Abstract
Introduction and hypothesis
Tears of the levator ani muscle are common after vaginal birth and associated with pelvic organ prolapse (POP). Although such trauma is usually attributed to the first vaginal birth, epidemiological evidence suggests an additional effect of subsequent vaginal deliveries. Our hypothesis was: “The prevalence of avulsion increases with the number of vaginal births”.
Methods
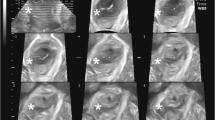
We conducted a retrospective cohort study in patients who presented to a tertiary urogynaecology clinic. Assessment included a physician-directed interview, POP-Q and 4D translabial ultrasound (TLUS), supine, after voiding, at rest, on maximum pelvic floor muscle contraction (PFMC) and Valsalva. Offline analysis of levator integrity was undertaken by tomographic imaging (TUI) at a later date, blinded against all other data.
Results
A total of 1,124 patients had been seen between 1 January 2014 and 30 June 2016, on average 33 (0.32–69.7) years after their first birth. Mean age was 56 (19–90) years. 1,012 (90%) were vaginally parous with a median vaginal parity of 2 (1–8). On TUI, avulsion was diagnosed in 257 (23%) women, all of whom were vaginally parous. On univariate analysis, there was no significant difference in the prevalence of avulsion on comparing vaginally primiparous and multiparous women (P = 0.6), nor was there any difference between vaginal parity groups (one, two, three, and ≥4 births; p = 0.7). This remained true after controlling for potential confounding factors using multivariate regression (p = 0.6).
Conclusions
There was no significant difference in the prevalence of avulsion between vaginally primiparous and multiparous women. Vaginal deliveries after a first vaginal birth are unlikely to cause avulsion.

Similar content being viewed by others
References
Volloyhaug I, Morkved S, Salvesen K. Association between pelvic floor muscle trauma and pelvic organ prolapse 20 years after delivery. Int Urogynecol J. 2016;27(1):39–45.
Shek K, Green K, Caudwell Hall J, Guzman Rojas R, Dietz H. Perineal and vaginal tears are clinical markers for occult levator ani trauma: a retrospective observational study. Ultrasound Obstet Gynecol. 2016;47:224–7.
Dietz H, Gillespie A, Phadke P. Avulsion of the pubovisceral muscle associated with large vaginal tear after normal vaginal delivery at term. Aust N Z J Obstet Gynaecol. 2007;47:341–4.
Kearney R, Miller JM, Delancey JO. Interrater reliability and physical examination of the pubovisceral portion of the levator ani muscle, validity comparisons using MR imaging. Neurourol Urodyn. 2006;25(1):50–4.
Dietz HP, Shek KL. Levator defects can be diagnosed by 2D translabial ultrasound. Int Urogynecol J. 2009;20:807–11.
DeLancey JO, Kearney R, Chou Q, Speights S, Binno S. The appearance of levator ani muscle abnormalities in magnetic resonance images after vaginal delivery. Obstet Gynecol. 2003;101(1):46–53.
Dietz H, Lanzarone V. Levator trauma after vaginal delivery. Obstet Gynecol. 2005;106:707–12.
DeLancey J, Morgan D, Fenner D, Kearney R, Guire K, Miller J, et al. Comparison of levator ani muscle defects and function in women with and without pelvic organ prolapse. Obstet Gynecol. 2007;109(2):295–302.
Dietz H, Simpson J. Levator trauma is associated with pelvic organ prolapse. Br J Obstet Gynaecol. 2008;115:979–84.
Friedman T, Eslick G, Dietz H. Risk factors for prolapse recurrence: systematic review and meta-analysis. Int Urogynecol J. 2018;29(1):13–21.
DeLancey JO. The anatomy of the pelvic floor. Curr Opin Obstet Gynecol. 1994;6(4):313–6.
Friedman T, Eslick G, Dietz HP. Delivery mode and the risk of levator muscle avulsion: a meta-analysis. Int Urogynecol J. 2019;30:901–7.
Horak A, Guzman Rojas R, Shek K, Dietz H. Pelvic floor trauma: does the second baby matter? Int Urogynecol J. 2012;23(S2):S175–6.
Atan I, Lin S, Dietz H, Herbison P, Wilson P. It is the first birth that does the damage: a cross-sectional study 20 years after delivery. Int Urogynecol J. 2018;29:1637–43.
Leijonhufvud A, Lundholm C, Cnattingius S, et al. Risks of stress urinary incontinence and pelvic organ prolapse surgery in relation to mode of childbirth. Am J Obstet Gynecol. 2011;204:70.e1–6.
Glazener C, Elders A, MacArthur C, Lancashire R, Herbison P, Hagen S, et al. Childbirth and prolapse: long-term associations with the symptoms and objective measurement of pelvic organ prolapse. BJOG. 2013;120:161–8.
Bump RC, Mattiasson A, Bo K, Brubaker LP, DeLancey JO, Klarskov P, et al. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol. 1996;175(1):10–7.
Dietz H. Pelvic floor ultrasound—a review. Clin Obstet Gynecol. 2017;60:58–81.
Dietz H, Bernardo M, Kirby A, Shek K. Minimal criteria for the diagnosis of avulsion of the puborectalis muscle by tomographic ultrasound. Int Urogynecol J. 2011;22(6):699–704.
Dietz H, Abbu A, Shek K. The levator urethral gap measurement: a more objective means of determining levator avulsion? Ultrasound Obstet Gynecol. 2008;32:941–5.
Abdool Z, Shek KL, Dietz HP. The effect of levator avulsion on hiatal dimension and function. Am J Obstet Gynecol. 2009;201:89.e1–5.
Skinner L, Dietz HP. Psychological and somatic sequelae of traumatic vaginal delivery: a literature review. Aust N Z J Obstet Gynaecol. 2015;55:309–31.
Skinner E, Barnett B, Dietz H. Psychological consequences of pelvic floor trauma following vaginal birth: a qualitative study from two Australian tertiary maternity units. Arch Womens Ment Health. 2018;21(3):341–51.
Dolan LM, Hilton P. Obstetric risk factors and pelvic floor dysfunction 20 years after first delivery. Int Urogynecol J. 2010;21:535–44.
MacLennan AH, Taylor AW, Wilson DH, Wilson PD. The prevalence of pelvic floor disorders and their relationship to gender, age, parity and mode of delivery. Br J Obstet Gynaecol. 2000;107:1460–70.
Swift SE. The distribution of pelvic organ support in a population of female subjects seen for routine gynecologic health care. Am J Obstet Gynecol. 2000;183:277–85.
Abdool Z, Dietz HP, Lindeque G. Interethnic variation in pelvic floor morphology in women with symptomatic pelvic organ prolapse. Int Urogynecol J. 2018;29(5):745–50. https://doi.org/10.1007/s00192-017-3391-7.
Cheung R, Chan S, Shek KL, Chung T, Dietz HP. Pelvic organ prolapse in Caucasian and Asian women: a comparative study ultrasound. Obstet Gynaecol. 2019;53(4):541–5. https://doi.org/10.1002/uog.20124.
Handa V, Lockhart M, Fielding J, Bradley C, Brubaker L, Cundiff G, et al. Racial differences in pelvic anatomy by magnetic resonance imaging. Obstet Gynecol. 2008;111(4):914–20.
AIUM/IUGA practice parameter for the performance of urogynecological ultrasound examinations: developed in collaboration with the ACR, the AUGS, the AUA, and the SRU. Int Urogynecol J. 2019;30(9):1389–400.
Contributions
H.P. Dietz: project conception, design and development, data acquisition, analysis and interpretation, drafting the manuscript, revising it critically for important intellectual content and final approval of the version to be published; C. Walsh: data acquisition, analysis and interpretation, drafting the manuscript, revising it critically for important intellectual content and final approval of the version to be published; N. Subramaniam: data acquisition, analysis and interpretation, drafting the manuscript, revising it critically for important intellectual content and final approval of the version to be published; T. Friedman: data acquisition, analysis and interpretation, drafting the manuscript, revising it critically for important intellectual content and final approval of the version to be published.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
H.P. Dietz has received unrestricted educational grants from GE Medical and Mindray. The other authors have no conflicts of interest to declare.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dietz, H.P., Walsh, C., Subramaniam, N. et al. Levator avulsion and vaginal parity: do subsequent vaginal births matter?. Int Urogynecol J 31, 2311–2315 (2020). https://doi.org/10.1007/s00192-020-04330-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-020-04330-4