Abstract
Introduction and hypothesis
Conservative treatment is recommended as first-line therapy for stress urinary incontinence (SUI). We hypothesized that CO2 laser treatment would demonstrate safety and efficacy for women with SUI.
Methods
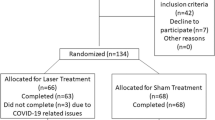
A prospective, open-label, cohort study of 33 women (mean age 43 years) referred from a continence clinic after urologist/urogynecologist assessment, with a verified stress urinary incontinence diagnosis based on urodynamic testing. The participants completed three outpatient treatments with laser therapy and were subsequently evaluated at 1, 3 and 6 months. The independent t and chi-square tests were used to assess changes in sanitary pad usage and SUI symptoms.
Results
Sanitary pad usage decreased from a median of 12 per day at baseline to 7 at 1–3 months post-treatment (P < 0.0001) and returned to 12 at 6 months post-treatment. Scores on the Urogenital Distress Inventory and the International Consultation of Incontinence Questionnaire decreased (improved) significantly at 1–3 months post-treatment: from 45 ± 2 and 16 ± 4, respectively, to 29.3 ± 14.7 and 8.15 ± 3.1, respectively (P < 0.0001). The scores returned to levels similar to baseline at 6 months after treatment. Participants reported mild and transient side effects, with significant improvement in quality of life.
Conclusions
Laser therapy can be an optional conservative treatment for women who seek minimally invasive non-surgical treatment for the management of SUI. No serious adverse effects were reported though the sample size was not large, a possible limitation of the study. Further large randomized control trials are needed to appraise the efficacy and safety of laser therapy for stress urinary incontinence and to demonstrate the ultimate utility of this modality.

Similar content being viewed by others
References
Castro RA, Arruda RM, Bortolini MA. Female urinary incontinence: effective treatment strategies. Climacteric: the journal of the International Menopause Society. 2015;18:135–41.
MacLennan AH, Taylor AW, Wilson DH, Wilson D. The prevalence of pelvic floor disorders and their relationship to gender, age, parity and mode of delivery. BJOG: an international journal of obstetrics and gynaecology. 2000;107:1460–70.
Norton P, Brubaker L. Urinary incontinence in women. Lancet. 2006;367:57–67.
Nystrom E, Sjostrom M, Stenlund H, Samuelsson E. ICIQ symptom and quality of life instruments measure clinically relevant improvements in women with stress urinary incontinence. Neurourol Urodyn. 2015;34:747–51.
Gil KM, Somerville AM, Cichowski S, Savitski JL. Distress and quality of life characteristics associated with seeking surgical treatment for stress urinary incontinence. Health Qual Life Outcomes. 2009;7:8.
Urinary incontinence and pelvic organ prolapse in women: management National Institute for Health and Care Excellence (NICE) guideline [NG123].
Bump RC, Norton PA, Zinner NR, Yalcin I. Mixed urinary incontinence symptoms: urodynamic findings, incontinence severity, and treatment response. Obstet Gynecol. 2003;102:76–83.
Schimpf MO, Rahn DD, Wheeler TL, et al. Sling surgery for stress urinary incontinence in women: a systematic review and metaanalysis. Am J Obstet Gynecol. 2014;211:71 e1–71 e27.
Barski D, Gerullis H, Georgas E, et al. Coating of mesh grafts for prolapse and urinary incontinence repair with autologous plasma: exploration stage of a surgical innovation. Biomed Res Int. 2014;2014:296498.
Maher C, Feiner B, Baessler K, Christmann-Schmid C, Haya N, Brown J. Surgery for women with anterior compartment prolapse. Cochrane Database Syst Rev. 2017;11:Cd004014.
Surgical Mesh for Transvaginal Repair of Pelvic Organ Prolapse in the Anterior Vaginal Compartment. FDA Executive Summary. https://www.fda.gov/media/122854. Accessed July 20 2019.
Arunkalaivanan A, Kaur H, Onuma O. Laser therapy as a treatment modality for genitourinary syndrome of menopause: a critical appraisal of evidence. Int Urogynecol J. 2017;28:681–5.
Gambacciani M, Levancini M. Short-term effect of vaginal erbium laser on the genitourinary syndrome of menopause. Minerva Ginecol. 2015;67:97–102.
Salvatore S, Nappi RE, Zerbinati N, et al. A 12-week treatment with fractional CO2 laser for vulvovaginal atrophy: a pilot study. Climacteric: the journal of the International Menopause Society. 2014;17:363–9.
Salvatore S, Leone Roberti Maggiore U, Athanasiou S, et al. Histological study on the effects of microablative fractional CO2 laser on atrophic vaginal tissue: an ex vivo study. Menopause. 2015;22:845–9.
Hutchinson-Colas J, Segal S. Genitourinary syndrome of menopause and the use of laser therapy. Maturitas. 2015;82:342–5.
Pieralli A, Fallani MG, Becorpi A, et al. Fractional CO2 laser for vulvovaginal atrophy (VVA) dyspareunia relief in breast cancer survivors. Arch Gynecol Obstet. 2016;294:841–6.
Arroyo C. Fractional CO2 laser treatment for vulvovaginal atrophy symptoms and vaginal rejuvenation in perimenopausal women. Int J Women’s Health. 2017;9:591–5.
Pagano T, De Rosa P, Vallone R, et al. Fractional microablative CO2 laser for vulvovaginal atrophy in women treated with chemotherapy and/or hormonal therapy for breast cancer: a retrospective study. Menopause. 2016;23:1108–13.
Gambacciani M, Levancini M. Vaginal erbium laser as second-generation thermotherapy for the genitourinary syndrome of menopause: a pilot study in breast cancer survivors. Menopause. 2017;24:316–9.
Sokol ER, Karram MM. An assessment of the safety and efficacy of a fractional CO2 laser system for the treatment of vulvovaginal atrophy. Menopause. 2016;23:1102–7.
Salvatore S, Nappi RE, Parma M, et al. Sexual function after fractional microablative CO(2) laser in women with vulvovaginal atrophy. Climacteric: the journal of the International Menopause Society. 2015;18:219–25.
Fistonic N, Fistonic I, Gustek SF, et al. Minimally invasive, non-ablative Er:YAG laser treatment of stress urinary incontinence in women--a pilot study. Lasers Med Sci. 2016;31:635–43.
Ogrinc UB, Sencar S, Lenasi H. Novel minimally invasive laser treatment of urinary incontinence in women. Lasers Surg Med. 2015;47:689–97.
Filippini M, Del Duca E, Negosanti F, et al. Fractional CO2 laser: from skin rejuvenation to Vulvo-vaginal reshaping. Photomed Laser Surg. 2017;35:171–5.
Lee MS. Treatment of vaginal relaxation syndrome with an erbium:YAG laser using 90 degrees and 360 degrees scanning scopes: a pilot Study & Short-term Results. Laser therapy. 2014;23:129–38.
Lev-Sagie A, Kopitman A, Brzezinski A. Low-level laser therapy for the treatment of provoked Vestibulodynia-a randomized, placebo-controlled pilot trial. J Sex Med. 2017;14:1403–11.
Murina F, Karram M, Salvatore S, Felice R. Fractional CO2 laser treatment of the vestibule for patients with Vestibulodynia and genitourinary syndrome of menopause: a pilot study. J Sex Med. 2016;13:1915–7.
Drnovsek-Olup B, Beltram M, Pizem J. Repetitive Er:YAG laser irradiation of human skin: a histological evaluation. Lasers Surg Med. 2004;35:146–51.
Zerbinati N, Serati M, Origoni M, et al. Microscopic and ultrastructural modifications of postmenopausal atrophic vaginal mucosa after fractional carbon dioxide laser treatment. Lasers Med Sci. 2015;30:429–36.
Poon VK, Huang L, Burd A. Biostimulation of dermal fibroblast by sublethal Q-switched Nd:YAG 532 nm laser: collagen remodeling and pigmentation. J Photochem Photobiol B. 2005;81:1–8.
Jiang X, Ge H, Zhou C, Chai X, Ren QS. The role of vascular endothelial growth factor in fractional laser resurfacing with the carbon dioxide laser. Lasers Med Sci. 2012;27:599–606.
Chan SS, Cheung RY, Lai BP, Lee LL, Choy KW, Chung TK. Responsiveness of the pelvic floor distress inventory and pelvic floor impact questionnaire in women undergoing treatment for pelvic floor disorders. Int Urogynecol J. 2013 Feb;24(2):213–21.
Lin HY, Tsai HW, Tsui KH, et al. The short-term outcome of laser in the management of female pelvic floor disorders: focus on stress urine incontinence and sexual dysfunction. Taiwanese journal of obstetrics & gynecology. 2018;57:825–9.
Lin KL, Chou SH, Long CY. Effect of Er:YAG laser for women with stress urinary incontinence. Biomed Res Int. 2019;2019:7915813.
Blaganje M, Scepanovic D, Zgur L, Verdenik I, Pajk F, Lukanovic A. Non-ablative Er:YAG laser therapy effect on stress urinary incontinence related to quality of life and sexual function: a randomized controlled trial. Eur J Obstet Gynecol Reprod Biol. 2018;224:153–8.
Lin YH, Hsieh WC, Huang L, Liang CC. Effect of non-ablative laser treatment on overactive bladder symptoms, urinary incontinence and sexual function in women with urodynamic stress incontinence. Taiwanese journal of obstetrics & gynecology. 2017;56:815–20.
Gonzalez Isaza P, Jaguszewska K, Cardona JL, Lukaszuk M. Long-term effect of thermoablative fractional CO2 laser treatment as a novel approach to urinary incontinence management in women with genitourinary syndrome of menopause. Int Urogynecol J. 2018;29:211–5.
Gaspar A, Brandi H. Non-ablative erbium YAG laser for the treatment of type III stress urinary incontinence (intrinsic sphincter deficiency). Lasers Med Sci. 2017;32:685–91.
Neimark AI, Yakovleva AY, Lapii GA. Outcomes of ER:YAG LASER treatment of stress urinary incontinence in women. Urologiia. 2018:20–5.
Tien YW, Hsiao SM, Lee CN, Lin HH. Effects of laser procedure for female urodynamic stress incontinence on pad weight, urodynamics, and sexual function. Int Urogynecol J. 2017;28:469–76.
US Food and Drug Administration. FDA Warns Against Use of Energy-Based Devices to Perform Vaginal “Rejuvenation” or Vaginal Cosmetic Procedures [Internet]. FDA Safety Communications.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dabaja, H., Lauterbach, R., Matanes, E. et al. The safety and efficacy of CO2 laser in the treatment of stress urinary incontinence. Int Urogynecol J 31, 1691–1696 (2020). https://doi.org/10.1007/s00192-019-04204-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-019-04204-4