Abstract
Introduction and hypothesis
Pelvic organ prolapse (POP) is a common pathological condition that may require surgical management. Several surgical treatment options are possible, and practice varies from one center to another. The objective of the present study was to describe the surgical management and outcomes of POP in France from 2008 to 2014.
Methods
We performed a retrospective cohort study of all patients operated on for POP from 2008 to 2014, according to the French national hospital discharge summary database. Patient characteristics, surgical approaches, concomitant hysterectomy and/or incontinence surgery, the length of stay, the proportion of day-case operations, and patient outcomes were analyzed.
Results
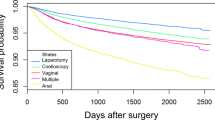
We analyzed 310,938 hospital stays with POP surgery between 2008 and 2014; 130,908 (42%) of the operations took place in hospitals performing more than 100 prolapse surgical procedures per year. The proportion of day-case operations was low, but rose significantly from 1.2% to 4.6% during the study period. More than half of the operations featured a vaginal approach. The proportions of operations with concomitant hysterectomy or urinary incontinence surgery fell from 41.0% to 36.1% and from 33.0% to 25.8% respectively. The proportions of laparoscopic procedures increased. The mortality rate was stable (0.07% for all years).
Conclusions
The number of patients undergoing POP surgery remained stable from 2008 to 2014. The proportion of laparoscopic procedures increased (in parallel with the rising proportion of day-case operations) and the proportion of procedures with concomitant hysterectomy or incontinence treatment decreased.


Similar content being viewed by others
References
Lousquy R, Costa P, Delmas V, Haab F. Update on the epidemiology of genital prolapse. Prog Urol. 2009;19:907–15.
Barber MD, Maher C. Epidemiology and outcome assessment of pelvic organ prolapse. Int Urogynecol J. 2013;24:1783–90.
Olsen AL, Smith VJ, Bergstrom JO, Colling JC, Clark AL. Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol. 1997;89:501–6.
Le Normand L, Cosson M, Cour F, Deffieux X, Donon L, et al. Clinical practice guidelines: synthesis of the guidelines for the surgical treatment of primary pelvic organ prolapse in women by the AFU, CNGOF, SIFUD-PP, SNFCP, and SCGP. J Gynecol Obstet Hum Reprod. 2017;46(5):387-91
Brown JS, Waetjen LE, Subak LL, Thom DH, Van den Eeden S, et al. Pelvic organ prolapse surgery in the United States, 1997. Am J Obstet Gynecol. 2002;186:712–6.
Detollenaere RJ, Den Boon J, Kluivers KB, Vierhout ME, Van Eijndhoven HWF. Surgical management of pelvic organ prolapse and uterine descent in the Netherlands. Int Urogynecol J. 2013;24:781–8.
Luber KM, Boero S, Choe JY. The demographics of pelvic floor disorders: current observations and future projections. Am J Obstet Gynecol. 2001;184:1496–501 1503.
Debodinance P, Berrocal J, Clavé H, Cosson M, Garbin O, et al. Changing attitudes on the surgical treatment of urogenital prolapse: birth of the tension-free vaginal mesh. J Gynecol Obstet Biol Reprod (Paris). 2004;33:577–88.
HAS 2019, National Commission for Medical Devices and Health Technologies, which reinforcing implants to treat prolapse of the female pelvic organs? https://www.has-sante.fr/upload/docs/application/pdf/2020-02/300120_reco329__note_cadrage_rbp_prolapsus_mel.pdf.
Lucot JP, Cosson M, Bader G, Debodinance P, Akladios C, et al. Safety of vaginal mesh surgery versus laparoscopic mesh sacropexy for cystocele repair: results of the prosthetic pelvic floor repair randomized controlled trial. Eur Urol 2018;74(2):167–176.
Maher C, Feiner B, Baessler K, Schmid C. Surgical management of pelvic organ prolapse in women. Cochrane Database Syst Rev 2013;(4)CD004014.
Deffieux X, Fernandez H. Vaginal prolapse surgery. EMC 2014.
Mandron E, Bryckaert PE. Genital prolapse and colpocele. Coelioscopic sacrocolpopexy. Ann Urol. 2005;39:247–56.
Rozet F, Mandron E, Arroyo C, Andrews H, Cathelineau X, et al. Laparoscopic sacral colpopexy approach for genito-urinary prolapse: experience with 363 cases. Eur Urol. 2005;47:230–6.
Boudemaghe T, Belhadj I. Data resource profile: the French national uniform hospital discharge data set database (PMSI). Int J Epidemiol. 2016;46(2):392-392d
WHO. International Classification of Diseases, 11th Revision (ICD-11). In: WHO. http://www.who.int/classifications/icd/en/. Accessed 1 Oct 2018.
Codage des actes médicaux—CCAM. https://www.ameli.fr/medecin/exercice-liberal/facturation-remuneration/nomenclatures-codage/codage-actes-medicaux-ccam. Accessed 1 Oct 2018.
Core Team R. R: a language and environment for statistical computing. Vienna: R Foundation for Statistical Computing; 2016.
Cotte B, De Lapasse C, Nohuz E, Rivoire C, Tamburro S, et al. Coeliochirurgie. EMC 2008.
Wagner L, Meurette G, Vidart A, Warembourg S, Terassa JB, et al. Laparoscopic sacrocolpopexy for pelvic organ prolapse: guidelines for clinical practice. Prog Urol. 2016;26(Suppl 1):S27–37.
Hamid D. Preliminary results for ambulatory surgery for vaginal prolapse. J Gynecol Obstet Biol Reprod (Paris). 2016;45:580–4.
Hefni M, El Toukhy T, Bhaumik J, Katsimanis E. Sacrospinous cervicocolpopexy with uterine conservation for uterovaginal prolapse in elderly women: an evolving concept. Am J Obstet Gynecol. 2003;188:645–50.
Detollenaere RJ, Den Boon J, Stekelenburg J, Inthout J, Vierhout ME, al. Sacrospinous hysteropexy versus vaginal hysterectomy with suspension of the uterosacral ligaments in women with uterine prolapse stage 2 or higher: multicentre randomised non-inferiority trial. BMJ. 2015;351:h3717.
Cayrac M, Warembourg S, Le Normand L, Fatton B. Does hysterectomy modifies the anatomical and functional outcomes of prolapse surgery?: clinical practice guidelines. Prog Urol. 2016;26(Suppl 1):S73–88.
Lin TY, Su TH, Wang YL, Lee MY, Hsieh CH, et al. Risk factors for failure of transvaginal sacrospinous uterine suspension in the treatment of uterovaginal prolapse. J Formos Med Assoc. 2005;104:249–53.
Cortesse A, Cardot V, Basset V, Le Normand L, Donon L. Treatment of urinary incontinence associated with genital prolapse: clinical practice guidelines. Prog Urol. 2016;26(Suppl 1):S89–97.
Alas AN, Chinthakanan O, Espaillat L, Plowright L, Davila GW, al. De novo stress urinary incontinence after pelvic organ prolapse surgery in women without occult incontinence. Int Urogynecol J. 2017;28:583–90.
Ennemoser S, Schönfeld M, Von Bodungen V, Dian D, Friese K, et al. Clinical relevance of occult stress urinary incontinence (OSUI) following vaginal prolapse surgery: long-term follow-up. Int Urogynecol J. 2012;23:851–5.
Giraudet G, Lucot JP, Quinton JF, Cosson M. Genital prolapse. EMC 2016.
Dwyer PL. Women with occult stress incontinence should not routinely have a mid-urethral sling with prolapse surgery. Int Urogynecol J. 2012;23:827–9.
Funding
This work is part of the Probiomesh project funded by the European Regional Development Fund and the Cohesion Fund.
Author information
Authors and Affiliations
Contributions
M. Hendriks: manuscript writing/editing, critical manuscript revision, final approval of the manuscript; S. Bartolo: protocol, critical manuscript revision, final approval of the manuscript; G. Giraudet: critical manuscript revision, final approval of the manuscript; M. Cosson: protocol, critical manuscript revision, final approval of the manuscript; E. Chazard: protocol, data collection or management, data analysis, critical manuscript revision, final approval of the manuscript.
Corresponding author
Ethics declarations
Ethics committee approval
This article is an epidemiological study for which ethical approval does not apply.
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hendriks, M., Bartolo, S., Giraudet, G. et al. Change over time in the surgical management of pelvic organ prolapse between 2008 and 2014 in France: patient profiles, surgical approaches, and outcomes. Int Urogynecol J 32, 961–966 (2021). https://doi.org/10.1007/s00192-020-04491-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-020-04491-2