Abstract
Introduction and hypothesis
To describe study design flaws and limited outcomes of a randomized trial that intended to compare satisfaction and complication rates between patients managing their pelvic organ prolapse with a pessary at different maintenance intervals.
Methods
A randomized clinical trial was conducted at two tertiary pessary clinics. After a successful fitting, patients were randomly allocated to follow-up at 3-month or 6-month intervals and followed for 12 months. Symptoms, complications, and pelvic examination characteristics were recorded at each visit. At 6 and 12 months, patient satisfaction with the pessary was also recorded. Sample size calculation was based on the minimal relevant difference in Pessary Satisfaction score (created for this study). With a power of 0.8 and an alpha of 0.05, the minimum number of patients required in each group was 28.
Results
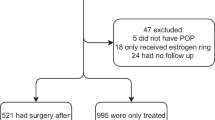
We were unable to reach our sample size as most patients did not meet inclusion criteria. After 2 years we were only able to recruit 20/56 patients, with 9 patients in the 3-month group and 11 patients in the 6-month group. Additionally, seven patients dropped out of the study. Overall satisfaction was high and similar between groups at 6- and 12-month follow-up visits. Pessary complications were noted in both groups but in low numbers.
Conclusions
Pessary use is associated with high patient satisfaction and low complication rates, regardless of the follow-up interval. The recruitment failure demonstrated that a randomized trial is not feasible for this research question. Optimally, pessary follow-up should be based on patient symptoms and scheduling preference.



Similar content being viewed by others
References
Samuelsson EC, Victor FT, Tibblin G, Svärdsudd KF. Signs of genital prolapse in a Swedish population of women 20 to 59 years of age and possible related factors. Am J Obstet Gynecol. 1999;180:299–305.
MacLennan AH, Taylor AW, Wilson DH, Wilson D. The prevalence of pelvic floor disorders and their relationship to gender, age, parity and mode of delivery. BJOG. 2000;107:1460–70.
Fernando RJ, Thakar R, Sultan AH, Shah SM, Jones PW. Effect of vaginal pessaries on symptoms associated with pelvic organ prolapse. Obstet Gynecol. 2006;108:93–9.
Boyles SH, Weber AM, Meyn L. Procedures for pelvic organ prolapse and urinary incontinence in the United States, 1979- 1997. Am J Obstet Gynecol. 2003;188:108–15.
Abed H, Rahn DD, Lowenstein L, Balk EM, Clemons JL, Rogers RG. Incidence and management of graft erosion, wound granulation, and dyspareunia following vaginal prolapse repair with graft materials: a systematic review. Int Urogynecol J. 2011;22:789–98.
Cundiff GW, Weidner AC, Visco AG, Bump RC, Addison WA. A survey of pessary use by members of the American Urogynecologic Society. Obstet Gynecol. 2000;95:931–5.
Sarma S, Ying T, Moore KH. Long-term vaginal ring pessary use: discontinuation rates and adverse events. BJOG. 2009;116:1715–21.
Powers K, Grigorescu B, Lazarou G, Greston WM, Weber T. Neglected pessary causing a rectovaginal fistula: a case report. J Reprod Med. 2008;53:235–7.
Kearney R, Brown C (2014) Self-management of vaginal pessaries for pelvic organ prolapse. BMJ Qual Improv Rep 3(1).
Radnia N, Hajhashemi M, Eflekhar T, et al. Patient satisfaction and symptoms improvement in women using a vaginal pessary for the treatment of pelvic organ prolapse. J Med Life. 2019;12:271–5.
Mao M, Ai F, Kang J, et al. Successful long-term use of Gellhorn pessary and the effect on symptoms and quality of life in women with symptomatic pelvic organ prolapse. Menopause. 2019;26:145–51.
Ko PC, Lo TS, Tseng LH, Lin YH, Liang CC, Lee SJ. Use of a pessary in treatment of pelvic organ prolapse: quality of life, compliance and failure at 1-year follow-up. J Minim Invasive Gynecol. 2011;18:68–74.
Lamers BHC, Broekman BMW, Milani AL. Pessary treatment for pelvic organ prolapse and health-realated quality of life: a review. Int Urogynecol J. 2011;22:637–44.
Gorti M, Hudelist G, Simons A. Evaluation of vaginal pessary management: a UK-based survey. J Obstet Gynaecol. 2009;29(2):129–31.
Wu V, Farrell SA, Baskett TF, Flowerdew G. A simplified protocol for pessary management. Obstet Gynecol. 1997;90:990–4.
Adams E, Thomson A, Maher C, Hagen S. Mechanical devices for pelvic organ prolapse in women. Cochrane Database Syst Rev. 2004;2:CD004010.
Tam MS, Lee VYT, Yu ELM, et al. The effect of time interval of vaginal ring pessary replacement for pelvic organ prolapse on complications and patient satisfaction: a randomised controlled trial. Maturitas. 2019;128:29–35.
Manonai J, Sarit-Apirak S, Udomsubpayakul U. Vaginal ring pessary use for pelvic organ prolapse: continuation rates and predictors of continued use. Menopause. 2018;26:665–9.
Hsieh MF, Tsai HW, Liou WS, et al. Long-term compliance of vaginal pessaries: does stress urinary incontinence matter? Medicine (Baltimore). 2019;98:e15063.
Mao M, Xu T, Kang J, et al. Factors associated with long-term pessary use in women with symptomatic pelvic organ prolapse. Climacteric. 2019;22:478–82.
Clemons JL, Aguilar VC, Tillinghast TA, Jackson ND, Myers DL. Risk factors associated with an unsuccessful pessary fitting trial in women with pelvic organ prolapse. Am J Obstet Gynecol. 2004;190:345–50.
Roberge RJ, Keller C, Garfinkel M. Vaginal pessary-induced mechanical bowel obstruction. J Emerg Med. 2001;20:367–70.
Dengler EG, Mounsey LA, Gines F, Agha M, Long T, Geller EJ. Defecatory dysfunction and other clinical variables are predictors of pessary discontinuation. Int Urogynecol J. 2019;30:1111–6.
Abdulaziz M, Stothers L, Lazare D, Macnab A. An integrative review and severity classification of complications related to pessary use in the treatment of female pelvic organ prolapse. Can Urol Assoc J. 2015;9:E400–6.
Radnia N, Hajhashemi M, Eftekhar T, et al. Patient satisfaction and symptoms improvement in women using vaginal pessary for the treatment of pelvic organ prolapse. J Med Life. 2019;12:271–5.
Acknowledgments
The authors would like to thank the study coordinator, Vishu Chakravarti, for her organization and assistance during the study period.
Author information
Authors and Affiliations
Contributions
B Anglim: data analysis, manuscript writing and editing, visualization.
ZY Zhao: data collection, data analysis and curation, visualization.
D Lovatsis: protocol/project development, resources, manuscript writing and editing.
CD McDermott: protocol/project development, data collection, data management, resources, manuscript writing and editing, visualization, supervision, project administration.
Corresponding author
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Clinical trial registration
NCT01644214 (https://clinicaltrials.gov).
Rights and permissions
About this article
Cite this article
Anglim, B., Zhao, Z.Y., Lovatsis, D. et al. The extended pessary interval for care (EPIC) study: a failed randomized clinical trial. Int Urogynecol J 32, 937–944 (2021). https://doi.org/10.1007/s00192-020-04489-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-020-04489-w