Abstract
Introduction and hypothesis
Uncomplicated urinary tract infection (uUTI) is defined as the presence of pathogenic organisms in the urinary tract without anatomical and functional abnormalities, is accompanied by inflammatory leukocytes and cytokines and may or may not develop clinical symptoms. The frequency of uncomplicated urinary tract infection is higher in young women. Several quinolone treatment regimens are available; however, since we do not know which is the best antibiotic regimen for the treatment of this urinary infection, we analyzed the published evidence and conducted a systematic review with network meta-analysis. The aim was to compare and hierarchize quinolones according to their efficacy and safety and to identify the best treatment for uncomplicated urinary tract infection in women through a systematic review with network meta-analysis.
Methods
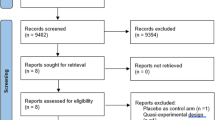
Medline, Embase, LILACS, Cochrane CENTRAL and other databases were searched for trials. Bias in the trials was assessed using the Cochrane Collaboration tool. To analyze efficacy and adverse events, for direct comparisons, we obtained risk ratios and 95% confidence intervals by applying a fixed-effects model using tau2 and Q2 tests to calculate the heterogeneity. For the network meta-analysis, we analyzed the indirect comparisons by Bucher’s method.
Results
We included 18 trials (8765 women). For premenopausal women, ofloxacin had a 57% probability of achieving remission but an 83% frequency of adverse events. For postmenopausal women, ofloxacin was 82% more effective for remission, with a 49% frequency of adverse events, compared with other types of quinolones.
Conclusions
Compared with other quinolones, ofloxacin 200 mg once daily for a treatment duration < 3 days provides the highest clinical and bacteriological remission rates with the lowest relapse and resistance rates for the treatment of women with uUTIs. However, additional trials are needed to confirm our findings, especially when the treatment duration exceeds 3 days.






Similar content being viewed by others
Abbreviations
- CI 95%:
-
95% confidence intervals
- DNA:
-
deoxyribonucleic acid
- IF:
-
inconsistency factor
- MeSH:
-
Medical Subject Headings
- NMA:
-
network meta-analysis
- RR:
-
risk ratio
- SUCRA:
-
surface under the cumulative ranking curve
- TMP/SMX:
-
trimethoprim-sulfamethoxazole
- UTI:
-
urinary tract infection
- uUTI:
-
uncomplicated urinary tract infection
References
Booth J, Mullen A, Thomson D, Johnstone C, Galbraith S, Bryson S, et al. Antibiotic treatment of urinary tract infection by community pharmacists: a cross-sectional study. Br J Gen Pract 2013; 63: e244–e249. http://dx.doi.org/https://doi.org/10.3399/bjgp13X665206.
Rafalsky V, Andreeva I, Rjabkova E. Quinolones for uncomplicated acute cystitis in women (review). Cochrane Database Syst Rev, 2006; 3: CD003597. http://dx.doi.org/https://doi.org/10.1002/14651858.CD003597.pub2.
Alós J. Epidemiology and etiology of urinary tract infections in the community. Antimicrobial susceptibility of the main pathogens and clinical significance of resistance. Enferm Infecc Microbiol Clin. 2005;23(4):3–8.
Gupta K, Trautner B. Principios de Medicina Interna. 19 ed. Mexico: Mc GrawHill; c2016. Chapter 162, Infecciones de vías urinarias, pielonefritis y prostatitis; p. 861–68.
Medina M, Castillo-Pino E. An introduction to the epidemiology and burden of urinary trac infections. Ther Adv Urol 2019;11:3–7. http://dx.doi.org/https://doi.org/10.1177/1756287219832172.
Zalmanovici Trestioreanu A, Green H, Paul M, Yaphe J, Leibovici L. Antimicrobial agents for treating uncomplicated urinary tract infection in women. Cochrane Database Syst Rev 2010, Issue 10. Art. No.: CD007182. http://dx.doi.org/https://doi.org/10.1002/14651858.CD007182.pub2.
Urinary Tract Infection In: Litwin MS, Saigal CS, editors. Urologic Diseases in America. US Department of Health and Human Services, Public Health Service, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases. Washington, DC: US Government Printing Office, 2012; NIH Publication No. 1265: 365–404.
Gupta K, Hooton T, Naber K, Wullt B, Colgan R, Miller L, et al. International clinical practice guidelines for the treatment of acute uncomplicated cystitis and pyelonephritis in women: a 2010 update by the Infectious Diseases Society of America and the European Society for Microbiology and Infectious Diseases. Clin Infect Dis 2011; 52(5): e103–e120. http://dx.doi.org/https://doi.org/10.1093/cid/ciq257.
Andersson MI, MacGowan AP. Development of the quinolones. J Antimicrob Chemother. 2003;51(S1):1–11. http://dx.doi.org/. https://doi.org/10.1093/jac/dkg212.
Heeb S, Fletcher M, Chhabra S, Diggle S, Williams P, Cámara M. Quinolones: from antibiotics to autoinducers. FEMS Microbiol Lett 2011; 35(2): 247–274. http://dx.doi.org/https://doi.org/10.1111/j.1574-6976.2010.00247.x.
Henry N, Schultz H, Grubbs N, Muller S, Ilstrup D, Wilson W. Comparison of ciprofloxacin and co-trimoxazole in the treatment of uncomplicated urinary tract infection in women. J Antimicrobl Chemother 1986; 18(Supppl D): 103–106. http://dx.doi.org/https://doi.org/10.1093/jac/18.supplement_d.103.
Higgins JPT, Green S, Editors. Cochrane handbook for systematic reviews of interventions version 5.1.0 [updated march 2011]. London: The Cochrane Collaboration, 2011. Available from www.cochrane-handbook.org. http://dx.doi.org/https://doi.org/10.1002/9780470712184.
Salanti G, Ades A, Lonnidis JP. Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: an overview and tutorial. J Clin Epidemiol 2011; 64: 163–171. http://dx.doi.org/https://doi.org/10.1016/j.jclinepi.2010.03.016.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6(7):e1000100. https://doi.org/10.1371/journal.pmed.1000100.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–88 https://doi.org/10.1016/0197-2456(86)90046-2.
Habord RM, Egger M, Sterne JA. A modified test for small-study effects in meta-analyses of controlled trials with binary endpoints. Stat Med 2006; 25(20): 3443–3457. http://dx.doi.org/https://doi.org/10.1002/sim.2380.
Lu G, Ades AE. Assessing evidence inconsistency in mixed treatment comparisons. J Am Stat Assoc 2006; 101(474): 447–459. http://dx.doi.org/https://doi.org/10.1198/016214505000001302.
Arredondo J, Figueroa R, Rosas A, Jáuregui A, Corral M, Costo A, et al. Comparison of short-term treatment regimen of ciprofloxacin versus long-term treatment regimens of trimethoprim/sulfamethoxazole or norfloxacin for uncomplicated lower urinary tract infections: a randomized, multicentre, open-label, prospective study. J Antimicrob Chemother 2004; 54: 840–843. http://dx.doi.org/https://doi.org/10.1093/jac/dkh414.
Auquer F, Cordón F, Gorina E, Caballero J, Adalid C, Batlle J; Urinary Tract Infection Study Group. Single-dose ciprofloxacin versus 3 days of norfloxacin in uncomplicated urinary tract infections in women. Clin Microbiol Infect, 2002; 8: 50–54. http://dx.doi.org/https://doi.org/10.1046/j.1198-743x.2001.00359.x.
Basista MP. Randomized study to evaluate efficacy and safety of ofloxacin vs. trimethoprim and sulfamethoxazole in treatment of uncomplicated urinary tract infection. Urology 1997; 37(3): 21–27. http://dx.doi.org/https://doi.org/10.1016/0090-4295(91)80092-L.
Cox CE, Serfer HS, Mena HR, Briefer C, Childs SJ, Gordon SF, et al. Ofloxacin versus trimethoprim/sulfamethoxazole in the treatment of uncomplicated urinary tract infection. Clin Ther. 1992;14(3):446–57.
Fourcroy J, Berner B, Chiang Y, Cramer M, Rowe L, Shore N. Efficacy and safety of a novel once-daily extended-release ciprofloxacin tablet formulation for treatment of uncomplicated urinary tract infection in women. Antimicrob Agents Chemother 2005; 49(10): 4137–4143. http://dx.doi.org/https://doi.org/10.1128/AAC.49.10.4137-4143.2005.
Garlando F, Rietiker S, Täuber M, Flepp M, Meier B, Lüthy R. Single-dose ciprofloxacin at 100 versus 250 mg for treatment of uncomplicated urinary tract infections in women. Antimicrob Agents Chemother 1987; 31: 354–356. http://dx.doi.org/https://doi.org/10.1128/aac.31.2.354.
Gomolin I, Siami P, Reuning J, Haverstock D, Heyd A, the Oral Suspension Study Group. Efficacy and safety of ciprofloxacin oral suspension versus trimethoprim-sulfamethoxazole oral suspension for treatment of older women with acute urinary tract infection. J Am Geriatr Soc 2001; 49: 1606–1613. http://dx.doi.org/https://doi.org/10.1046/j.1532-5415.2001.t01-1-49268.x.
Henry D, Bettis R, Riffer E, Haverstock D, Kowalsky S, Manning K, et al. Comparison of once-daily extended-release ciprofloxacin and conventional twice-daily ciprofloxacin for the treatment of uncomplicated urinary tract infection in women. Clin Therap 2002; 24: 2088–2104. http://dx.doi.org/https://doi.org/10.1016/S0149-2918(02)80099-6.
Hooton T, Johnson C, Winter C, Kuwamura L, Rogers M, Roberts P, et al. Single-dose and three-day regimens of ofloxacin versus trimethoprim-sulfamethoxazole for acute cystitits in women. Antimicrob Agents Chemother 1991; 35: 1479–1483. http://dx.doi.org/https://doi.org/10.1128/aac.35.7.1479.
Iravani A. Multicenter study of single-dose and multiple-dose fleroxacin versus ciprofloxacin in the treatment of uncomplicated urinary tract infections. Am J Med. 1993;94(3A):89S–96S.
Iravani A, Tice A, McCarty J, Sikes D, Nolen T, Gallis H, et al. Short-course ciprofloxacin treatment of acute uncomplicated urinary tract infection in women: the minimum effective dose. Arch Int Med, 1995; 155: 485–494. http://dx.doi.org/https://doi.org/10.1001/archinte.1995.00430050061007.
Iravani A, Klimberg I, Briefer C, Munera C, Kowalsky S, Echols R, Urinary tract infection group. A trial comparing low-dose, short-course ciprofloxacin and standard 7 days therapy with co-trimoxazole or nitrofurantoin in the treatment of uncomplicated urinary tract infection. J Antimicrob Chemother 1999; 43(A): 67–75. http://dx.doi.org/https://doi.org/10.1093/jac/43.suppl_1.67.
McCarty J, Richard G, Huck W, Tucker R, Tosiello R, Shan M, et al.; The ciprofloxacin urinary tract infection group. A randomized trial of short course ciprofloxacin, ofloxacin, or trimethoprim/sulfamethoxazole for the treatment of acute urinary tract infection in women. Am J Med 1999; 106: 292–299. http://dx.doi.org/https://doi.org/10.1016/s0002-9343(99)00026-1.
Naber K, Allin D, Clarysse L, Haworth D, James I, Raini C, Scheneider H, Wall A, Weitz P, Hopkins G, Ankel-Fuchs D. Gatifloxacin 400 mg as a single shot or 200 mg once daily for 3 days is as effective as ciprofloxacin 250 mg twice daily for the treatment of patients with uncomplicated urinary tract infections. Int J Antimicrob Agents 2004; 23: 596–605. http://dx.doi.org/https://doi.org/10.1016/j.ijantimicag.2003.12.017.
Pfau A, Sacks T. Single dose quinolone treatment in acute uncomplicated urinary tract infection in women. J Urol, 1993; 149: 532–534. http://dx.doi.org/https://doi.org/10.1016/s0022-5347(17)36137-2.
Richard G, Klimberg I, Fowler C, Callery-D’Amico C, Kim S. Levofloxacin versus ciprofloxacin versus Lomefloxacin in acute pyelonephritis. Urology, 1998; 51: 51–55. http://dx.doi.org/https://doi.org/10.1016/S0090-4295(98)00160-5.
Richard G, DeAbate C, Rouff G, Corrado M, Fowler C, Morgan N. A double-blind, randomized trial of the efficacy and safety of short-course, once-daily levofloxacin versus Ofloxacin twice daily in uncomplicated urinary tract infections. Infect Dis Clin Pract (Baltim Md). 1998;9:323–9.
Ceran N, Mert D, Yuksel F, Erdem I, Adalati R, Ozyurek S, et al. A randomized comparative study of single-dose fosfomycin and 5-day ciprofloxacin in female patients with uncomplicated lower urinary tract infections. J Infect Chemother, 2010; 16: 424–430. http://dx.doi.org/https://doi.org/10.1007/s10156-010-0079-z.
García G, Fava E, Rubio V, Luna J. Infecciones urinarias no complicadas: comparación de una pauta con norfloxacino durante 7 días frente a norfloxacino durante 3 días. Aten Primaria. 2002;29(1):148–9.
Paparo S, De Rosa F, Marangi M, Polimeni A, Bertucci P, Terzaroli P, et al. Ciprofloxacin versus amoxicillin/clavulanic acid in the treatment of urinary tract infection. Med J Infect Parasit Dis. 1994;9:111–3.
Piipo T, Pitkajarvi T, Salo SA. Three-day versus seven days treatment with norfloxacin in acute cystitis. Curr Ther Res Clin Exp. 1990;47(4):644–53.
Trienekens T, London N, Houben A, Dejong R, Stobberingh E. Treating acute urinary tract infections. An RCT of 3-day versus 7-day norfloxacin. Can Fam Physician. 1993;39:514–8.
Vogel T, Verreault R, Gourdeau M. Antibiotic treatment for uncomplicated urinary tract infections in the elderly: a comparison of 3-day and 7-day courses. CMAJ. 2004;170:469–73.
Wagenlehner F, Umeh O, Steenbergen J, Yuan G, Daroviche R. Ceftolozane tazobactam compared with levofloxacin in the treatment of complicated urinary tract infections, including pyelonephritis: a randomized, double-blind, phase 3 trial (ASPECT-cUTI). Lancet, 2015; 385: 1949–1956. http://dx.doi.org/https://doi.org/10.1016/S0140-6736(14)62220-0.
Sotomayor M. Ponce de León A, Guzmán J, Rosas E, Rodríguez F, González A, et al. Recomendaciones de expertos mexicanos en el tratamiento de las infecciones del tracto urinario en pacientes adultos, embarazadas y niños. Rev Mex Urol. 2015;75(2):1–46.
Alonso MD, Marcos C, Davila I, de la Hoz B, Martin JA, Parra F, et al. Hipersensitivity to trimethoprim. Allergy 1992;47(1): 340–42. https://doi.org/10.1111/j.1398-9995.1992.tb02067.x.
Khan D, Knowless S, Shea N. Sulfonamide hypersensitivity: fact and fiction. J Aller C Imm-Pract. 2019;7(7):2116–23. https://doi.org/10.1016/j.jaip.2019.05.034.
Demoleas S, Davies G. Quinolones antibiotics of the future. J Am Podiatr Med Assoc. 1988;78(10):522–5. https://doi.org/10.7547/87507315-78-10-522.
Dembry L, Farrinton J, Andriole V. Fluoroquinolone antibiotics: adverse effects and safety profiles. Infect Dis Clin Pract. 1999;8:421–8.
Acknowledgments
We thank Deborah H. S. for English language editing.
Funding
Senosiain Laboratories S.A. provided only financial support for the acquisition of articles but was not involved in the research, the collection, analysis or interpretation of data or in the writing of the manuscript. The authors declare that they have no conflict of interest or disclosures and received no compensation from Senosiain Laboratories S.A. for their work in the writing of this manuscript.
This manuscript is derived from the project registered with the number 2019/018 approved by the Research Committee of Instituto Nacional de Pediatría.
Author information
Authors and Affiliations
Contributions
A González-Garay contributed to the conceptualization, writing draft and review, methodology, resources, formal analysis, investigation and supervision of this work.
L Velasco-Hidalgo contributed to the conceptualization, writing draft, methodology, formal analysis, investigation and supervision of this work.
E Ochoa-Hein contributed to the conceptualization, validation, investigation, editing, visualization, supervision, writing review and editing of this manuscript.
R Rivera-Luna contributed to the conceptualization, methodology, resources, validation, visualization, writing review and editing of this manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors of this review declare that we have no significant competing financial, professional or personal interests that might have influenced the performance or presentation of the work described in this manuscript.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
González-Garay, A., Velasco-Hidalgo, L., Ochoa-Hein, E. et al. Efficacy and safety of quinolones for the treatment of uncomplicated urinary tract infections in women: a network meta-analysis. Int Urogynecol J 32, 3–15 (2021). https://doi.org/10.1007/s00192-020-04255-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-020-04255-y