Abstract
Introduction and hypothesis
The aim of this study was to report the long-term subjective and objective outcomes after transvaginal mesh (TVM) or native tissue repair.
Methods
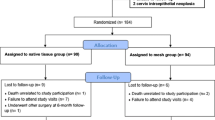
Prospective, randomized, multicenter study conducted between April 2005 and December 2009 comparing anterior colporrhaphy with trans-obturator vaginal mesh (Pelvitex/Ugytex®, Sofradim, Trevoux, France) for the treatment of anterior vaginal wall prolapse. The primary endpoint was functional recurrence rate 5–8 years after surgery. Secondary endpoints consisted of anatomical results, mesh-related morbidity and patient satisfaction measured through validated questionnaires.
Results
Of the 147 women originally included, 75 (51%) were successfully re-contacted a median of 7 years after the initial surgery. The primary outcome, subjective recurrence of prolapse, was similar between the TVM and the anterior colporrhaphy groups (31 vs 34% respectively). Anatomical recurrence was less likely in the TVM group (67 vs 24%, p = 0.004). Mesh exposure occurred in 4 of the 39 patients (13%) during follow-up, 2 of which had a surgical reintervention. Reintervention for prolapse took place in 7 patients (9%).
Conclusion
Seven-year follow-up showed similar functional outcomes for mesh and native tissue repair in anterior vaginal wall prolapse. TVM did not reduce repeat surgery in the long term; it did, however, reduce anatomical recurrence. Mesh exposure rates were relatively high, but no difference in outcome of pain or dyspareunia was noted.

Similar content being viewed by others
References
Wu JM, Matthews CA, Conover MM, Pate V, Jonsson Funk M. Lifetime risk of stress urinary incontinence or pelvic organ prolapse surgery. Obstet Gynecol. 2014;123(6):1201–6.
Smith FJ, Holman CD, Moorin RE, Tsokos N. Lifetime risk of undergoing surgery for pelvic organ prolapse. Obstet Gynecol. 2010;116(5):1096–100.
Shah AD, Kohli N, Rajan SS, Hoyte L. The age distribution, rates, and types of surgery for pelvic organ prolapse in the USA. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19(3):421–8.
Vollebregt A, Fischer K, Gietelink D, van der Vaart CH. Primary surgical repair of anterior vaginal prolapse: a randomised trial comparing anatomical and functional outcome between anterior colporrhaphy and trocar-guided transobturator anterior mesh. BJOG. 2011;118(12):1518–27.
Diez-Itza I, Aizpitarte I, Becerro A. Risk factors for the recurrence of pelvic organ prolapse after vaginal surgery: a review at 5 years after surgery. Int Urogynecol J Pelvic Floor Dysfunct. 2007;18(11):1317–24.
Abed H, Rahn DD, Lowenstein L, et al. Incidence and management of graft erosion, wound granulation, and dyspareunia following vaginal prolapse repair with graft materials: a systematic review. Int Urogynecol J. 2011;22(7):789–98.
Health, C.f.D.a.R., Public Health Notifications (Medical Devices)—FDA Public Health Notification: Serious Complications Associated with Transvaginal Placement of Surgical Mesh in Repair of Pelvic Organ Prolapse and Stress Urinary Incontinence. 2011.
SCENIHR. Opinion on the safety of surgical meshes used in urogynecological surgery. 2015. https://ec.europa.eu/health/scientific_committees/emerging/docs/scenihr_o_049.pdf
Maher C, Feiner B, Baessler K, Christmann-Schmid C, Haya N, Brown J. Surgery for women with anterior compartment prolapse. Cochrane Database Syst Rev. 2016;11:Cd004014.
Cobb WS, Kercher KW, Heniford BT. The argument for lightweight polypropylene mesh in hernia repair. Surg Innov. 2005;12(1):63–9.
Klosterhalfen B, Junge K, Klinge U. The lightweight and large porous mesh concept for hernia repair. Expert Rev Med Devices. 2005;2(1):103–17.
Zinther NB, Wara P, Friis-Andersen H. Shrinkage of intraperitoneal onlay mesh in sheep: coated polyester mesh versus covered polypropylene mesh. Hernia. 2010;14(6):611–5.
de Tayrac R, Alves A, Therin M. Collagen-coated vs noncoated low-weight polypropylene meshes in a sheep model for vaginal surgery. A pilot study. Int Urogynecol J Pelvic Floor Dysfunct. 2007;18(5):513–20.
De Tayrac R, Cornille A, Eglin G, Guilbaud O, Mansoor A, Alonso S, Fernandez H. Comparison between trans-obturator trans-vaginal mesh and traditional anterior colporrhaphy in the treatment of anterior vaginal wall prolapse: results of a French RCT. Int Urogynecol J. 2013;24(10):1651–61.
Barber MD, Neubauer NL, Klein-Olarte V. Can we screen for pelvic organ prolapse without a physical examination in epidemiologic studies? Am J Obstet Gynecol. 2006;195(4):942–8.
De Tayrac R, Chauveaud-Lambling A, Fernandez D, Fernandez H. Quality of life instruments for women with pelvic organ prolapse. J Gynecol Obstet Biol Reprod (Paris). 2003;32(6):503–7.
Rogers RG, Coates KW, Kammerer-Doak D, Khalsa S, Qualls C. A short form of the pelvic organ prolapse/urinary incontinence sexual questionnaire (PISQ-12). Int Urogynecol J Pelvic Floor Dysfunct. 2003;14(3):164–8, discussion 168.
Bump RC, Mattiasson A, Bø K, et al. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol. 1996;175(1):10–7.
Haylen BT, Freeman RM, Swift SE, et al. An International Urogynecological Association (IUGA) / International Continence Society (ICS) joint terminology and classification of the complications related directly to the insertion of prostheses (meshes, implants, tapes) and grafts in female pelvic floor surgery. Int Urogynecol J Pelvic Floor Dysfunct. 2011;22(1):3–15.
Srikrishna S, Robinson D, Cardozo L. Validation of the patient global impression of improvement (PGI-I) for urogenital prolapse. Int Urogynecol J. 2010;21(5):523–8.
Geller EJ, Barbee ER, Wu JM, Loomis MJ, Visco AG. Validation of telephone administration of 2 condition-specific quality-of-life questionnaires. Am J Obstet Gynecol. 2007;197(6):632.e1–4.
Glazener CM, Breeman S, Elders A, et al. Mesh, graft, or standard repair for women having primary transvaginal anterior or posterior compartment prolapse surgery: two parallel-group, multicentre, randomised, controlled trials (PROSPECT). Lancet. 2017;389(10067):381–92.
Milani AL, Damoiseaux A, IntHout J, Kluivers KB, Withagen MIJ. Long-term outcome of vaginal mesh or native tissue in recurrent prolapse: a randomized controlled trial. Int Urogynecol J. 2018;29(6):847–58.
Heinonen P, Aaltonen R, Joronen K, Ala-Nissilä S. Long-term outcome after transvaginal mesh repair of pelvic organ prolapse. Int Urogynecol J. 2016;27(7):1069–74.
Pecheux O, Giraudet G, Drumez E, et al. Long-term (8.5 years) analysis of the type and rate of reoperation after transvaginal mesh repair (Prolift®) in 349 patients. Eur J Obstet Gynecol Reprod Biol. 2019;232:33–9.
Withagen MI, Vierhout ME, Hendriks JC, Kluivers KB, Milani AL. Risk factors for exposure, pain, and dyspareunia after tension-free vaginal mesh procedure. Obstet Gynecol. 2011;118(3):629–36.
Chughtai B, Barber MD, Mao J, Forde JC, Normand ST, Sedrakyan A. Association between the amount of vaginal mesh used with mesh erosions and repeated surgery after repairing pelvic organ prolapse and stress urinary incontinence. JAMA Surg. 2017;152(3):257–63.
Liang R, Abramowitch S, Knight K, et al. Vaginal degeneration following implantation of synthetic mesh with increased stiffness. BJOG. 2013;120(2):233–43.
Frankman EA, Alperin M, Sutkin G, Meyn L, Zyczynski HM. Mesh exposure and associated risk factors in women undergoing transvaginal prolapse repair with mesh. Obstet Gynecol Int. 2013;2013:926313.
Eilber KS, Alperin M, Khan A, et al. The role of the surgeon on outcomes of vaginal prolapse surgery with mesh. Female Pelvic Med Reconstr Surg. 2017;23(5):293–6.
Collinet P, Belot F, Debodinance P, Ha Duc E, Lucot JP, Cosson M. Transvaginal mesh technique for pelvic organ prolapse repair: mesh exposure management and risk factors. Int Urogynecol J Pelvic Floor Dysfunct. 2006;17(4):315–20.
Lee DM, Nazroo J, O’Connor DB, Blake M, Pendleton N. Sexual health and well-being among older men and women in England: findings from the English longitudinal study of ageing. Arch Sex Behav. 2016;45(1):133–44.
Bell S, Reissing ED, Henry LA, VanZuylen H. Sexual activity after 60: a systematic review of associated factors. Sex Med Rev. 2017;5(1):52–80.
Aponte MM, Rosenblum N. Repair of pelvic organ prolapse: what is the goal? Curr Urol Rep. 2014;15(2):385.
Barber MD, Brubaker L, Nygaard I, et al. Defining success after surgery for pelvic organ prolapse. Obstet Gynecol. 2009;114(3):600–9.
Weber AM, Abrams P, Brubaker L, et al. The standardization of terminology for researchers in female pelvic floor disorders. Int Urogynecol J Pelvic Floor Dysfunct. 2001;12(3):178–86.
Ou R, Xie XJ, Zimmern PE. Prolapse follow-up at 5 years or more: myth or reality? Urology. 2011;78(2):295–9.
Eilber KS, Alperin M, Khan A, et al. Outcomes of vaginal prolapse surgery among female Medicare beneficiaries: the role of apical support. Obstet Gynecol. 2013;122(5):981–7.
Abrams P, Andersson KE, Apostolidis A, et al. 6th International Consultation on Incontinence. Recommendations of the International Scientific Committee: evaluation and treatment of urinary incontinence, pelvic organ prolapse and faecal incontinence. Neurourol Urodyn. 2018;37(7):2271–2.
Acknowledgements
We would like to show our gratitude to our colleagues from the other participating centers: Dr. Nizar Aflak, Dr. Jérôme Blanchot, Dr. Pierre-Louis Broux, Dr. Olivier Guilbaud, Dr. Aslam Monsoor, Prof. Xavier Deffieux, Prof. Loïc Marpeau, Dr. Vincent Descheemaeker, Dr. Philippe Ferry, and Dr. Sandrine Campagne. We also wish to thank the members of the BESPIM for the data management and statistical analysis (especially Dr. Pascale Fabbro-Peray, methodologist and Stéphanie Salles, data manager), and Dr. Sarah Kabani (for English editing), Department of Biostatistics, Epidemiology, Public Health and Innovation in Methodology (BESPIM), Nîmes University Hospital, Nîmes, France.
Funding
This research was supported by the Nîmes University Hospital (Local Project 2013).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
R. de Tayrac is consultant for Boston Scientific, has had research funding from Sofradim-Covidien, Boston Scientific, and has accepted speaker’s fees from Boston Scientific, Coloplast, and American Medical Systems. G. Eglin has acted as a consultant for Sofradim. H. Fernandez is a consultant for American Medical Systems. L. Allègre, G. Callewaert, A. Cornille, O. Guilbaud, A. Mansoor, and S. Alonso have no conflicts of interest to declare.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Allègre, L., Callewaert, G., Alonso, S. et al. Long-term outcomes of a randomized controlled trial comparing trans-obturator vaginal mesh with native tissue repair in the treatment of anterior vaginal wall prolapse. Int Urogynecol J 31, 745–753 (2020). https://doi.org/10.1007/s00192-019-04073-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-019-04073-x