165/00063030-199810060-00002.
Maza A, Montaudié H, Sbidian E, Gallini A, Aractingi S, Aubin F, et al. Oral cyclosporin in psoriasis: a systematic review on treatment modalities, risk of kidney toxicity and evidence for use in non-plaque psoriasis. J Eur Acad Dermatol Venereol. 2011;25(Suppl 2):19–27. https://doi.org/10.1111/j.1468-3083.2011.03992.x.
Sairanen J, Forsell T, Ruutu M. Long-term outcome of patients with interstitial cystitis treated with low dose cyclosporine A. J Urol. 2004;171(6 Pt 1):2138–41. https://doi.org/10.1097/01.ju.0000125139.91203.7a.
Ehrén I, Hallén Grufman K, Vrba M, Sundelin R, Lafolie P. Nitric oxide as a marker for evaluation of treatment effect of cyclosporine a in patients with bladder pain syndrome/interstitial cystitis type 3C. Scand J Urol. 2013;47(6):503–8. https://doi.org/10.3109/21681805.2013.788552.
Wang J, Wang Q, Wu Q, Chen Y, Wu P. Intravesical botulinum toxin a injections for bladder pain syndrome/interstitial cystitis: a systematic review and meta-analysis of controlled studies. Med Sci Monit. 2016;22:3257–67. https://doi.org/10.12659/msm.897350.
Barua JM, Arance I, Angulo JC, Riedl CR. A systematic review and meta-analysis on the efficacy of intravesical therapy for bladder pain syndrome/interstitial cystitis. Int Urogynecol J. 2016;27(8):1137–47. https://doi.org/10.1007/s00192-015-2890-7.
Dawson TE, Jamison J (2007) Intravesical treatments for painful bladder syndrome/interstitial cystitis. Cochrane Database Syst Rev (4):CD006113. https://doi.org/10.1002/14651858.CD006113.pub2.
Acknowledgements
This study was funded by 1.3.5 project for disciplines of excellence, West China Hospital, Sichuan University (Grant Nos. ZY2016104) and 1.3.5 project for disciplines of excellence, West China Hospital, Sichuan University (Grant Nos. ZYGD18011), and 1.3.5 project for disciplines of excellence, West China Hospital, Sichuan University (Grant Nos. ZYGC18015). Project of Science and Technology Department of Sichuan Province (2018SZ0177, 2018SZ0055).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Table 1
(DOC 20 kb)
Supplementary Table 2
(DOC 21 kb)
Figure S1
(PNG 17 kb)
Figure S2
(PNG 1699 kb)
Figure S3
(PNG 2336 kb)
Figure S4
(PNG 1179 kb)
Figure S5
(PNG 1185 kb)
Figure S6
(PNG 1668 kb)
Rights and permissions
About this article
Cite this article
Di, Xp., Luo, Dy., Jin, X. et al. Efficacy and safety comparison of pharmacotherapies for interstitial cystitis and bladder pain syndrome: a systematic review and Bayesian network meta-analysis. Int Urogynecol J 32, 1129–1141 (2021). https://doi.org/10.1007/s00192-020-04659-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-020-04659-w