Abstract
Introduction and hypothesis
To describe associations between postoperative genital hiatus (GH) measurements and long-term anatomical and subjective outcomes following pelvic reconstructive surgery involving apical suspension.
Methods
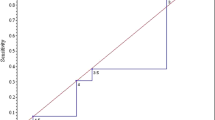
This IRB-approved secondary analysis reports outcomes 3–7 years following robotic sacrocolpopexy (RSC) and uterosacral ligament suspension (USLS). Objective and subjective measures were obtained through clinical examinations and validated questionnaires. Subjective success was defined as the absence of a symptomatic bulge or retreatment. Objective success was defined as all Pelvic Organ Prolapse Quantification (POP-Q) points at or above −1 at the long-term examination. Postoperative GH measures were obtained at 6 weeks (early) and 3–7 years (long term) postoperatively. GH measurements were classified as either normal (<4 cm) or wide (≥4 cm). Logistic regression identified associations between postoperative GH measurements and long-term subjective and objective outcomes.
Results
A total of 154 subjects completed long-term POP-Q examinations (74 RSC and 80 USLS). The median time to follow-up (minimum, maximum) was 59 months (range 34–89); 97.4% were Caucasian. Subjective success was achieved in 134 (87%), and objective success in 139 (90.2%) subjects. The majority (79%) underwent a posterior repair during their index surgery. An early postoperative GH of less than 4 cm was associated with an 11-fold higher likelihood of subsequent objective success (11.8, 2.7–51.7; p = 0.001). Furthermore, a postoperative GH less than 4 cm was not associated with dyspareunia at long-term follow-up.
Conclusions
Early postoperative GH <4 cm was associated with superior long-term objective success, without increasing dyspareunia. These data support correcting GH to <4 cm during prolapse repair with apical suspension to reduce objective long-term failure.
Similar content being viewed by others
References
Kelly HA. Gynecology. New York; London: Appleton; 1928.p. 265–7.
Berglas B, Rubin IC. Study of the supportive structures of the uterus by levator myography. Surg Gynecol Obstet. 1953;97(6):677–92.
Phaneuf LE. Inversion of the vagina and prolapse of the cervix following supracervical hysterectomy and inversion of the vagina following total hysterectomy. Am J Obstet Gynecol. 1952;64(4):739–45.
Lowder JL, Oliphant SS, Shepherd JP, Ghetti C, Sutkin G. Genital hiatus size is associated with and predictive of apical vaginal support loss. Am J Obstet Gynecol. 2016;214(6):718.e1–8.
Vaughan MH, Siddiqui NY, Newcomb LK, Weidner AC, Kawasaki A, Visco AG, et al. Surgical alteration of genital Hiatus size and anatomic failure after vaginal vault suspension. Obstet Gynecol. 2018;131(6):1137–44.
Bradley MS, Askew AL, Vaughan MH, Kawasaki A, Visco AG. Robotic-assisted sacrocolpopexy: early postoperative outcomes after surgical reduction of enlarged genital hiatus. Am J Obstet Gynecol. 2018;218(5):514.e1–8.
Smith BC, Crisp CC, Kleeman SD, Yook E, Pauls RN. Uterosacral ligament suspension versus robotic Sacrocolpopexy for treatment of apical pelvic organ prolapse. Female Pelvic Med Reconstr Surg. 2019;25(2):93–8.
Srikrishna S, Robinson D, Cardozo L. Validation of the patient global impression of improvement (PGI-I) for urogenital prolapse. Int Urogynecol J. 2010;21(5):523–8.
Barber MD, Walters MD, Cundiff GW. Responsiveness of the pelvic floor distress inventory (PFDI) and pelvic floor impact questionnaire (PFIQ) in women undergoing vaginal surgery and pessary treatment for pelvic organ prolapse. Am J Obstet Gynecol. 2006;194(5):1492–8.
Barber MD, Chen Z, Lukacz E, Markland A, Wai C, Brubaker L, et al. Further validation of the short form versions of the pelvic floor distress inventory (PFDI) and pelvic floor impact questionnaire (PFIQ). Neurourol Urodyn. 2011;30(4):541–6.
Wren PA, Janz NK, Brubaker L, Fitzgerald MP, Weber AM, LaPorte FB, et al. Reliability of health-related quality-of-life measures 1 year after surgical procedures for pelvic floor disorders. Am J Obstet Gynecol. 2005;192(3):780–8.
Rogers RG, Coates KW, Kammerer-Doak D, Khalsa S, Qualls C. A short form of the pelvic organ prolapse/urinary incontinence sexual questionnaire (PISQ-12). Int Urogynecol J. 2003;14(3):164–8.
Rogers RG, Kammerer-Doak D, Villarreal A, Coates K, Qualls C. A new instrument to measure sexual function in women with urinary incontinence or pelvic organ prolapse. Am J Obstet Gynecol. 2001;184(4):552–8.
Bump RC, Mattiasson A, Bø K, Brubaker LP, DeLancey JOL, Klarskov P, et al. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol. 1996;175(1):10–7.
Porges RF, Porges JC. Theoretical and practical aspects of the surgical correction of pelvic relaxation. Obstet Gynecol. 1967;29(3):450–5.
Nichols DH, Milley PS, Randall CL. Significance of restoration of normal vaginal depth and axis. Obstet Gynecol. 1970;36(2):251–6.
Inmon WB. Suspension of the vaginal cuff and posterior repair following vaginal hysterectomy. Am J Obstet Gynecol. 1974;120(7):977–82.
DeLancey JO. Anatomic aspects of vaginal eversion after hysterectomy. Am J Obstet Gynecol. 1992;166(6 Pt 1):1717–24 discussion 24-8.
Delancey JO, Hurd WW. Size of the urogenital hiatus in the levator ani muscles in normal women and women with pelvic organ prolapse. Obstet Gynecol. 1998;91(3):364–8.
Ghetti C, Gregory WT, Edwards SR, Otto LN, Clark AL. Severity of pelvic organ prolapse associated with measurements of pelvic floor function. Int Urogynecol J Pelvic Floor Dysfunct. 2005;16(6):432–6.
Vakili B, Zheng YT, Loesch H, Echols KT, Franco N, Chesson RR. Levator contraction strength and genital hiatus as risk factors for recurrent pelvic organ prolapse. Am J Obstet Gynecol. 2005;192(5):1592–8.
Medina CA, Candiotti K, Takacs P. Wide genital hiatus is a risk factor for recurrence following anterior vaginal repair. Int J Gynaecol Obstet. 2008;101(2):184–7.
Yousuf A, Chen L, Larson K, Ashton-Miller JA, DeLancey JO. The length of anterior vaginal wall exposed to external pressure on maximal straining MRI: relationship to urogenital hiatus diameter, and apical and bladder location. Int Urogynecol J. 2014;25(10):1349–56.
Grimes CL, Lukacz ES, Gantz MG, Warren LK, Brubaker L, Zyczynski HM, et al. What happens to the posterior compartment and bowel symptoms after sacrocolpopexy? Evaluation of 5-year outcomes from E-CARE. Female Pelvic Med Reconstr Surg. 2014;20(5):261–6.
Mueller MG, Jacobs KM, Mueller ER, Abernethy MG, Kenton KS. Outcomes in 450 women after minimally invasive abdominal sacrocolpopexy for pelvic organ prolapse. Female Pelvic Med Reconstr Surg. 2016;22(4):267–71.
Carter-Brooks CM, Lowder JL, Du AL, Lavelle ES, Giugale LE, Shepherd JP. Restoring genital hiatus to normative values after apical suspension alone versus with level 3 support procedures. Female Pelvic Med Reconstr Surg. 2017;25(3):226-230.
Barber MD, Brubaker L, Nygaard I, Wheeler TL 2nd, Schaffer J, Chen Z, et al. Defining success after surgery for pelvic organ prolapse. Obstet Gynecol. 2009;114(3):600–9.
Sources of support
The parent study was supported by an educational grant from the TriHealth Medical Education Research Fund.
National Trials Registry: NCT02741830.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hill, A.M., Shatkin-Margolis, A., Smith, B.C. et al. Associating genital hiatus size with long-term outcomes after apical suspension. Int Urogynecol J 31, 1537–1544 (2020). https://doi.org/10.1007/s00192-019-04138-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-019-04138-x