Abstract
Introduction
Urogynaecological conditions have been shown to negatively impact on body image in a number of previous studies. ePAQ-Pelvic Floor (ePAQ-PF) is a patient-reported outcome measure used in clinical practice to assess urogynaecological conditions and their impact on quality of life. This study aimed to develop and undertake initial psychometric testing of a new domain to assess urogynaecological body image within ePAQ-PF.
Methods
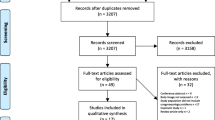
A patient involvement group, analysis of free-text data from ePAQ-PF and a systematic review of existing PROMs assessing urogynaecological body image informed the content of a new body-image domain within ePAQ-PF. This was administered to 208 patients who consented to the use of their anonymised ePAQ-PF responses for research purposes. These data underwent factor analysis, internal consistency reliability and item-total correlation testing. Evidence-based hypotheses were formulated to test construct validity. Criterion validity was assessed against the Body-image Scale (BIS). Patients completed a separate questionnaire (QQ-11) to measure the face validity of ePAQ-PF.
Results
Factor analysis revealed a four-item body-image domain with good internal consistency reliability (Cronbach’s α = 0.899) and item-total correlation (Spearman’s rank r > 0.40). ePAQ-PF body-image domain scores correlated significantly with the BIS scores (r = 0.501). Age, prolapse, sexual dysfunction, pelvic pain and urinary incontinence scores correlated significantly with body-image domain score. QQ-11 value scores demonstrated good acceptability.
Conclusions
Body-image assessment should form part of routine care in urogynaecology. Preliminary results support the validity, reliability and functionality of the body-image domain in ePAQ-PF. Further psychometric testing of this is required, including tests of responsiveness and stability.


Similar content being viewed by others
References
Cash TF. Body-image: past, present, and future. Body-image. 2004;1(1):1–5.
Tylka TL. Body-image: celebrating the past, appreciating the present, and envisioning the future. Body-image. 2018;24:A1–3.
Waltner R. Genital identity: a core component of sexual- and self-identity. Journal of Sex Research. 1986;22:399–408.
Berman L, Miles M, Pollets D, Powell JA. Genital self-image as a component of sexual health: relationship between genital self-image, female sexual function, and quality of life measures. Journal of Sex & Marital Therapy. 2003;29:11–21.
Lowenstein L, Gamble T, Deniseiko Sanses TV, Van Raalte H, Carberry C, Jakus S, et al. Sexual function is related to body image perception in women with pelvic organ prolapse. Journal of Sexual Medicine. 2009;6(8):2286–91.
Jelovsek JE, Barber MD. Women seeking treatment for advanced pelvic organ prolapse have decreased body image and quality of life. Am J Obstet Gynecol. 2006;194(5):1455–61.
Zielinski R, Low LK, Tumbarello J, Miller JM. Body image and sexuality in women with pelvic organ prolapse. Urol Nurs. 2009;29(4):239.
Handelzalts JE, Yaakobi T, Levy S, Peled Y, Wiznitzer A, Krissi H. The impact of genital self-image on sexual function in women with pelvic floor disorders. European Journal of Obstetrics & Gynecology and Reproductive Biology. 2017;211:164–8.
Gray T, Li W, Campbell P, Jha S, Radley S. Evaluation of coital incontinence by electronic questionnaire: prevalence, associations and outcomes in women attending a urogynaecology clinic. Int Urogynecol J. 2018;29(7):969–78.
Gray T, Vickers H, Jha S, Jones G, Brown S, Radley S. A systematic review of non-invasive modalities used to identify women with anal incontinence symptoms after childbirth. Int Urogynecol J. 2019;30(6):869–79.
Radley SC, Jones GL, Tanguy EA, Stevens VG, Nelson C, Mathers NJ. Computer interviewing in urogynaecology: concept, development and psychometric testing of an electronic pelvic floor assessment questionnaire in primary and secondary care. BJOG Int J Obstet Gynaecol. 2006;113(2):231–8.
Jones GL, Radley SC, Lumb J, Jha S. Electronic pelvic floor symptoms assessment: tests of data quality of ePAQ-PF. Int Urogynecol J. 2008;19(10):1337–47.
Dua A, Jones G, Wood H, Sidhu H. Understanding women’s experiences of electronic interviewing during the clinical episode in urogynaecology: a qualitative study. Int Urogynecol J. 2013;24(11):1969–75.
Gray T, Strickland S, Pooranawattanakul S, Li W, Campbell P, Jones G, et al. What are the concerns and goals of women attending a urogynaecology clinic? Thematic analysis of free-text data from a patient reported outcome measure. International Urogynaecology Journal. 2018;30(1):33–41.
Gray TG, Sneyd R, Scurr K, Jones GL, Iles D, Jha S, et al. Patient-reported outcome measures which assess body-image in urogynaecology patients: a systematic review. International Urogynaecology Journal. 2019;30(5):673–81.
Field A. Discovering statistics using IBM SPSS statistics, 4th ed. London: Sage Publications; 2013. Section 17.4
Gray TG, Alexander C, Jones GL, Tidy JA, Palmer JE, Radley SC. Development and psychometric testing of an electronic patient-reported outcome tool for Vulval disorders (ePAQ-vulva). Journal of Lower Genital Tract Disease. 2017;21(4):319–26.
Bolarinwa OA. Principles and methods of validity and reliability testing of questionnaires used in social and health science researches. Nigerian Postgraduate Medical Journal. 2015;22:195–201.
Hopwood P, Fletcher I, Lee A, Al GS. A body image scale for use with cancer patients. Eur J Cancer. 2001;37(2):189–97.
Moores KL, Jones GL, Radley SC. Development of an instrument to measure face validity, feasibility and utility of patient questionnaire use during health care: the QQ-10. Int J Qual Health Care. 2012;24(5):517–24.
Terwee CB, Bot SDM, De Boer MR, Van Der Windt DAWM, Knol DL, Dekker J, et al. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol. 2007;60:34–42.
Hunter MM, Nakagawa S, Van Den Eeden SK, Kuppermann M, Huang AJ. Predictors of impact of vaginal symptoms in postmenopausal women. Menopause. 2016;21(2):129–39.
Boyer SC, Pukall CF. Pelvic examination experiences in women with and without chronic pain during intercourse. Journal of Sexual Medicine. 2014;11(12):3035–50.
Bachman JW. The patient-computer interview: a neglected tool that can aid the clinician. Mayo Clinic Proceedings. Mayo Foundation for Medical Education and Research. 2003;78(1):67–78.
McCambridge J, Witton J, Elbourne DR. Systematic review of the Hawthorne effect: new concepts are needed to study research participation effects. J Clin Epidemiol. 2014;67(3):267–77.
McDermott E, Moloney J, Rafter N, Keegan D, Byrne K, Doherty GA, Cullen G, Malone K, Mulcahy HE. The Body-image Scale: A simple and valid tool for assessing body-image dissatisfaction in inflammatory bowel disease. 2018;20(2):286–290.
Chiara G, Piccioni V, Perino M, Ohlmeier U, Fassino S, Leombruni P. Psychological investigation in female patients suffering from urinary incontinence. Int Urogynecol J. 1998;9(2):73–7.
Debus G, Kästner R. Psychosomatic aspects of urinary incontinence in women. Geburtshilfe Frauenheilkd. 2015;75(2):165–9.
Bergeron S, Morin M, Lord M-J. Integrating pelvic floor rehabilitation and cognitive-behavioural therapy for sexual pain: what have we learned and where do we go from here? Sex Relatsh Ther. 2010;25(3):289–98.
National Institute for health and care excellence (2019). Urinary incontinence and pelvic organ prolapse in women: management NG23. Available at: https://www.nice.org.uk/guidance/ng123/resources/urinary-incontinence-and-pelvic-organ-prolapse-in-women-management-pdf-66141657205189 [Accessed 10th December 2019].
Author information
Authors and Affiliations
Contributions
Scurr: Project development, Data collection, management and analysis, Manuscript writing.
Gray: Project development, Data collection and analysis, Manuscript writing.
Jones: Data analysis, Manuscript editing.
Radley: Project development, Manuscript editing.
Corresponding author
Ethics declarations
Financial disclaimers/conflict of interest statement
Professor Stephen Radley is a director and shareholder of ePAQ Systems Limited, an NHS spin-out technology company largely owned by Sheffield Teaching Hospitals NHS Foundation Trust. Professor Radley did not collect or analyse any data included in this study. The other authors have no financial or commercial interests in ePAQ Systems Limited and no other conflicts of interests to declare. No funding was received for this study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Scurr, K., Gray, T.G., Jones, G.L. et al. Development and initial psychometric testing of a body-image domain within an electronic pelvic floor questionnaire (ePAQ-pelvic floor). Int Urogynecol J 31, 1245–1253 (2020). https://doi.org/10.1007/s00192-020-04247-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-020-04247-y