Abstract
Introduction and hypothesis
Nocturia, defined as the act of waking to pass urine during sleeping, is a common problem in older women and is associated with significant morbidity and impairments in health-related quality of life. The aim of this review was to synthesize the current evidence regarding the incidence, impact, pathophysiology, and specific diagnostic approach of nocturia in the postmenopausal population.
Methods
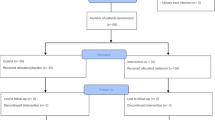
We searched PubMed and Web of Science databases to identify relevant studies published through June 2020. Reference lists of the reviews obtained were screened for other articles deemed pertinent by the authors.
Results
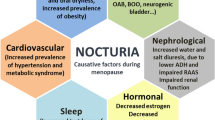
Genitourinary symptoms attributed to the menopause have been reported to occur in nearly 90% of postmenopausal women, and nocturia is one of the most common. The relative deficiency in endogenous estrogen production after the menopause is thought to exacerbate all major pathophysiological mechanisms that may underlie nocturia, including reduced bladder capacity, nocturnal polyuria, global polyuria, and sleep disorders. Diminished estrogen may induce anatomical and physiological bladder changes, contributing to a reduction in functional bladder capacity. Excess nocturnal urine production can also be provoked by estrogen depletion, either via free water-predominant diuresis by an impaired secretion of antidiuretic hormone, or a salt-predominant diuresis owing to diminished activation of the renin–angiotensin–aldosterone axis. Additionally, a relationship between the transition to menopause and impaired sleep has been described, mediated by increased incidence in vasomotor symptoms and obstructive sleep apnea signs during the menopause.
Conclusion
Further research is necessary to better characterize and manage nocturia in postmenopausal women.


Similar content being viewed by others
Abbreviations
- ADH:
-
Antidiuretic hormone
- BMI:
-
Body mass index
- DM:
-
Diabetes mellitus
- FVC:
-
Frequency volume chart
- FWC:
-
Free water clearance
- MHT:
-
Menopausal hormone therapy
- NP:
-
Nocturnal polyuria
- OAB:
-
Overactive bladder syndrome
- OSAS:
-
Obstructive sleep apnea syndrome
- RAAS:
-
Renin–angiotensin–aldosterone system
- VMS:
-
Vasomotor symptom
- VTE:
-
Venous thromboembolism
References
Hashim H, Blanker M, Djurhuus JC, Meijlink J, Morris V, Petros P, et al. The International Continence Society standardisation of terminology in nocturia. Neurourol Urodyn. 2017;21(2):179–83.
Kupelian V, Fitzgerald MP, Kaplan SA, Norgaard JP, Chiu GR, Rosen RC. Association of nocturia and mortality: results from the third National Health and Nutrition Examination Survey. J Urol. 2011;185(2):571–7.
Nakagawa H, Niu K, Hozawa A, Ikeda Y, Kaiho Y, Ohmori-Matsuda K, et al. Impact of nocturia on bone fracture and mortality in older individuals: a Japanese longitudinal cohort study. J Urol. 2010;184(4):1413–8.
Pesonen JS, Cartwright R, Vernooij RWM, Aoki Y, Agarwal A, Mangera A, et al. The impact of nocturia on mortality: a systematic review and meta-analysis. J Urol. 2020;203(3):486–95.
Pesonen JS, Vernooij RWM, Cartwright R, Aoki Y, Agarwal A, Mangera A, et al. The impact of nocturia on falls and fractures: a systematic review and meta-analysis. J Urol. 2020;203(4):674–83.
Bliwise DL, Holm-Larsen T, Goble S, Nørgaard JP. Short time to first void is associated with lower whole-night sleep quality in nocturia patients. J Clin Sleep Med. 2015;11(1):53–5. https://doi.org/10.5664/jcsm.4364.
Gulur DM, Mevcha AM, Drake MJ. Nocturia as a manifestation of systemic disease. BJU Int. 2011;107(5):702–13. https://doi.org/10.1111/j.1464-410X.2010.09763.x.
Yoshimura K. Correlates for nocturia: a review of epidemiological studies. Int J Urol. 2012;19(4):317–29. https://doi.org/10.1111/j.1442-2042.2011.02956.x.
Weiss JP. Nocturia: focus on etiology and consequences. Rev Urol. 2012;14(3–4):48–55.
Davies HO, Popplewell M, Singhal R, Smith N, Bradbury AW. Obesity and lower limb venous disease—the epidemic of phlebesity. Phlebology. 2017;32(4):227–33. https://doi.org/10.1177/0268355516649333.
Srisukho S, Pantasri T, Piyamongkol W, Phongnarisorn C, Morakote N. The experience of genitourinary syndrome of menopause (GSM) among Thai postmenopausal women: the non-reporting issue. Int Urogynecol J. 2019;30(11):1843–7.
Goldstein I, Dicks B, Kim NN, Hartzell R. Multidisciplinary overview of vaginal atrophy and associated genitourinary symptoms in postmenopausal women. Sex Med. 2013;1(2):44–53. https://doi.org/10.1002/sm2.17.
Terauchi M, Hirose A, Akiyoshi M, Owa Y, Kato K, Kubota T. Prevalence and predictors of storage lower urinary tract symptoms in perimenopausal and postmenopausal women attending a menopause clinic. Menopause. 2015;22(10):1084–90. https://doi.org/10.1097/GME.0000000000000432.
Varella LRD, Bezerra da Silva R, Eugênia de Oliveira MC, Melo PHA, de Maranhão TMO, Barbosa Cabral Micussi MTA. Assessment of lower urinary tract symptoms in different stages of menopause. J Phys Ther Sci. 2016;28(11):3116–21.
Asplund R, Åberg HE. Nocturia and health in women aged 40–64 years. Maturitas. 2000;35(2):143–8.
Pauwaert K, Goessaert A-S, Ghijselings L, Bower W, Depypere H, Everaert K. Characterizing nocturia among Belgian healthy postmenopausal women: prevalence, bother, etiology and possible risk factors for developing nocturia. Maturitas. 2020;143:41–6. https://doi.org/10.1016/j.maturitas.2020.08.008.
Oelke M, De Wachter S, Drake MJ, Giannantoni A, Kirby M, Orme S, et al. A practical approach to the management of nocturia. Int J Clin Pract. 2017;71(11):e13027.
Everaert K, Hervé F, Bower W, Djurhuus JC, Dmochowski R, Fine N, et al. How can we develop a more clinically useful and robust algorithm for diagnosing and treating nocturia? ICI-RS 2017. Neurourol Urodyn. 2018;37(S4):S46–59.
Batra SC, Iosif CS. Progesterone receptors in the female lower urinary tract. J Urol. 1987;138(5):1301–4.
Portman DJ, Gass MLS, Kingsberg S, Archer D, Bachmann G, Burrows L, et al. Genitourinary syndrome of menopause: new terminology for vulvovaginal atrophy from the International Society for the Study of Women’s Sexual Health and the North American Menopause Society. Menopause. 2014;21(10):1063–8.
Robinson D, Toozs-Hobson P, Cardozo L. The effect of hormones on the lower urinary tract. Menopause Int. 2013;19(4):155–62.
Overactive Bladder (OAB) Guideline—American Urological Association.
Parsons M, Amundsen CL, Cardozo L, Vella M, Webster GD, Coats AC. Bladder diary patterns in detrusor overactivity and urodynamic stress incontinence. Neurourol Urodyn. 2007;26(6):800–6. https://doi.org/10.1002/nau.20406.
Hristov KL, Parajuli SP, Provence A, Rovner ES, Petkov GV. Nongenomic modulation of the large conductance voltage- and Ca2+−activated K+ channels by estrogen: a novel regulatory mechanism in human detrusor smooth muscle. Phys Rep. 2017;5(14):e13351. https://doi.org/10.14814/phy2.13351.
Goessaert A-S, Krott L, Hoebeke P, Vande Walle J, Everaert K. Diagnosing the pathophysiologic mechanisms of nocturnal polyuria. Eur Urol. 2015;67(2):283–8.
Monaghan TF, Bliwise DL, Denys M-A, Goessaert A-S, Decalf V, Kumps C, et al. Phenotyping nocturnal polyuria: circadian and age-related variations in diuresis rate, free water clearance and sodium clearance. Age Ageing. 2020;49:439–45. https://doi.org/10.1093/ageing/afz200.
Kujubu DA, Aboseif SR. Evaluation of nocturia in the elderly. Perm J. 2007;11(1):37–9.
Stachenfeld NS. Hormonal changes during menopause and the impact on fluid regulation. Reprod Sci. 2014;21:555–61.
Verbalis JG. Renal physiology of nocturia. Neurourol Urodyn. 2014;33:S6–9. https://doi.org/10.1002/nau.22594.
Tani M, Hirayama A, Fujimoto K, Torimoto K, Akiyama T, Hirao Y. Increase in 24-hour urine production/weight causes nocturnal polyuria due to impaired function of antidiuretic hormone in elderly men. Int J Urol. 2008;15:151–4. https://doi.org/10.1111/j.1442-2042.2007.01949.x.
Stachenfeld NS, DiPietro L, Palter SF, Nadel ER. Estrogen influences osmotic secretion of AVP and body water balance in postmenopausal women. Am J Phys. 1998;274(1):R187–95.
Ishunina TA, Kruijver FPM, Balesar R, Swaab DF. Differential expression of estrogen receptor α and β immunoreactivity in the human Supraoptic nucleus in relation to sex and aging. J Clin Endocrinol Metab. 2000;85(9):3283–91. https://doi.org/10.1210/jcem.85.9.6826.
Paech K, Webb P, Kuiper GGJM, Nilsson S, Gustafsson JÅ, Kushner PJ, et al. Differential ligand activation of estrogen receptors ERα and ERrβ at AP1 sites. Science. 1997;277(5331):1508–10. https://doi.org/10.1126/science.277.5331.1508.
Stachenfeld NS, Splenser AE, Calzone WL, Taylor MP, Keefe DL. Selected contribution: sex differences in osmotic regulation of AVP and renal sodium handling. J Appl Physiol. 2001;91(4):1893–901.
Bossmar T, Forsling M, Åkerlund M. Circulating oxytocin and vasopressin is influenced by ovarian steroid replacement in women. Acta Obstet Gynecol Scand. 1995;74(7):544–8.
Oelkers WKH. Effects of estrogens and progestogens on the renin–aldosterone system and blood pressure. Steroids. 1996;61:166–71.
Chidambaram M, Duncan JA, Lai VS, Cattran DC, Floras JS, Scholey JW, et al. Variation in the renin angiotensin system throughout the normal menstrual cycle. J Am Soc Nephrol. 2002;13:446–52.
Harvey PJ, Morris BL, Miller JA, Floras JS. Estradiol induces discordant angiotensin and blood pressure responses to orthostasis in healthy postmenopausal women. Hypertension. 2005;45(3):399–405. https://doi.org/10.1161/01.HYP.0000157161.78721.5c.
Oelkers WHK. Drospirenone in combination with estrogens: for contraception and hormone replacement therapy. Climacteric. 2005;8:19–27. https://doi.org/10.1080/13697130500330341.
Leimola-Virtanen R, Salo T, Toikkanen S, Pulkkinen J, Syrjänen S. Expression of estrogen receptor (ER) in oral mucosa and salivary glands. Maturitas. 2000;36(2):131–7.
Leimola-Virtanen R, Helenius H, Laine M. Hormone replacement therapy and some salivary antimicrobial factors in post- and perimenopausal women. Maturitas. 1997;27(2):145–51.
Minicucci E, Pires R, Vieira R, Miot H, Sposto M. Assessing the impact of menopause on salivary flow and xerostomia. Aust Dent J. 2013;58(2):230–4. https://doi.org/10.1111/adj.12057.
McKinley MJ, Johnson AK. The physiological regulation of thirst and fluid intake. Physiology. 2004;19(1):1–6. https://doi.org/10.1152/nips.01470.2003.
Tani M, Hirayama A, Torimoto K, Matsushita C, Yamada A, Fujimoto K. Guidance on water intake effectively improves urinary frequency in patients with nocturia. Int J Urol. 2014;21(6):595–600. https://doi.org/10.1111/iju.12387.
Asplund R, Åberg HE. Oral dryness, nocturia and the menopause. Maturitas. 2005;50(2):86–90.
Tom SE, Kuh D, Guralnik JM, Mishra GD. Self-reported sleep difficulty during the menopausal transition: results from a prospective cohort study. Menopause. 2010;17(6):1128–35.
Xu Q, Lang CP. Examining the relationship between subjective sleep disturbance and menopause: a systematic review and meta-analysis. Menopause. 2014;21:1301–18.
Kravitz HM, Zhao X, Bromberger JT, Gold EB, Hall MH, Matthews KA, et al. Sleep disturbance during the menopausal transition in a multi-ethnic community sample of women. Sleep. 2008;31(7):979.
Ohayon MM. Severe hot flashes are associated with chronic insomnia. Arch Intern Med. 2006;166(12):1262–8.
Dennerstein L, Lehert P, Guthrie JR, Burger HG. Modeling women’s health during the menopausal transition: a longitudinal analysis. Menopause. 2007;14(1):53–62.
Kravitz HM, Ganz PA, Bromberger J, Powell LH, Sutton-Tyrrell K, Meyer PM. Sleep difficulty in women at midlife: a community survey of sleep and the menopausal transition. Menopause. 2003;10:19–28.
Freedman RR, Roehrs TA. Effects of REM sleep and ambient temperature on hot flash-induced sleep disturbance. Menopause. 2006;13(4):576–83.
Kapsimalis F, Kryger M. Sleep breathing disorders in the U.S. female population. J Womens Health. 2009;18(8):1211–9.
Bixler EO, Vgontzas AN, Lin HM, Ten Have T, Rein J, Vela-Bueno A, et al. Prevalence of sleep-disordered breathing in women: effects of gender. Am J Respir Crit Care Med. 2001;163(3 I):608–13. https://doi.org/10.1164/ajrccm.163.3.9911064.
Phillips BA. Differences between men and women in the clinical presentation of patients diagnosed with obstructive sleep apnea syndrome. Yearb Pulm Dis. 2006.
Dancey DR, Hanly PJ, Soong C, Lee B, Hoffstein V. Impact of menopause on the prevalence and severity of sleep apnea. Chest. 2001;120(1):151–5.
Young T, Finn L, Austin D, Peterson A. Menopausal status and sleep-disordered breathing in the Wisconsin sleep cohort study. Am J Respir Crit Care Med. 2003;167(9):1181–5. https://doi.org/10.1164/rccm.200209-1055OC.
Polesel DN, Hirotsu C, Nozoe KT, Boin AC, Bittencourt L, Tufik S, et al. Waist circumference and postmenopause stages as the main associated factors for sleep apnea in women: a cross-sectional population-based study. Menopause. 2015;22(8):835–44. https://doi.org/10.1097/GME.0000000000000406.
Guilleminault C, Palombini L, Poyares D, Chowdhuri S. Chronic insomnia, postmenopausal women, and sleep disordered breathing. I. Frequency of sleep disordered breathing in a cohort. J Psychosom Res. 2002;53(1):611–5.
Umlauf MG, Chasens ER, Greevy RA, Arnold J, Burgio KL, Pillion DJ. Obstructive sleep apnea, nocturia and polyuria in older adults. Sleep. 2004;27(1):139–44.
Miyazaki T, Kojima S, Yamamuro M, Sakamoto K, Izumiya Y, Tsujita K, et al. Nocturia in patients with sleep-disordered breathing and cardiovascular disease. Circ J. 2015;79(12):2632–40.
Gjørup PH, Sadauskiene L, Wessels J, Nyvad O, Strunge B, Pedersen EB. Increased nocturnal sodium excretion in obstructive sleep apnoea. Relation to nocturnal change in diastolic blood pressure. Scand J Clin Lab Invest. 2008;68(1):11–21. https://doi.org/10.1080/00365510701352020.
Bonanni E, Schirru A, Di Perri MC, Bonuccelli U, Maestri M. Insomnia and hot flashes. Maturitas. 2019;126:51–4.
Kravitz HM, Joffe H. Sleep during the perimenopause: a SWAN story. Obstet Gynecol Clin N Am. 2011;38(3):567–86.
Mintziori G, Lambrinoudaki I, Goulis DG, Ceausu I, Depypere H, Erel CT, et al. EMAS position statement: non-hormonal management of menopausal vasomotor symptoms. Maturitas. 2015;81(3):410–3. https://doi.org/10.1016/j.maturitas.2015.04.009.
Shen L, Song L, Li H, Liu B, Zheng X, Zhang L, et al. Association between earlier age at natural menopause and risk of diabetes in middle-aged and older Chinese women: the Dongfeng–Tongji cohort study. Diabetes Metab. 2017;43(4):345–50.
Malacara JM, Huerta R, Rivera B, Esparza S, Fajardo ME. Menopause in normal and uncomplicated NIDDM women: physical and emotional symptoms and hormone profile. Maturitas. 1997;28(1):35–45. https://doi.org/10.1016/S0378-5122(97)00051-0.
Appiah D, Winters SJ, Hornung CA. Bilateral oophorectomy and the risk of incident diabetes in postmenopausal women. Diabetes Care. 2014;37(3):725–33. https://doi.org/10.2337/dc13-1986.
Yuan Z, Tang Z, He C, Tang W. Diabetic cystopathy: a review. J Diabetes. 2015;7:442–7. https://doi.org/10.1111/1753-0407.12272.
Everaert K, Hervé F, Bosch R, Dmochowski R, Drake M, Hashim H, et al. International Continence Society consensus on the diagnosis and treatment of nocturia. Neurourol Urodyn. 2019;38(2):478–98. https://doi.org/10.1002/nau.23939.
Gratzke C, Bachmann A, Descazeaud A, Drake MJ, Madersbacher S, Mamoulakis C, et al. EAU guidelines on the assessment of non-neurogenic male lower urinary tract symptoms including benign prostatic obstruction. Eur Urol. 2015;67(6):1099–109.
Bower WF, Rose GE, Ervin CF, Goldin J, Whishaw DM, Khan F. TANGO—a screening tool to identify comorbidities on the causal pathway of nocturia. BJU Int. 2017;119(6):933–41.
Decalf V, Everaert K, De Witte N, Petrovic M, Bower W. Dutch version of the TANGO nocturia screening tool: cross-culturally translation and reliability study in community-dwelling people and nursing home residents. Acta Clin Belg. 2019;75(6):397–404.
Hanna-Mitchell AT, Robinson D, Cardozo L, Everaert K, Petkov GV. Do we need to know more about the effects of hormones on lower urinary tract dysfunction? ICI-RS 2014. Neurourol Urodyn. 2016;35(2):299–303. https://doi.org/10.1002/nau.22809.
Kiba K, Hirayama A, Yishikawa M, Yutaka Y, Torimoto K, Nobutaka S, et al. Increased urine production due to leg fluid displacement reduces hours of undisturbed sleep. Low Urin Tract Symptoms. 2018;10(3):253–8. https://doi.org/10.1111/luts.12176.
Carpenter J, Gass MLS, Maki PM, Newton KM, Pinkerton JV, Taylor M, et al. Nonhormonal management of menopause-associated vasomotor symptoms. Menopause. 2015;22(11):1155–74. https://doi.org/10.1097/GME.0000000000000546.
Freedman RR. Hot flashes: behavioral treatments, mechanisms, and relation to sleep. Am J Med. 2005;118:124–30.
Burkhard FC, Bosch JLHR, Cruz F, Lemack GE, Nambiar AK, Thiruchelvam N, et al. EAU guidelines on urinary incontinence in adults. Eur Assoc Urol. 2018;73(4):596–609.
Miotla P, Cartwright R, Futyma K, Bogusiewicz M, Skorupska K, Winkler I, et al. Can botox improve night-time overactive bladder symptoms in women? Neurourol Urodyn. 2017;36(3):648–52. https://doi.org/10.1002/nau.22983.
Abrams P, Chapple C, Khoury S, Roehrborn C, de la Rosette J. Evaluation and treatment of lower urinary tract symptoms in older men. J Urol. 2013;189(1):S93–101.
Sharaf A, Thomas L, Hashim H. The effect of sacral neuromodulation on nocturia in patients presenting with detrusor overactivity. https://www.ics.org/2016/abstract/849
Denys MA, Kapila V, Weiss J, Goessaert AS, Everaert K. Basic or extended urine sampling to analyse urine production? Neurourol Urodyn. 2017;36(7):1867–75. https://doi.org/10.1002/nau.23198.
Reynard C, Yang A. A novel therapy for nocturnal polyuria: a double-blind randomized trial of frusemide against placebo. Br J Urol. 1998;81(2):215–8. https://doi.org/10.1046/j.1464-410X.1998.00511.x.
Sand PK, Dmochowski RR, Reddy J, Van Der Meulen EA. Efficacy and safety of low dose desmopressin orally disintegrating tablet in women with nocturia: results of a multicenter, randomized, double-blind, placebo controlled, parallel group study. J Urol. 2013;190(3):958–64. https://doi.org/10.1016/j.juro.2013.02.037.
Weiss JP, Zinner NR, Klein BM, Nørgaard JP. Desmopressin orally disintegrating tablet effectively reduces nocturia: results of a randomized, double-blind, placebo-controlled trial. Neurourol Urodyn. 2012;31(4):441–7. https://doi.org/10.1002/nau.22243.
Rembratt A, Riis A, Norgaard JP. Desmopressin treatment in nocturia; an analysis of risk factors for hyponatremia. Neurourol Urodyn. 2006;25(2):105–9. https://doi.org/10.1002/nau.20168.
Weiss JP, Everaert K. Management of nocturia and nocturnal polyuria. Urology. 2019;133:24–33. https://doi.org/10.1016/j.urology.2019.09.022.
Juul KV, Jessen N, Bliwise DL, van der Meulen E, Nørgaard JP. Delaying time to first nocturnal void may have beneficial effects on reducing blood glucose levels. Endocrine. 2016;53(3):722–9.
The 2017 hormone therapy position statement of the North American Menopause Society. Menopause. 2018;25(11):1362–87. doi: https://doi.org/10.1097/GME.0000000000001241.
Rahn DD, Carberry C, Sanses TV, Mamik MM, Ward RM, Meriwether KV, et al. Vaginal estrogen for genitourinary syndrome of menopause. Obstet Gynecol. 2014;124:1147–56.
Kok ALM, Burger CW, Van De Weijer PHM, Voetberg GA, Peters-Muller ERA, Kenemans P. Micturition complaints in postmenopausal women treated with continuously combined hormone replacement therapy: a prospective study. Maturitas. 1999;31(2):143–9.
Cody JD, Jacobs ML, Richardson K, Moehrer B, Hextall A. Oestrogen therapy for urinary incontinence in post-menopausal women. Cochrane Database Syst Rev. 2012;10(10):CD001405. https://doi.org/10.1002/14651858.cd001405.pub3.
MacLennan AH, Broadbent JL, Lester S, Moore V. Oral oestrogen and combined oestrogen/progestogen therapy versus placebo for hot flushes. Cochrane Database Syst Rev. 2004;2004(4):CD002978. https://doi.org/10.1002/14651858.cd002978.pub2.
Shahar E, Redline S, Young T, Boland LL, Baldwin CM, Nieto FJ, et al. Hormone replacement therapy and sleep-disordered breathing. Am J Respir Crit Care Med. 2003;167(9):1186–92. https://doi.org/10.1164/rccm.200210-1238OC.
Cistulli PA, Barnes DJ, Grunstein RR, Sullivan CE, Cistulli PA, Barnes DJ, et al. Effect of short term hormone replacement in the treatment of obstructive sleep apnoea in postmenopausal women. Thorax. 1994;49:699–702.
Baber RJ, Panay N, Fenton A. 2016 IMS recommendations on women’s midlife health and menopause hormone therapy. Climacteric. 2016;19(2):109–50. https://doi.org/10.3109/13697137.2015.1129166.
Roach REJ, Lijfering WM, Van Hylckama VA, Helmerhorst FM, Rosendaal FR, Cannegieter SC. The risk of venous thrombosis in individuals with a history of superficial vein thrombosis and acquired venous thrombotic risk factors. Blood. 2013;122(26):4264–9. https://doi.org/10.1182/blood-2013-07-518159.
Scarabin P-Y. Hormone therapy and venous thromboembolism among postmenopausal women. Front Horm Res. 2014;43:21–32. https://doi.org/10.1159/000360554.
Canonico M, Plu-Bureau G, Lowe GDO, Scarabin PY. Hormone replacement therapy and risk of venous thromboembolism in postmenopausal women: systematic review and meta-analysis. BMJ. 2008;336(7655):1227–31. https://doi.org/10.1136/bmj.39555.441944.BE.
Rovinski D, Ramos RB, Fighera TM, Casanova GK, Spritzer PM. Risk of venous thromboembolism events in postmenopausal women using oral versus non-oral hormone therapy: a systematic review and meta-analysis. Thromb Res. 2018;168:83–95.
Manson JAE, Chlebowski RT, Stefanick ML, Aragaki AK, Rossouw JE, Prentice RL, et al. Menopausal hormone therapy and health outcomes during the intervention and extended poststopping phases of the women’s health initiative randomized trials. JAMA. 2013;310(13):1353–68. https://doi.org/10.1001/jama.2013.278040.
Shams T, Firwana B, Habib F, Alshahrani A, Alnouh B, Murad MH, et al. SSRIs for hot flashes: a systematic review and meta-analysis of randomized trials. J Gen Intern Med. 2014;29:204–13. https://doi.org/10.1007/s11606-013-2535-9.
Margel D, Shochat T, Getzler O, Livne PM, Pillar G. Continuous positive airway pressure reduces nocturia in patients with obstructive sleep apnea. Urology. 2006;67(5):974–7.
Miyazato M, Tohyama K, Touyama M, Nakamura H, Oshiro T, Ueda S, et al. Effect of continuous positive airway pressure on nocturnal urine production in patients with obstructive sleep apnea syndrome. Neurourol Urodyn. 2017;36(2):376–9. https://doi.org/10.1002/nau.22936.
Miyauchi Y, Okazoe H, Okujyo M, Inada F, Kakehi T, Kikuchi H, et al. Effect of the continuous positive airway pressure on the nocturnal urine volume or night-time frequency in patients with obstructive sleep apnea syndrome. Urology. 2015;85(2):333–6.
Acknowledgements
The authors thank the Ghent University Frederik Paulson Chair for unrestricted support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
K.P. receives a research grant from Ferring; K.E. reports grants and other financial contributions from Ferring, grants from Astellas, grants and other financial contributions from Medtronic outside the submitted work, shareholder and co-founder of P2S. The remaining authors claim no conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pauwaert, K., Goessaert, AS., Ghijselings, L. et al. Nocturia through the menopausal transition and beyond: a narrative review. Int Urogynecol J 32, 1097–1106 (2021). https://doi.org/10.1007/s00192-020-04640-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-020-04640-7