Abstract
Introduction and hypothesis
There has been a scarcity of long-term published data comparing lightweight versus heavier weight transvaginal mesh for prolapse repair. The aim was to ascertain the long-term rates of recurrent prolapse and mesh exposure in a cohort of vaginal repairs utilizing two different weights of transvaginal mesh.
Methods
Data were prospectively collected on all mesh-augmented vaginal prolapse repairs performed with Apogee® or Perigee® mesh kits (IntePro® or IntePro Lite®) at a single centre over an 11-year period, with patients receiving ongoing annual follow-up. A sequential stepwise univariate and multivariate Cox regression analysis was performed to identify variables that were significantly associated with mesh exposure.
Results
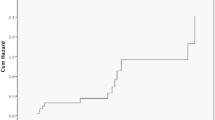
Eighty-eight women with 113 mesh kits were reviewed from the original cohort of 158 women. The median length of follow-up was 6.4 years (range 1.1–12.5 years). Mesh exposure rate per implant in the IntePro® group was 16/40 (40%) versus 4/73 (5.5%) in the IntePro Lite® group (p < 0.0001). A hazard ratio of 4.2 was identified for mesh exposure for IntePro® versus IntePro Lite® (95% CI 3.0–6.8). There was no difference in rates of recurrent prolapse between the heavy- and lightweight mesh groups.
Conclusions
Lightweight transvaginal mesh is associated with lower mesh exposure rates than heavyweight mesh at a median follow-up of 6.4 years, with no difference in rates of recurrent prolapse.
Similar content being viewed by others
References
Nygaard I, Bradley C, Brandt D. Pelvic organ prolapse in older women: prevalence and risk factors. Obstet Gynecol. 2004;104(3):489–97. https://doi.org/10.1097/01.AOG.0000136100.10818.d8.
Chow D, Rodriguez LV. Epidemiology and prevalence of pelvic organ prolapse. Curr Opin Urol. 2013;23(4):293–8. https://doi.org/10.1097/MOU.0b013e3283619ed0.
Smith FJ, Holman CD, Moorin RE, Tsokos N. Lifetime risk of undergoing surgery for pelvic organ prolapse. Obstet Gynecol. 2010;116(5):1096–100. https://doi.org/10.1097/AOG.0b013e3181f73729.
Olsen AL, Smith VJ, Bergstrom JO, Colling JC, Clark AL. Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol. 1997;89(4):501–6. https://doi.org/10.1016/s0029-7844(97)00058-6.
Jonsson Funk M, Edenfield AL, Pate V, Visco AG, Weidner AC, Wu JM. Trends in use of surgical mesh for pelvic organ prolapse. Am J Obstet Gynecol. 2013;208(1):79.e71–7. https://doi.org/10.1016/j.ajog.2012.11.008.
FDA News Release 16 April 2019 https://www.fda.gov/news-events/press-announcements/fda-takes-action-protect-womens-health-orders-manufacturers-surgical-mesh-intended-transvaginal.
Karmakar D, Hayward L, Smalldridge J, Lin S. Vaginal mesh for prolapse: a long-term prospective study of 218 mesh kits from a single centre. Int Urogynecol J. 2015;26(8):1161–70. https://doi.org/10.1007/s00192-015-2658-0.
Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J. 2010;21(1):5–26. https://doi.org/10.1007/s00192-009-0976-9.
Karmakar D HL, Lin S, Smalldridge J (2014) A calculator for risk prediction of mesh extrusion in vaginal mesh augmented repair: a novel translational approach to risk counselling and decision making in urogynaecology. Int Urogynecol J 25. https://doi.org/10.1007/s00192-014-2429-3.
Curtiss N, Duckett J. A long-term cohort study of surgery for recurrent prolapse comparing mesh augmented anterior repairs to anterior colporrhaphy. Gynecol Surg. 2018;15(1):1. https://doi.org/10.1186/s10397-017-1035-z.
Maher C, Feiner B, Baessler K, Christmann-Schmid C, Haya N, Marjoribanks J. Transvaginal mesh or grafts compared with native tissue repair for vaginal prolapse. Cochrane Database Syst Rev. 2016;2:Cd012079. https://doi.org/10.1002/14651858.Cd012079.
Rane A, Iyer J, Kannan K, Corstiaans A. Prospective study of the perigee system for treatment of cystocele—our five-year experience. Aust N Z J Obstet Gynaecol. 2012;52(1):28–33. https://doi.org/10.1111/j.1479-828X.2011.01384.x.
Glazener CMA, Breeman S, Elders A, Hemming C, Cooper KG, Freeman RM. Mesh, graft, or standard repair for women having primary transvaginal anterior or posterior compartment prolapse surgery: two parallel-group, multicentre, randomised, controlled trials (PROSPECT). Lancet. 2017;389(10067):381–92. https://doi.org/10.1016/s0140-6736(16)31596-3.
Donati M, Brancato G, Grosso G, Li Volti G, La Camera G, Cardi F. Immunological reaction and oxidative stress after light or heavy polypropylene mesh implantation in inguinal hernioplasty: a CONSORT-prospective, randomized, clinical trial. Medicine. 2016;95(24):e3791. https://doi.org/10.1097/md.0000000000003791.
Liang R, Abramowitch S, Knight K, Palcsey S, Nolfi A, Feola A. Vaginal degeneration following implantation of synthetic mesh with increased stiffness. BJOG. 2013;120(2):233–43. https://doi.org/10.1111/1471-0528.12085.
Feola A, Abramowitch S, Jallah Z, Stein S, Barone W, Palcsey S. Deterioration in biomechanical properties of the vagina following implantation of a high-stiffness prolapse mesh. BJOG. 2013;120(2):224–32. https://doi.org/10.1111/1471-0528.12077.
Liang R, Knight K, Abramowitch S, Moalli PA. Exploring the basic science of prolapse meshes. Curr Opin Obstet Gynecol. 2016;28(5):413–9. https://doi.org/10.1097/gco.0000000000000313.
Kelly EC, Winick-Ng J, Welk B. Surgeon experience and complications of transvaginal prolapse mesh. Obstet Gynecol. 2016;128(1):65–72. https://doi.org/10.1097/aog.0000000000001450.
Management of Mesh and Graft Complications in Gynecologic Surgery. Female pelvic medicine & reconstructive surgery 2017;23(3):171–176. https://doi.org/10.1097/spv.0000000000000425
Lo TS, Tan YL, Cortes EF, Wu PY, Pue LB, Al-Kharabsheh A. Clinical outcomes of mesh exposure/extrusion: presentation, timing and management. Aust N Z J Obstet Gynaecol. 2015;55(3):284–90. https://doi.org/10.1111/ajo.12340.
Tijdink MM, Vierhout ME, Heesakkers JP, Withagen MI. Surgical management of mesh-related complications after prior pelvic floor reconstructive surgery with mesh. Int Urogynecol J. 2011;22(11):1395–404. https://doi.org/10.1007/s00192-011-1476-2.
Cundiff GW, Quinlan DJ, van Rensburg JA, Slack M. Foundation for an evidence-informed algorithm for treating pelvic floor mesh complications: a review. Bjog. 2018;125(8):1026–37. https://doi.org/10.1111/1471-0528.15148.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Previously presented as a Fellows Day Presentation at the IUGA 43nd Annual Meeting, Vienna, Austria, June 2018.
Rights and permissions
About this article
Cite this article
Dykes, N., Karmakar, D. & Hayward, L. Lightweight transvaginal mesh is associated with lower mesh exposure rates than heavyweight mesh. Int Urogynecol J 31, 1785–1791 (2020). https://doi.org/10.1007/s00192-020-04270-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-020-04270-z