Abstract
Introduction
Self-management with clinician guidance is a cornerstone of successful conservative treatment for accidental bowel leakage (ABL). There are currently few resources to assist patients with that essential self-management. The purpose of this study was to describe self-management of ABL and explore interest in a mobile health application (m-Health app) for supporting ABL self-management among community-living women.
Methods
Using an observational/descriptive design, women (18+ years) previously seen in a urogynecology clinic for ABL were mailed a survey containing eight multiple-choice questions and an open-ended prompt for comments.
Results
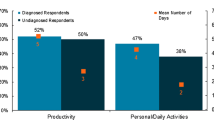
Survey responses were received from 161 women (18% response rate). The highest percentage of participants was aged 61–70 years (39%). Nearly half of the participants (47%) “did not know anything” about ABL self-management before visiting a clinician. Only 4% “knew a lot.” Of those who have been trying to self-manage their ABL (n = 132), 37% reported that it was not effective, and only 5% thought their self-management was “very effective.” Half (50%) of the participants had “a lot of” interest in an m-Health app to support managing ABL, and 30% had “some” interest. The vast majority (89%) thought that it was “very important” to have ongoing guidance and support for self-managing ABL.
Conclusions
Before visiting a clinician, most women with ABL lacked knowledge about ABL self-management, and their self-management was not very effective. Women thought having guidance to self-manage ABL was important. There would be good interest among women in an m-Health app supporting self-management of ABL if one were created.



Similar content being viewed by others
References
Milsom I, Altman D, Cartwright R, Lapitan MC, Nelson R, Sjostrom S, et al. Epidemiology of urinary incontinence (UI) and other lower urinary tract symptoms (LUTS), pelvic organ prolapse (POP) and anal incontinence (AI). In: Abrams P, Cardozo L, Wagg A, Wein A, editors. Incontinence. 6th ed. Bristol, UK: International Continence Society; 2017. p. 1–142.
Richter HE, Nager CW, Burgio KL, Whitworth R, Weidner AC, Schaffer J, et al. Incidence and predictors of anal incontinence after obstetric anal sphincter injury in primiparous women. Female Pelvic Med Reconstruct Surg. 2015;21(4):182–9.
Tejedor P, Bodega-Quiroga I, Plaza J, Ortega-López M, Gutiérrez C, García-Olmo D, et al. Quality of life and 3D-EUS assessment for anal incontinence after childbirth. Revista Espanola de Enfermedades Digestivas: Organo Oficial de la Sociedad Espanola de Patologia Digestiva 2019;111.
Bliss D, Mimura T, Berghmans B, Bharucha A, Chiarioni G, Emmanuel A, et al. Assessment and conservative management of faecal incontinence and quality of life in adults. In: Abrams P, Cardozo L, Wagg A, Wein A, editors. Incontinence. 6 ed. Bristol, UK: International Continence Society; 2017. p. 1993–2085.
Meyer I, Richter HE. Impact of fecal incontinence and its treatment on quality of life in women. Women’s Health. 2015;11(2):225–38.
Peden-McAlpine C, Bliss D, Hill J. The experience of community-living women managing fecal incontinence. West J Nurs Res. 2008;30(7):817–35.
Tsuji I, Whalen S, Finucane TE. Predictors of nursing home placement in community-based long-term care. J Am Geriatr Soc. 1995;43(7):761–6.
Di Rosa M, Lamura G. The impact of incontinence management on informal caregivers’ quality of life. Aging Clin Experiment Res. 2016;28(1):89–97.
Bliss DZ. Management of Fecal Incontinence for the advanced practice nurse. Paris, FR: Springer; 2018.
Whitehead WE, Palsson OS, Simren M. Treating fecal incontinence an unmet need in primary care medicine. N C Med J. 2016;77(3):211–5.
Krebs P, Duncan DT. Health app use among US mobile phone owners: A national survey. JMIR mHealth and uHealth. 2015;3(4).
Martínez-Pérez B, De La Torre-Díez I, López-Coronado M. Mobile health applications for the most prevalent conditions by the World Health Organization: Review and analysis. Journal of Medical Internet Research. 2013;15(6).
Asklund I, Nystrom E, Sjostrom M, Umefjord G, Stenlund H, Samuelsson E. Mobile app for treatment of stress urinary incontinence: A randomized controlled trial. Neurourol Urodynam. 2017;36(5):1369–76.
Hoffman V, Soderstrom L, Samuelsson E. Self-management of stress urinary incontinence via a mobile app: two-year follow-up of a randomized controlled trial. Acta Obstet Gynecol Scand. 2017;96(10):1180–7.
Hartigan JA, Kleiner B. Mosaics for Contingency Tables. 13th Symposium on the Interface. New York: Springer; 1981. p. 268–73.
Wilkinson A, Whitehead L. Evolution of the concept of self-care and implications for nurses: A literature review. Int J Nurs Stud. 2009;46(8):1143–7.
Bliss DZ, Fischer LR, Savik K. Managing fecal incontinence: self-care practices of older adults. J Gerontol Nurs. 2005;31(7):35–44.
Thekkinkattil D, Lim M, Finan P, Sagar P, Burke D. Awareness of investigations and treatment of faecal incontinence among the general practitioners: A postal questionnaire survey. Color Dis. 2008;10(3):263–7.
Dunivan GC, Heymen S, Palsson OS, von Korff M, Turner MJ, Melville JL, et al. Fecal incontinence in primary care: Prevalence, diagnosis, and health care utilization. Am J Obstetr Gynecol. 2010;202(5):493.e1–6.
Olsson F, Bertero C. Living with faecal incontinence: trying to control the daily life that is out of control. J Clin Nurs. 2015;24(1–2):141–50.
Peden-McAlpine C, Bliss D, Becker B, Sherman S. The experience of community-living men managing fecal incontinence. Rehab Nursing. 2012;37(6):298–306.
Ernsting C, Dombrowski SU, Oedekoven M, Lo J, Kanzler M, Kuhlmey A, et al. Using smartphones and health apps to change and manage health behaviors: A population-based survey. J Med Internet Res. 2017;19(4):e101.
Bhuyan SS, Lu N, Chandak A, Kim H, Wyant D, Bhatt J, et al. Use of mobile health applications for health-seeking behavior among US adults. J Med Syst. 2016;40(6):153.
Conn J. Easy on those apps: Mobile medical apps gain support, but may lack clinical evidence: Modern Healthcare; 2015 [45:[Available from: http://www.modernhealthcare.com/article/20151128/MAGAZINE/311289981.
Dahlke DV, Ory MG. mHealth Applications Use and Potential for Older Adults, Overview of. Encyclopedia of Geropsychology, 2016. p. 1–9.
Pepper J, Zhang A, Li R, Wang XH. Usage results of a mobile app for managing urinary incontinence. J Urol. 2015;193(4):1292–7.
Levine DM, Lipsitz SR, Linder JA. Trends in seniors’ use of digital health technology in the United States, 2011-2014. J Am Med Assoc. 2016;316(5):538–40.
Anderson M, Perrin A. Tech adoption climbs among older adults: pew research center; 2017 [1-22]. Available from: https://www.pewinternet.org/2017/05/17/tech-adoption-climbs-among-older-adults/.
Anderson G. Technology use and attitudes among mid-life and older Americans: AARP; 2017 [Available from: https://www.aarp.org/content/dam/aarp/research/surveys_statistics/technology/info-2018/atom-nov-2017-tech-module.doi.10.26419%252Fres.00210.001.pdf.
Mitzner TL, Boron JB, Fausset CB, Adams AE, Charness N, Czaja SJ, et al. Older adults talk technology: technology usage and attitudes. Comput Hum Behav. 2010;26(6):1710–21.
Typical Response Rates for Common Survey Types: Survey Gizmo blog. [Available from: https://www.surveygizmo.com/resources/blog/survey-response-rates/.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
This study was funded in part by internal funds from the University of Minnesota School of Nursing, Minneapolis, MN. The authors have no conflicts of interest regarding this study to declare.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Conference Presentations
International Continence Society annual meeting podium presentation, Philadelphia, PA, US, August 2018
Rights and permissions
About this article
Cite this article
Bliss, D.Z., Gurvich, O.V., Patel, S. et al. Self-management of accidental bowel leakage and interest in a supportive m-Health app among women. Int Urogynecol J 31, 1133–1140 (2020). https://doi.org/10.1007/s00192-019-04192-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-019-04192-5